Communication
advertisement
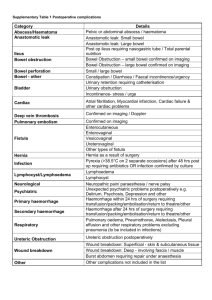
Bowel Obstruction in Cancer Patients Dr Fathi Azribi Consultant Medical Oncologist The James Cook University Hospital 19/04/2013 Bowel Obstruction in Cancer Patients • Ovarian cancer: 5%-51% • Gastrointestinal cancer: 10%-28% • Other cancers (breast, melanoma, sarcoma, lung…etc) • Poor prognosis Median survival 30-90 days Mercadante S. Palliative Medicine, 2009 Pasanisi F, Nutrition, 2001 Pameijer CR, Int J Gastrointest. Cancer 2005 Bais JMJ, J Gynecol Oncol 2002 Types of obstruction • Site: – Bowel level • Proximal BO: Upper GI &HBP Cancers • Distal BO: Colon & Ovarian Cancers – Obstruction level • One site • Multiple sites • Mechanism: – Mechanical: • Tumour • Non malignant (adhesions, strictures, desmoplastic reactions) – Functional: • Paraneoplastic • Drugs • Onset: – Acute…complete – Sub acute….partial – Intermittent Symptoms and signs Severity and order vary: • Symptoms: – – – – Nausea & vomiting Bloating & fullness Pain Constipation • Signs – Abdominal distension – Bowel sounds: active & tinkling vs. silent – Signs of dehydration – Perforation, peritonitic & toxic Approach to management • History and clinical examination • Initial treatment: hydration • Imaging • Direct discussion (with surgeons)… MDT • Specialist Palliative Care Team Investigations • Imaging: – Plain x ray useful but low accuracy – Barium/gastrograffin studies hardly used – CT scan specificity 100% sensitivity 94% • Other investigation: FBC, U& Es, LFT, tumour markers….etc Individualized approach Surgery PS Comorbidities Nutritional status Tumour type Tumour burden Diffuse carcinomatosis Extensive prior anticancer therapy Previous surgery Single vs. multilevel Expected survival Patient’s choice NG tubes Stenting Venting gastrostomy Medical therapy Individualized approach • 68 years old lady • Stage IIIC ovarian carcinoma presented with bowel obstruction • Defunctioning ileostomy…North Tees Hospital October 2009 • 4 cycles of Carboplatin and Paclitaxel chemotherapy • Laparotomy BSO, omental biopsy, reversal of ileostomy Feb 2010 followed by 2 more cycles of chemotherapy • Disease progression with several lines of chemotherapy • 8/4/2013 reasonably well and will have some more chemotherapy for further progression Individualized approach • 47 years old lady • Stage 4 primary peritoneal carcinoma July 2010 • 6 cycles of Carboplatin and Paclitaxel chemotherapy completed December 2010 with good response • Disease progression April 2011, treated with 6 cycles of Caelyx completed October 2011 • Small bowel obstruction Feb 12, laparotomy and loop ileostomy….good symptomatic improvement and reasonable quality of life for a few months • Died August 2012 Individualized approach • 35 year old lady • Low grade ovarian carcinoma • Diagnostic laparoscopy: extensive disease, drainage of ascites and intrabdominal biopsies November 2011 • Received 1 cycle of carboplatin and paclitaxel chemotherapy on December 2011 • High small bowel obstruction Jan 2012 due to disease progression • Best supportive care • Discharged home ( PPC) • Died 2 weeks later Surgery? Who is for surgery? • Patients should be carefully selected • Careful consideration of prognostic factors (e.g. PS, tumour burden) and the expected outcome (symptom control, quality of life. Survival) • A thorough discussion among the health professionals • Patient’s expectations and wishes should be explored Surgery? • What surgery – Resection/debulking….primary anastomosis – Bypass surgery – Defunctioning colostomy/ileostomy Chemotherapy? • Unlikely to help as a sole modality • It depends: – Tumour type – Extent of disease – Type of obstruction – Heavily pre-treated – Previous PS – Co-morbidities Gastric & colonic stenting • Advantages: – Alternative option for patients unfit for surgery or do not want to have surgery – A quick fix while waiting for surgery – High success rate for gastric outlet and left sided colonic obstruction – Quicker recovery & shorter hospital stay • Less successful: – Rapidly progressive cancers – Multifocal bowel obstruction – Diffuse carcinomatosis NG tubes and PEG • NG tube: – Could be useful for a quick relief of gastric distension and improve nausea and vomiting – Not recommended for long term use (nose and throat pain, sinusitis, abscess formation, erosion of nasal cartilage, aspiration oesophageal erosion.. etc.) • PEG: – Effective symptom relief – Technically easy procedure – Easily handling at home and at terminal stages – However, not very popular! Medical therapy • Pain • Nausea/vomiting • Gastrointestinal secretions Medical therapy • Pain – Continuous • Opiates: morphine, oxycodone, fentanyl – Can aggravate colic – Constipation – Nausea/vomiting • Other analgesics – Colic • Hyoscine butylbromide (Buscopan) Medical therapy • Nausea/vomiting – Cyclizine: safe when complete obstruction – Haloperidol: less sedation, good for nausea – levomepromazine – Metclopramide: antiemetic and gastroprokinteic • Contraindicated: complete obstruction • Caution: colic • Useful: functional, partial obstruction – Dexamethasone – Ondansetron Medical therapy • Gastrointestinal secretions: – Anticholinergic: Hyoscine butylbromide – Somatostatin analogues: Octreotide • Combination therapy – Almost always needed typical combination: analgesic + antiemetic + corticosteroid + octreotide – Syringe driver Total parental nutrition (TPN) • Not recommended for the majority of patients with malignant obstruction – Advanced malignancy with poor prognosis – High rate of complications (infection, electrolyte disturbance, thrombosis…etc) • May be considered for a selected patients – Neoadjuvant setting – Low volume disease, high response rate to chemotherapy and expected long survival Continued care • Patients can eat - as long as it is tolerated • Mouth care, ice chips, lubrication to the lips, and sips of fluid are all helpful to reduce mouth dryness and sense of thirst • Intravenous fluids: usually difficult discussion – Long-term and excessive use is not recommended – Discontinue once symptoms controlled and no further intervention is planned – Patients and family should be well informed and involved in decision-making Summary • Malignant bowel obstruction needs: – individualised approach – Team work (oncology, surgery, radiology, specialist palliative care team and other health care professionals) • Communication: – Treatment options, expectations & limitations, discharge plan and preferred place of care….the earlier you discuss with patient and family, the better coping and the less of unnecessary anxiety and fear of uncertainty