Peds and IVs - group 11 powerpoint
advertisement
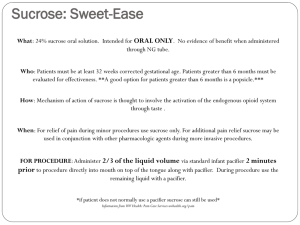
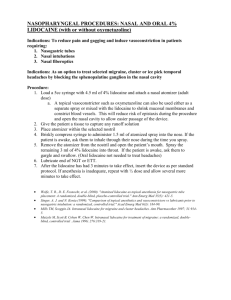
Best Practice For IV Insertion In Infants And Children Columbus State University Team: Peds and IVs • • • • • • Justin Banister Michael Chamberlain Jacob Chauvin Eric Hall Kirsten Joiner Darrell Mackenzie Purpose • To determine the best practice for the use of a numbing device in reducing pain and anxiety of infants and children during peripheral IV insertion. http://mystuffspace.com/graphic/happy-baby.jpg Significance • Reduction of pain and anxiety in pediatric patients • Increase first attempt IV insertion success rates • Conserve time, money, and resources http://www.skywriting.net PICO(T) Clinical Question • • • • P: Infants and Children I: Pain/Anxiety reducing interventions C: No intervention O: Decreased pain and anxiety during IV insertion Interventions for Pain/Anxiety: • • • • • • • No Intervention Distractions Saline Wheal ELA Max Cream Sub-Q Lidocaine Vapocoolant Spray Jet Lidocaine Device http://www.thrivingpets.com http://4.bp.blogspot.com The Use of No Intervention • It will be the child and/or caregiver’s choice as to whether the patient will recieve any type of intervention for the insertion of the IV. http://www.frickart.org Distractions • Bubbles • Pinwheels • Music http://www.picturesofbabies.net/ http://www.ourwebpage.org/aircastles andslides/bubbles_2zillions.jpg Saline Wheal • Bacteriostatic Normal Saline (BNS) compared to 1% lidocaine and no anesthetic • 27-gauge needle was used to intradermally inject 0.1 to 0.2 mL of BNS and 1% lidocaine • 1 minute after the injection of the compound, the IV was inserted into the vein. •A modified visual analog scale was used for the children to rate their preprocedural anxiety, pain with intradermal injection, and pain with cannulation (Fein, Boardman, Stevenson, & Selbst, 1998) Saline Wheal •Pain Scale: • No anesthesia: 41.0 • BNS: 9.0 • 1% Lidocaine: 10.0 •Significance: •p = 0.006 - BNS vs no anesthesia •p = 0.04 - lidocaine vs no anesthesia •p = 0.57 - BNS vs lidocaine (Fein, Boardman, Stevenson, & Selbst, 1998) ELA-Max Cream • A 4% lidocaine cream that features a liposomal delivery system and is administered topically after disinfection of insertion site. • 2.5 g applied to the skin and covered with an occlusive dressing (Tegaderm) overlying the IV site 30 minutes before IV insertion • It has been shown to effectively reduce pain and distress associated with venipuncture in children (Luhmann, Hurt, Shootman, & Kennedy, 2004) ELA-Max Cream Benefits: • No occlusive dressing needed per ELA-Max packaging • Decreases pain and distress of IV insertion Complications: • Time constraints • Child could touch and place cream in mouth • If not covered by transparent dressing Limitations: • Study indicated a limitation was the skill to apply cream • Non-toxic and over the counter, but we discourage ingesting (Luhmann, Hurt, Shootman, & Kennedy, 2004) Sub-Q Lidocaine • 0.1 to 0.2 ml 1% buffered lidocaine administered subcutaneously with a 30-gauge needle 5 minutes before IV insertion • Significantly reduces distress associated with peripheral intravenous catheter insertion in children http://imghost.indiamart.com (Luhmann, Hurt, Shootman, & Kennedy, 2004) Sub-Q Lidocaine Complications: • Additional stick for the patient • Skill of sub-q injection http://www.travmed.com (Luhmann, Hurt, Shootman, & Kennedy, 2004) ELA-Max vs Sub-Q Lidocaine • No significant difference in pain scores between the two methods: • Pain: p = 0.19 • Anxiety: p = 0.18 (Luhmann, Hurt, Shootman, & Kennedy, 2004) EMLA-Max vs Sub-Q Lidocaine vs Intradermal Lidocaine • • • • Eutetic Mixture of Local Anesthetics 4 European studies EMLA comparable to Sub-Q lidocaine EMLA less effective than intradermal lidocaine (Delisa, Gans, & Walsh, 2005) Vapocoolant Spray • • • Sprayed directly onto skin from 3-9 inches away, or can be used on a cotton ball and applied with forceps. Pain was reduced from a mean score of 56 - 37 per color visual analog scale, p < 0.01 It was not specified in the study if disinfection of the site was performed prior to or after the vapocoolant spray was applied (Farion, Splinter, Newbook, Gaboury, Splinter, 2008) gebauerspainease.com Vapocoolant Spray • 50% of patients receiving vapocoolant spray reported no pain compared to 32% in placebo group, p = 0.01 • 85% first attempt cannulation success vs. 62.5% in placebo group, p = 0.02 - Child life specialists ratings favored vapocoolant vs. placebo emedicine.medscape.com (Farion, Splinter, Newbook, Gaboury, Splinter, 2008) Vapocoolant Spray - The study did not indicate the specific mechanism of action that increased successful first attempts. It is assumed that a reduction in pain, anxiety, and movement of the patient contributed to this. - Nurses noticed an improvement of technical ease when using the vapocoolant spray vs. placebo - Results: Vapocoolant spray effectively reduced pain and increased first attempt cannulation success rates in pediatric patients (Farion, Splinter, Newhook, Gaboury, Splinter, 2008) Vapocoolant Spray Risks: • Burning sensation produced when cooling • Tissue Necrosis after 10 seconds Benefits: • Reduction in pain and associated anxiety • Non-flammable, non-toxic, and Ozone friendly, works instantly, costs around 50 cents per use • Safe to use on pediatric patients gebauerspainease.com (Farion, Splinter, Newhook, Gaboury, Splinter, 2008) Jet Lidocaine Device • It does not contain any sharp needles, thus reducing the risk of needle-stick injuries, and can be safely discarded in to a normal waste container • Delivers medication into the epidermis in 0.2 seconds and takes approximately 1 minute to fully work http://onlinelibrary.wiley.com/doi/10.1111/j.15532712.2009.00401.x/full (Auerbach, Tunik, & Mojica, 2009) Jet Lidocaine Device • Study has shown that it provides greater anesthesia than that of ELA-Max • The J-Tip jet device is a cost effective device at approximately $2/device; 1 use per device • P<0.001 – Limitations (Spanos, Booth, Koenig, Sikes, Gracely, & Kim, 2008) Conclusion • Recommend: – Jet Lidocaine for efficacy – Bacteriostatic normal saline for “biggest bang for the buck” Guideline procedure • • • • A nurse reviews the order. Select a suitable vein Disinfect site per hospital protocol A numbing agent will be selected by the patient and/or caregiver and applied per hospital protocol. Guideline procedure • • • Jet Lidocaine • 0.2 mL of buffered 1% lidocaine injected via jet device at least 60 seconds before IV insertion attempt ELA-Max Cream • Applied to the skin and occluded with Tegaderm 30 minutes before peripheral IV insertion attempt Sub-q Lidocaine • 30-gauge needle to subcutaneously inject 0.2 mL of buffered 1% lidocaine 5 minutes before IV insertion attempt • Vapocoolant Spray • Administer Vapocoolant spray to IV insertion site within 60 seconds before IV insertion attempt • Bacteriostatic normal saline (BNS) • 27-gauge needle is used to inject 0.1 to 0.2 mL intradermally of BNS 1 minute before IV insertion attempt • Insert IV per hospital protocol Resources Auerbach, M, Tunik, M, & Mojica, M. (2009). A Randomized, double-blind controlled study of jet lidocaine compared to jet placebo for pain relief in children undergoing needle insertion in the emergency department. Academic Emergency Medicine, 16 (5), 388-393. Delisa, J., Gans, B., & Walsh, N. (2005). Physical medicine and rehabilitation: Principles and practice, volume 1. Philadelphia, PA: Lippincott, Williams, & Wilkins. Farion, K, J., Splinter, K, L., Newhook, K., Gaboury, I., & Splinter, W, M. (2008). The effect of vapocoolant spray on pain due to intravenous cannulation in children: a randomized controlled trial. Canadian Medical Association Journal, 179(1):31-6. Fein J. A., Boardman C. R., Stevenson S., & Selbst S. M. (1998). Saline with benzyl alcohol as intradermal anesthesia for intravenous line placement in children. Pediatric Emergency Care, 14(2), 119-122. Retrieved from http://journals.lww.com/peconline/pages/default.aspx Resources Larsen, P., Eldridge, D., Brinkley, J., Newton, D., Goff, D., Hartzog, T., et al. (2010). Pediatric peripheral intravenous access: does nursing experience and competence really make a difference?. Journal of Infusion Nursing, 33(4), 226-235. Luhmann, J., Hurt, S., Shootman, M., & Kennedy, R. (2004). A Comparison of buffered lidocaine versus ELA-Max before peripheral intravenous catheter insertions in children. Pediatrics, 113(3 Part 1), e217-20. Spanos, S., Booth, R., Koenig, H., Sikes, K., Gracely, E., & Kim, I. (2008). Jet injection of 1% buffered lidocaine versus topical ELA-Max for anesthesia before peripheral intravenous catheterization in children: a randomized controlled trial. Pediatric Emergency Care, 24(8), 511-515. Windle, P., Kwan, M., Warwick, H., Sibayan, A., Espiritu, C., & Vergara, J. (2006). Comparison of bacteriostatic normal saline and lidocaine used as intradermal anesthesia for the placement of intravenous lines. Journal of PeriAnesthesia Nursing, 21(4), 251-258. Thank http://wawmptacouncil.info/ http://www.cs.cmu.edu/~christel/MM_MSEC/Ozarks /Missouri.html You!!