Preterm labor and PROM
advertisement
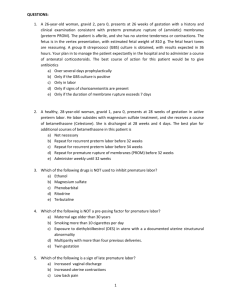
Preterm labor and PROM Dr. Wisit Woranitat Preterm labor • What is preterm labor • How dose labor start • What can happen if my baby is born too early • What factors increase the risk of preterm labor • What are the signs and symptoms of preterm labor • How can preterm labor be diagnosed Preterm labor • If I am at risk of preterm labor, what can I do to decrease the risk • How do I monitor myself for contraction • What medications are used to slow or stop per term • What are the special needs of preterm babies What is preterm labor • The labor begin start before 37 weeks • About 1 in 10 babies born in USA • 75% of neonatal mortality • 50% of the long term neurologic impairment in children How does labor start • Regular uterine contraction • Progression of cervix • Effacement • Dilatation • Hormones produced by uterus and placenta What can happen if my baby is born too early • Newborn death • Eyes • Ears • Breathing • Nervous system Perinatal Morbidity Pulmonary- RDS bronchopulmonary dysplasia Cardiovascular: PDA, persistent fetal circulation CNS: IVH, cerebral palsy, seizures, sensory deficits GI: NEC Metabolic: hypoglycemia, hypocalcemia, jaundice Perinatal morbidity Infections: GBS, E. Coli SIDS Psychosocial:> prevalence of child abuse • 50% Preterm labor Pathogenesis • 30% Preterm premature rupture of the membranes • Pathogenic processes • Activation of the maternal or fetal hypothalamic pituitary axis • Infection What factors increase the risk of preterm labor Previous History Smoking Cocaine use & DES Multiple pregnancy Abn Cx & Ut Surgery Bleeding 2 half Hydramnios Infection Poor ANC What are the signs and symptoms of preterm labor Vaginal discharge Pelvic&Abd pressure Backache Abd cramps Ut contraction PROM How can preterm labor be diagnosed • Cervical change • Regular contraction • Ultrasonography. ( Cx length ) • Fetal fibronectin • Fetal mornitoring Biologic markers for predicting preterm birth • Cervical length measurement- many studies have confirmed an association with cervical shortening and preterm delivery. When combined with positive fetal fibronectin and length less than 2.5 cm, this is a strong predictor of preterm delivery Biologic markers for predicting preterm birth • Fetal fibronectin- need intact membranes, less than 3 cm dilated, not useful before 24 weeks or after 34 weeks 6 days • Negative fetal fibronectin gives about a 95% chance of the pregnancy continuing 14 days or more. A positive test is not as predictive. What can I do to decrease the risk of preterm labor • Early ANC • Test or investigation • Progesterone • Limited and control the risk How do I monitor myself for contraction • Monitor for sign of uterine activity • 4 times in 20 minutes • 8 times in 60 minute • Vaginal discharge • PROM What medications are used to slow or stop • Tocolysis agents preterm Bricanyl • NSAIDS • Corticosteroid • Anti-biotic agent Calcium Chanel blocker • Oxytocin antagonist Assessment of patients in preterm labor Labs-CBC, UA +/- culture, electrolytes Sterile speculum exam obtaining cultures for group B strep, BV, GC, Chlamydia, obtain fetal fibronectin Cervical length measurement The last thing is the cervical digital exam What are the special needs of preterm babies • NICU • Breathe • Eat • Keep warm • Other health problem Premature rupture of membrane • Definition • Incidence • Diagnosis • Risk factors • Management Definition Premature rupture of membranes (PROM) Rupture of the chorioamnionic membrane prior to the onset of labor at any stage of gestation Preterm premature rupture of membranes (PPROM) PROM prior to 37-wk. gestation Incidence PROM – 12% of all pregnancies PROM – 8% term pregnancies PPROM – 30% of preterm deliveries History Diagnosis “Gush” of fluid Steady leakage of small amounts of fluid Physical Sterile vaginal speculum exam Minimize digital examination of cervix, regardless of gestational age, to avoid risk of ascending infection/amnionitis Assess cervical dilation and length Obtain cervical cultures (Gonorrhea, Chlamydia) Obtain amniotic fluid samples Findings Pooling of amniotic fluid in posterior vaginal fornix Fluid per cervical os Diagnosis • Test or investigation • Nitrazine test • Fern test • Nine blue test • Ultrasound • Indigo-carmine Amnioinfusion Nitrazine test Fluid from vaginal exam placed on strip of nitrazine paper Paper turns blue in presence of alkaline (pH > 7.1) amniotic fluid Fern test Fluid from vaginal exam placed on slide and allowed to dry Amniotic fluid narrow fern vs. cervical mucus broad fern Nile blue tests • >32 wks. Fetal fat cell can discover in amniotic fluid • Strained with Nile blue sulphate. Become to red color • Fetal Fibronectin (AmniSure) Newer test • Point of Care test • Cost-up to $50 each • Sensitivity-98.798.9% • Specificity-87.5100% • Awaiting further testing prior to recommendations Ultrasound Assess amniotic fluid level and compatibility with PROM Indigo-carmine Amnioinfusion Ultrasound guided indigo carmine dye amnioinfusion (“Blue tap”) Observe for passage of blue fluid from vagina Risk factor of PROM Prior PROM or PPROM Prior preterm delivery Multiple gestation Polyhydramnios Incompetent cervix Vaginal/Cervical Infection Gonorrhea, Chlamydia, GBS, S. Aureus Antepartum bleeding (threatened abortion) Smoking Poor nutrition Effect to mother and fetus • Feto-maternal infection • Placenta abruptio • Premature infant: 30% - 40% of premature labour is associated with premature rupture of membrane • Cord prolapse, cord compression • Poor fetal lung development and fetal compression syndrome Management PROM at term: (1) Awaiting the onset of spontaneous labor for 12-24h (2) Termination of pregnancy after 24 hours PROM before term Termination of pregnancy (1) Evidence of fetal pulmonary maturation (2) Evidence of intrauterine infection Expectant therapy Indication : (1) Evidence of fetal pulmonary immaturation (2) Without evidence of intrauterine infection Management: (1)To enhance fetal pulmonary maturation (2) Antibiotic Management: Rationale Antibiotics Prolong latency period Prophylaxis of GBS in neonate Prevention of maternal chorioamnionitis and neonatal sepsis Corticosteroids Enhance fetal lung maturity Decrease risk of RDS, IVH, and necrotizing enterocolitis Tocolytics Delay delivery to allow administration of corticosteroids Controversial, randomized trials have shown no pregnancy prolongation Management: Surveillance Maternal: Monitor for signs of infection Temperature Maternal heart rate Fetal heart rate Uterine tenderness Contractions Management: Surveillance Fetal: Monitor for fetal well-being Kick counts Nonstress tests (NST’s) Biophysical profile (BPP) Immediate Delivery Intrauterine infection Abruptio placenta Repetitive fetal heart rate decelerations Cord prolapse. Thank you For your attention