WHAT IS PARAPLEGIA?
PARALYSIS OF LOWER PART OF
BODY,COMMONLY AFFECTING BOTH
LEGS AND OFTEN INTERNAL ORGANS
BELOW WAIST.
ETIOLOGY
DIVIDED INTO 2 TYPES
DUE TO UPPER MOTOR NEURON
LESION
DUE TO LOWER MOTOR NEURON
LESION
UMN LESIONS
SPINAL LESIONS (common)
Spinal cord compression( Pott’s disease,disc prolapse
or fracture, tumors,epidural abscess,cervical
spondylosis etc)
VASCULAR
Hemorrhage, Infarction
SYSTEMIC DEGENERATION OF TRACTS
Multiple sclerosis, MND, Sub acute combined
degeneration of cord.
INFECTION
Transverse myelitis, Neurosyphilis
UMN LESIONS
CEREBRAL LESIONS (uncommon)
Thrombosis of superior sagital sinus
Tumor of falx-cerebri
Hydrocephalus
LMN LESIONS
Anterior horn cells
Poliomyelitis, Motor neuron disease
Peripheral nerve
Peripheral neuropathy
Neuromuscular junction
Myasthenia gravis
Muscles
Muscular dystrophies
SPINAL CORD COMPRESSION
It may be acute with trauma,metastasis
or
Arterial occlusion or it may be slow
developing over weeks as in Pott’s
disease,cervical spondylosis etc.
POTT’S DISEASE
TB of spine often involves two or more
adjacent vertebral bodies. Lower
thoracic and upper lumber vertebrae
are commonly involved.Intervertebral
disc is also destroyed. With advanced
disease paravertebral cold abscess ,
gibbus formation and PARAPLEGIA
occur.
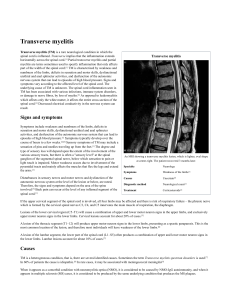
TRANSVERSE MYELITIS
It is an acute or subacute inflammation
of spinal cord occuring after infection or
recent vaccination. Many agents like
influenza,measles,CMV,EBV and
mycoplasma have been implicated.
Guillain Barre Syndrome
Acute inflammatory or post-infective
demyelinating polyneuropathy.
Develops 1-3 weeks after
respiratoryinfection or diarrhea in
>70% cases.
Ascending polyneuropathy.
MOTOR NEURON DISEASE
Progressive degenerative disorder of upper
and lower motor neurons in spinal
cord,cranial motor neurons and pyramidal
neurons in motor cortex.
Cause- unknown.
Patterns
Progressive bulbar palsy
Progressive muscular atrophy
Amytrophic lateral sclerosis.
SUBACUTE COMBINED
DEGENERATION
OF SPINAL CORD
Syndrome of combined spinal cord and
peripheral nerve damage
cause: Vit.B12 deficinency
Changes start in posterior columnn
(affecting vibration and position sense)
then involve lateral column(pyramidal
tracts)
MYASTHENIA GRAVIS
Acquired autoimmune disorder of NMJ.
Causes skeletal muscle fatigubility and
weakness, esp of proximal limb
muscles,ocular anb bulbar muscles.
DUCHENNE’S MUSCULAR
DYSTROPHY
X-linked recessive disorder
Deficiency of protein dystrophin in
muscles.
Symptoms start in childhood,become
severe in adolescence and death occurs
by age 20 years.
MANAGEMENT OF PARAPLEGIA
HISTORY
EXAMINATION
INVESTIGATIONS
TREATMENT
HISTORY
AGE AND SEX
Young age: Inherited disorders,muscle dis.,infections
Old age: malignancies r common.
DURATION
ACUTE:GBS,transverse myelitis, cord compression.
CHRONIC:MND,polyneuropathies,muscle dis.
SPHINCTER DISTURBANCES (INITIALLY
URGENCY OR HESITENCY OF MICTURATION,THEN
URINARY RETENTION)
Seen in UMN lesions.
HISTORY
SENSORY SYMPTOMS
Numbness,tingling and hyperesthesias in neuropathy.
ROOT PAIN
In cord compression.
BACKACHE
In cord compression,transverse myelitis.
HEADACHE,VOMITING
Intracranial lesions
PRECEDING FEVER,URTI
In GBS
EXAMINATION
MOTOR SYSTEM
FEATURES
Muscle waisting
Muscle tone
Power
Deep reflexes
Superficial
reflex
Planters
Fasciculations
UMNL LMNL
absent present
+++
_
absent present
absent present
SENSORY SYSTEM
Sharp sensory level in transverse myelitis
differentiates it from GBS.
Neuropathy:glove and stocking
distribution.
Romberg sign +ve if posterior column is
involved.
SIGNS OF SPINAL CORD
COMPRESSION
CERVICAL,ABOVE C5
UMN signs and sensory loss in all 4 limbs
CERVICAL,C5 TO T1
LMNsigns and segmental sensory loss in arms,and
UMN signs in legs
THORACIC CORD
Spastic paraplegia with a sensory level on trunk.
CONUS MEDULLARIS
Sensory loss in sacral area and extensor plantar
response
CAUDA EQUINA
LMN signs in lower limbs.
EXAMINATION
EXAMINATION OF SPINE
For deformity and tenderness.
SPHINCTERS:Look for incontinence or
retention of urine or faeces.
OTHER FEATURES:
Anemia-B12 deficiency
Stiff neck in cervical spondylosis
Site of malignancy.
INVESTIGATIONS
X-RAY SPINE:
May show collapse or erosion of
vertebrae,herniated interverteberal
disc,mets.,# or dislocation of vertebra
etc.
MRI:
Investigation of choice
CT SCAN
BLOOD CP:
Megaloblastic anemia in subacute
combined degeneration of spinal
cord.
INVESTIGATIONS
CSF examination:
Inflammatory lesions, both cells and proteins
are increased.
In malignancy,malignant cells may be present.
In transverse myelitis ,proteins are increased
and upto 50 lymphocytes/cmm are present.
In MS,monoclonal IgG is increased.
In GBS,protein cell dissociation is seen.
INVESTIGATIONS
MYELOGRAPHY:
Site of cord compression is demonstrated.
NERVE CONDUCTION STUDIES:
Helpful in diagnosis of neuropathies.
FUNDOSCOPY:
For papilloedema due to intracranial tumor
or MS.
BONE SCAN:
Mets and inflammatory vertebral lesions r
detected.
TREATMENT
GENERAL MEASURES
SKIN CARE:
Change posture every 2-4 hrly to avoid bed
sores.
Keep skin dry and clean.
BLADDER CARE:
CATHETERIZATION for urinary retention.
BOWEL CARE:
Avoid constipation by suitable diet and
laxatives.
TREATMENT
PREVENTION OF CONTRACTURES
By regular passive movements.
REHABILITATION
By using wheel chair,standing
frames,vocational training etc.
SPECIFIC TREATMENT
POTT’S DISEASE
Immobilization
ATT
Surgery:Anterior transthoracic
decompression.
TRANSVERSE MYELITIS
Glucocorticiods are given.Initially I/V
methylprednisolone,then oral prednisolone.
TREATMENT
MND
Symptomatic T/M like
physiotherapy,walking aids,splints and
speech therapy.
Glutamate antagonist,RILUZOLE ?
SUBACUTE COMBINED
SPINALCORD DEGENERATION
Injection vit.B12 1000 ug I/M daily for
7-10 days,then weekly for a month and
then monthly for whole life.
TREATMENT
GBS
Plasma pharesis(effective only in first 2
weeks)
i/v immunoglobulins(2g/kg in 5 days)
No role of steriods.
SPINAL CORD TUMORS
Radiotherapy
Surgical decompression.
COMPLICATIONS
BEDSORES
BOWEL AND BLADDER INCONTINENCE
DVT
PULMONARY EMBOLISM
PSYCHIATRIC LAYOUT
HYPOSTATIC PNEUMONIA
DISEASE RELATED COMLICATIONS
THANK YOU