MRI in white matter diseases - c
Journal club Presentation
Presented by:
Dept of Radiology & Imaging, MMCH.
Chairperson
Dr. Sankar Narayan Dey.
Asst Prof. & Head.
Dept of Radiology & Imaging
Speaker: Dr. Farzana Sultana.
MD (Thesis part ) student.
Today’s Topics:
MRI in white matter diseases - clinico radiological correlation
BN Lakhkar, M Aggarwal, JR John
Department of Radio Diagnosis and Imaging, Kasturba Medical
College, Manipal, Karnataka, India
Indian J Radio Imaing /2002 / Volume : 12 / Issue : 1 .
Abstract
•The purpose of this study is to evaluate the role of MRI as an investigative modality in white matter diseases and to document its value in early diagnosis and management.
•Studying the MR appearances of various white matter diseases encountered in our hospital with special reference to multiple sclerosis and correlating it with the clinical presentation.
•Demyelinating foci were demonstrated with a high degree of accuracy on MR as prolonged
T1 and T2 relaxation times, the site of the lesion varying in different disorders.
•Multiple sclerosis accounted for the majority of cases (37.5%) followed by acute disseminated encephalomyelitis (15%).
•Other causes like infections, toxic causes, periventricular leukomalacia and leukodystrophies.
•MRI due to its excellent gray-white matter resolution is very sensitive in detecting subtle demyelination, the sensitivity being still further enhanced by FLAIR (Fluid attenuation inversion recovery) sequences.
•The present study concludes that MRI, in correlation with the clinical signs and symptoms is an ideal modality in early diagnosis of white matter diseases and aids in the early institution of therapy so that the curable conditions among them can be treated.
Introduction
• With the introduction of MRI and increasing awareness of the disease, more and more cases of multiple sclerosis and other demyelinating diseases are being diagnosed.
• Many of these diseases if detected early can be cured and MRI plays a vital role in its early diagnosis.
• MRI has virtually replaced all other imaging modalities including CT in the evaluation of white matter diseases due to its excellent graywhite matter resolution and multiplanar imaging capability.
• Simultaneous imaging of spinal cord and orbits can also be done by
MRI.
• In this article, the authors report their experience with MR in 40 patients with a clinical diagnosis of demyelination and evaluate its role in the diagnosis of these diseases.
Materials
• Forty patients with a strong clinical suspicion of demyelinating disorder were evaluated by MRI in a prospective study period of two years.
• Among them 22 were men and 18 were women.
• All the patients with age related vascular causes of demyelination were excluded from the study group.
Methods
• The MRI scan was performed using a 0.5 Tesla (Signa Contour, GE) scanner using standard head coil.
• Slice thickness of 5mm.
• T1(TR/TE-440/10ms), T2 (TR/TE-2240/90ms) and FLAIR(TR/TE-
10,000/94ms) images were taken in multiple planes with or without
Gadolinium.
• All patients were followed up to reach a therapeutic/biopsy diagnosis.
The symptomatic response with medical therapy was noted which helped in the retrospective confirmation of the diagnosis. Brain biopsy was not done in any of the cases.
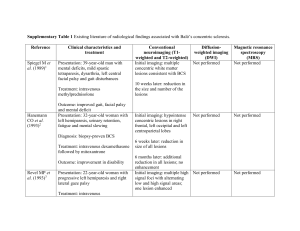
Result
Distribution of white matter diseases
Table - 1
Multiple sclerosis (MS)
Number ,age & gender:15 cases out of 40, the third decade of life with a definite female preponderance (M:F - 1:2).
Mean age of onset was 27.6 years with range 23.9 - 35.2 years in males.
Symptom:
Imaging:
•
MR revealed multiple lesions confined to the white matter, appearing hypointense on T1W and hyperintense on T2W images.
•
In all patients, more than three lesions were seen. The lesions varied in size with most of the lesions being less than 1 cm.
• The commonest site of involvement in MS was found to be the periventricular area (80%) with the perivenular extension (Dawson's fingers) being specific for the disease
• Lesions at the calloso-septal interface are also characteristic with atrophy of the corpus callosum.
• Brain stem and cerebellar involvement were seen in 40% and 6.6% respectively.
• Spinal cord and optic nerve involvement were noted in 20% each.
• No mass effect or perifocal edema.
• Contrast administration showed enhancement in only four cases which was of both solid and ring type of enhancement
Acute disseminated encephalomyelitis (ADEM)
Number & age:
6 cases out of 40, age range were 6-55years, 4 were adult & 2 were children.
Sypmtoms:
All having a history of fever prior to the onset of clinical symptoms, symptoms were altered consciousness (50%) followed by motor symptoms and urinary retention (33.3% each).
Imaging:
• Commonly located in the cerebral white matter (83.3%) with asymmetric and patchy involvement followed by brain stem involvement (50%).
• Spinal cord and cerebellar lesion were noted in one patient each. Thalamic involvement was seen in two cases and added to the specificity of diagnosis.
Prognosis:
On steroid therapy, majority showed clinical improvement
Herpes simplex encephalitis (HSE)
Number, age and sex:
5 cases out of 40,all were females & under 20-30 years of age.
Symptoms:
• Altered sensorium and fever (80%) followed by seizures (40%).
Imaging:
• T1 hypo and T2-FLAIR hyperintensity.
• Characteristically involving the temporal lobes extending into the basifrontal areas in 60%.
• Contrast enhancement was seen in only one of the patients being patchy in appearance and hemorrhage was not noted.
• Four cases showed bilateral asymmetric involvement, the left temporal lobe being affected more than the right in 60%
• Unilateral involvement was seen in only one case.
Prognosis:
All cases showed prompt recovery with acyclovir therapy.
Progressive multifocal leukoencephalopathy (PML)
Number,age & sex :
• 2 cases out of 40 .
• Mean age was 29 yrs.
• Both were HIV positive males
Sign & Symptoms :
• Hemiparesis
• Cerebellar signs.
Imaging:
• Well defined non enhancing hypointense lesions on T1WI one showing supratentorial (frontal white matter) and the other posterior fossa (pons and cerebellum) involvement
• No mass effect or cortical atrophy.
Central pontine myelinolysis (CPM)
Number, age & sex:
• 4 cases out of 40, age range was 24 to 60 years.
• All patients were males
Predisposing factors:
• Hyponatremia
• Alcoholism
Imaging:
• All the four patients showed extra pontine involvement in addition to the characteristic involvement of central pons.
Radiation induced white matter demyelination
• There was one patient with optico-chiasmatic glioma post op and post radiotherapy.
Imaging:
• On MR, extensive demyelination of the cerebral white matter with scalloped edges was noted which was not enhancing on the contrast study
• An enhancing tumour at the optico-chiasmatic area was also noted suggestive of recurrence.
Periventricular leucomalacia (PVL)
Number,age & sex:
• 4 cases out of 40.
• Age range was 3 to 9 years .
• M:F= 3:1
History & clinical presentation :
• H/O preterm delivery & asphyxia
• Full term infants with insult in the prenatal life
• Common clinical presentation was spastic diplegia (cerebral palsy) followed by seizures .
Imaging:
• White matter volume loss and Bilateral symmetrical hyperintensity of the periventricular white matter specially of the periatrial region in all patients.
• Ventriculomegaly and scalloping of ventricular margins
Metachromatic leukodystrophy (MLD)
• Two boys out of 40cases.
Sign & symptoms:
• Pyramidal dysfunction and developmental regression.
Imaging:
• Bilateral symmetrical diffuse periventricular hyperintensity.
• Thalamic hypointensity on T2-weighted images and cerebral atrophy in long standing disease.
Adrenoleukodystrophy (ALD)
Number, age & Sex:
• One case,four year old boy.
Sign & symptoms:
• Progressive visual loss and neuro regression.
Imaging:
• Hyperintensity on T2-weighted images in the periatrial region spanning the corpus callosum.
Discussion
• Though CT was used previously for cranial imaging in these conditions, it was not able to detect subtle lesions especially in stages of clinical inactivity and not ideal in posterior fossa imaging due to the beam hardening artifacts produced.
• MRI is a noninvasive modality with multiplanar imaging capability and has a very high sensitivity for demyelinating foci due to its excellent gray-white matter resolution.
• In this study, it was found that FLAIR sequences had a better sensitivity for subtle demyelinating foci especially those with periventricular locations.
Continued:
Multiple sclerosis
• Most of the other Indian series have reported a male preponderance in India.
•
Significant difference in clinical symptoms between Indian and Western MS was the higher frequency of visual involvement in Indian cases and low yield of oligoclonal bands in CSF.
• Most common site of lesion in this study was the periventricular area.
• MS patients demonstrated confluent / focal lesions involving the calloso-septal interface and concluded that callosal involvement was specific for MS.
• Whereas higher percentage of brainstem and cerebellar involvement (85&77%) in US.
• Cerebellar involvement is more commonly seen in Caucasians than in Orientals
• Other diseases discussed in this paper, there is no significant difference among indian and western countries.
Conclusion
• In this study, it was observed that a correct diagnosis could be made in majority of the patients based on MR findings and clinical history alone.
• Confirmation by brain biopsy thus is not essential in all patients except in indeterminate conditions.
• The authors conclude that MR, in conjunction with clinical findings, plays a significant role in establishing the diagnosis and in the further follow up of patients with white matter diseases.