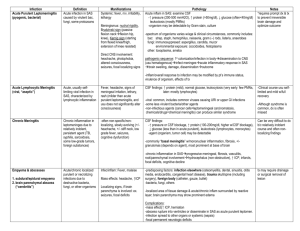
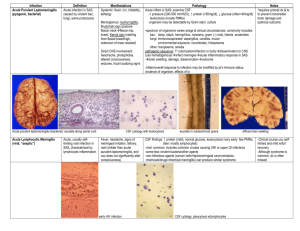
Acute hemorrhagic leukoencephalitis
advertisement
AMERICAN ASSOCIATION OF NEUROPATHOLOGISTS 51ST ANNUAL DIAGNOSTIC SLIDE SESSION Case 2010-10 Douglas C Miller MD,PhD University of Missouri School of Medicine Department of Pathology & Anatomical Sciences Case History This 65 year old man developed a cough and sore throat, which worsened over several days, bringing him initially to his primary care physician. He had a negative test for influenza and was told he had a viral illness, was given cough syrup, and was sent home. He developed fever to 104˚F, weakness, and anorexia and came to the hospital. He was admitted, started on oxygen, antibiotics, and bronchodilators, and was noted to have febrile neutropenia. He was neurologically normal. However he further deteriorated and required sedation, intubation, ICU admission, and pressors for septic shock. He developed ventricular tachycardia and then had an arrest after being given amiodarone; he was resuscitated. He developed acute renal failure. Six days after admission a head CT was said to show subarachnoid hemorrhage. He was weaned from sedation but remained comatose, thought secondary to hypoxic brain damage after his cardiac arrest. Given the poor prognosis the family agreed to comfort care only, and shortly thereafter he died. Permission for a full autopsy was obtained. CT scan without contrast Autopsy The general autopsy documented septicemia and a bilateral lower lobe pneumonia with Candida glabrata and coagulasenegative Staphylococcus; the bone marrow was hypercellular, thought consistent with sepsis. There was cardiomegaly with moderate coronary artery disease. The brain was 1600 grams (fixed weight) and was swollen with central herniation and had small foci of fresh subarachnoid hemorrhage. Coronal sections showed no abnormalities of the cortex, but the white matter had numerous scattered round petechiae, the largest of which was 0.6 x 0.5 cm in one section. There were also petechiae in the brainstem and in the cerebellar white matter. Material submitted: One Luxol Fast Blue/H&E combination stained section of cerebrum (from one of three areas) Small lesion from slide in DSS set. Note absence of LFB myelin staining in the lesion, which contains microglia and histiocytes. Diagnosis? Pathogenesis? From the gross the differential diagnosis included fat emboli. Oil Red O stains on frozen tissue showed no fat, and no bone marrow elements were seen in any vessels in any brain sections. Bielschowsky silver stains suggested relative preservation of axons in the perivascular areas with and without hemorrhage but lacking LFB + myelin. Immunostains for intermediate molecular weight neurofilament protein (NF-M; antibody RMDO20) confirmed the presence of axons but suggested acute axonal swelling and damage in the perivascular lesions. The cellular infiltrates were mostly histiocytes (CD68 +), and there was extensive diffuse activation of and infiltration by microglia. CD68, 20x CD45/LCA, 20x Azocarmine stains did not show fibrinoid necrosis of vessel walls although there is obviously fibrin in the hemorrhages. GFAP immunostains demonstrated an early gliosis in and around the lesions 20x 40x Diagnosis ACUTE HEMORRHAGIC LEUKOENCEPHALITIS (SYNONYMS: WESTON HURST DISEASE; ACUTE NECROTIZING ENCEPHALITIS; ACUTE NECROTIZING HEMORRHAGIC ENCEPHALITIS) Diagnosis, Pathogenesis AHEM is an post-infectious demyelinating disease often thought of as a fulminant and hemorrhagic variant of Acute Disseminated Encephalomyelitis In contrast to ADEM, AHEM is more often fatal, and (as here) is often discovered only at autopsy, although with MRI the diagnosis is made more frequently in life than formerly Survival has been reported with aggressive immunosuppressive therapy including high dose steroids, and survivors often have minimal sequelae This is believed to be a florid auto-immune disorder or immune-related hypersensitivity reaction causing vascular damage and demyelination, essentially a brain-limited Arthus reaction. It has been associated with a broad spectrum of triggering illnesses, with increasing attention paid to Mycoplasma pneumoniae upper respiratory infections References Hurst EW. Acute hemorrhagic leucoencephalitis: a previously undefined entity. Med J Aust 2, 1-6, 1941. General Neuropathological Descriptions Greenfield JG. Infectious Diseases of the Central Nervous System. Ch 3 in Neuropathology, 1st ed (JG Greenfield, W Blackwood, WH McMenemy, Meyer A, Norman KM, eds). London: Edward Arnold, 1958; pp. 205-207. Sobel RA, Moore GRW. Demyelinating Diseases. Ch 20 in Greenfield’s Neuropathology, 8th ed (S Love, DN Louis, DW Ellison, eds). London:Hodder-Arnold, 2008; pp. 1586-1588. Kleinschmidt-DeMasters BK, Simon JH. Dysmyelinating and Demyelinating Disorders. Ch 5 in Neuropathology. (R Prayson, ed). Philadelphia: Elsevier/Churchill Livingstone, 2007; pp. 217-219. Hart MN, Earle KM. Haemorrhagic and perivenous encephalitis: a clinical-pathological review of 38 cases. J Neurol Neurosurg Psychiatr 38, 585-591, 1975. Select Recent Articles References Pfausler B, Engelhardt K, Kampfl A, Spiss H, Taferner E, Schmutzhard E. Post-infectious central and peripheral nervous system diseases complicating Mycoplasma pneumoniae infection. Report of three cases and review of the literature. Eur J Neurol 9, 93-96, 2002. Leake JAD, Billman GF, Nespeca MP, Duthie SE, Dory CE, Meltzer HS, Bradley JS. Pediatric acute hemorrhagic leukoencephalitis: report of a surviving patient and review. Clin Infect Dis 34, 699-703, 2002. Lee HY, Chang K-H, Kim JH, Na DG, Kwon BJ, Lee K-W, Park SH. Serial MR imaging findings of acute hemorrhagic leukoencephalitis: a case report. Am J Neuroradiol 26, 1996-1999, 2005.