The Mangled Lower Extremity
advertisement
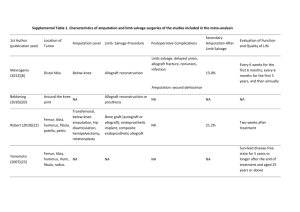
The Mangled Lower Extremity Dr. Marlis Sabo Orthopaedic Trauma Fellow 2011.04.28 Objectives To review emergency assessment and care of the open fracture To review the components of the mangled extremity and discuss treatment considerations To briefly outline the advantages/disadvantages of limb salvage compared with amputation Open Fractures Is that the bone sticking out?!? Components: Soft tissue loss Fracture/bone loss Vascular injury Nerve injury Immediate Care Place in context of ATLS protocol Examination IV antibiotics Tetanus Gross debridement Sterile dressing Splint limb Exam: Soft Tissue How big is the laceration? Is there loss of skin, muscle? How contaminated is it? What environment did the injury occur in (ie: barnyard, aquatic, etc.)? Exam: Vascular Palpable pulses? Asymmetry? Doppler pulses? Asymmetry? Wave form? Color, temperature of limb Compartments Expanding hematoma, pulsatile bleeding Exam: Neurologic Sciatic --> Tibial + Peroneal Femoral --> Saphenous Exam: Neurologic • Light touch & Sharp/Dull Exam: Neurologic Sciatic - knee flexion Tibial - ankle and great toe plantarflexion Peroneal Superficial - foot inversion/eversion Deep - ankle and great toe dorsiflexion Femoral - quads contraction/knee extension The Mangled Extremity What a M.E.S.S.! Considerations: • • 1. Is the limb salvagable? 2. If salvaged, will a functional limb result? Potential Scenarios Immediate amputation Attempted salvage with early amputation Successful salvage Unsuccessful salvage with late amputation Components of Salvage Bone stabilization Uniplanar fixator Circular fixator Delayed ORIF Components of Salvage Soft Tissue Coverage Primary closure Skin grafts Local or free flaps Components of Salvage Nerve Injury Nerve repair Tendon transfers Bracing/aids How do we know if the limb can be saved? Trauma Scores: MESS Energy Low Medium High Very High 1 2 3 4 Limb Ischemia Pulse reduced, perfused Pulse absent Cool, paralyzed, insensate 1 2 3 Shock SBP > 90 Transient Hypotension Persistent Hypotension 0 1 2 Age (years) < 30 YO 30-50 YO > 50 YO 0 1 2 Trauma Scores: NISSSA Nerve Injury Up to 3 Ischemia Up to 6 Soft Tissue Injury Up to 3 Skeletal Injury Up to 3 Shock Up to 2 Age Up to 2 Trauma Scores Several other examples Similar principles Variable ability to predict amputation Do not correlate well with final limb function Other factors: Other injuries • Scenario: open tibia fracture, distal limb pulseless, bone and soft tissue loss, partial plantar sensation Patient 1: 20 YO non-smoker, isolated injury Patient 2: 40 YO, bilateral flail chest with pulmonary contusions, aortic arch injury, hemodynamic instability in extremis Patient 3: 80 YO, known DM, known PVD, prior history of MI, chest injury Other Factors: Proposed Level of Amputation Below knee Through knee Above knee Energy of ambulation goes up with the level of amputation. When to consider salvage? Anatomically intact sciatic/tibial nerve Can reconstruct vascular supply: proximal injury, warm ischemia < 6 hrs Moderate soft tissue injury or loss Moderate bone loss Functional ankle, foot and knee Younger patients If salvaged, will a functional limb result? Bosse, NEJM 2002 Limb salvage v. amputation at 24 month F/U SIP scores similar between amp and salvage groups Reconstruction group more OR and hospitalization Neither group reflected population norms Approx. 50% had returned to work at 24 months Outcome more determined by social factors than treatment choice Busse, JOT 2007 Meta-analysis (9 eligible studies) Hospital stay same Salvage had longer rehab, higher cost, more complications, more surgery Salvage failed in 10-20% Return to work similar (50%) Results deteriorated over time in both groups Patient self-image may be better in limb salvage group So... To sum up: Mangled limb belongs to a patient - keep things in context Few indications for immediate amputation - time to consult, assess patient factors, educate Limb salvage and amputation have similar long-term outcomes Long-term disability common Thank-You