Laparoscopic Sleeve Gastrectomy
advertisement
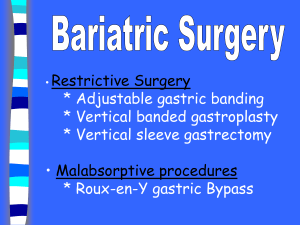
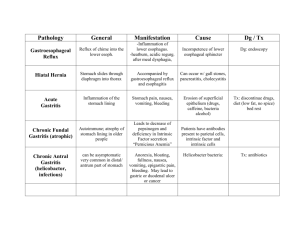
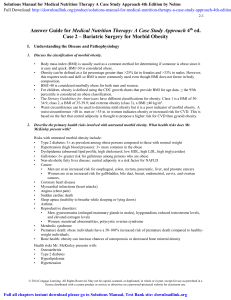
Bariatric surgery Laparoscopic Sleeve Gastrectomy By Dr Hosam Ghazy El-Banna Assistant Professor of General surgery Mansoura Faculty of Medicine Introduction Laparoscopic Sleeve gastrectomy (LSG) is a new restrictive bariatric procedure increasingly indicated in the treatment of morbid obesity. LSG is a reproducible and seems to be an effective treatment to achieve significant weight loss after 12 months follow-up. Indications LSG was indicated for weight reduction only for patients with a BMI > 40 or > 35 kg/m2 with severe comorbidity. Patients assessed by a dietician, a nutritionist, and a psychologist before surgery. Preoperative preparation Start Atkins diet for 2 weeks before the surgery to reduce the fat around your liver. Make sure to be on a regular intake of clear fluids 48 hours before surgery. Stop any medication unless indicated and recommended by your doctor. Operative procedure Operations are performed under general anesthesia using the supine position. Each procedure required only 4 trocars. Two 12-mm ports were placed in the supraumbilical region and in the left upper quadrant. One 10-mm port was placed in the right upper quadrant for liver retraction. One 12-mm port used for stapling was placed in the left mid-abdomen, just medial to the mid-clavicular line . Placement of 4 trocars Pneumoperitoneum was induced by primary trocar insertion and maintained at a pressure of 16 mm Hg. Dissection began on the greater curvature, 6 cm from the pylorus. The gastrocolic ligament along the greater curvature of the stomach was opened using a coagulator and was freed as far as the cardioesophageal junction. A 36-F plastic tube was then inserted perorally into the stomach by the anesthesiologist and was directed toward the pylorus. A laparoscopic linear stapler was introduced into the peritoneal cavity and was positioned so that it divided the stomach parallel to the orogastric tube along the lesser curvature. The instrument was fired, reloaded, and the maneuver was repeated; 60-mm green cartridge was used to staple the antrum followed by 3 or 4 sequential 60-mm gold cartridges to staple the remaining gastric corpus and fundus. After 5 or 6 firings of the stapler, the greater curvature was completely detached from the stomach. A methylene blue test was performed to exclude staple-line leakage. The gastric suture line was not systematically reinforced except in the case of bleeding or positive methylene blue test, in which case a drain was placed along the staple line. A nasogastric tube was left in place. A water-soluble upper gastrointestinal (GI) contrast study was performed on the first postoperative day, and oral fluids were allowed if no leakage was demonstrated. Patients were discharged except in the case of a complication resulting in prolongation of the hospital stay. Follow up Patients were reviewed at 1 month and then every 3 months. Mortality and morbidity were defined as death or complications and reoperations during the first 30 days after the operation or during the hospital stay, respectively. Eating after surgery Immediately after surgery, the patient is restricted to a clear liquid diet. The next stage provides a blended or pureed sugar-free diet for at least two weeks. Post-surgery, overeating is curbed because exceeding the capacity of the stomach causes nausea and vomiting. Advantages 1. 2. 3. 4. 5. 6. Stomach tends to function normally so most food items can be consumed in small amounts. Removes the portion of the stomach that produces the hormones that stimulates hunger (Ghrelin). No dumping syndrome because the pylorus is preserved. Minimizes the chance of an ulcer occurring. The chance of intestinal obstruction, anemia, osteoporosis, protein deficiency and vitamin deficiency are significantly reduced. Results appear promising as a single stage procedure for low BMI patients (BMI 35–45 kg/m2). Complications Leakage: can be treated easily by performing a second procedure that helps in strengthening the staple lines. Stapple line bleeding: Gastroesophageal Reflux: It might be happening because of the changes in the shape of the stomach. Gastric Fistula: may occur and another surgery may be needed to treat this condition. Narrowing of Stoma: A tube used for dilation is passed from the mouth to pass into the stomach as this expands the stoma. Hernia: Another surgery may be needed to repair this condition. Malabsorption of Vitamins and Minerals: 1. 2. 3. Anemia and vitamin B12 deficiency can cause neurological diseases. Changes in the absorption of phosphates, calcium and oxalates can result in kidney stone formation. Similarly, deficiency of vitamin D and calcium can also give rise to different disorders of the bone. Microbial infections : as pneumonia and intraabdominal abscess are most common. Deep vein thrombosis (DVT). Hair loss. Hair thinning. Mood swings. General feeling of weakness. Dry skin . Outcomes of SG & other bariatric procedures GB AGB BPD BPD+D switch SG 65-70% (EBW) 50% (EBW) 70% 70% 50-80% Morbidity 5% 5% 5% 5-10% 5% Mortality 0.1% 1% 1-5% …… Weight loss 0.5-1% vvvvvvvvvvvvvvvvv THANK YOU