Learning objectives
advertisement

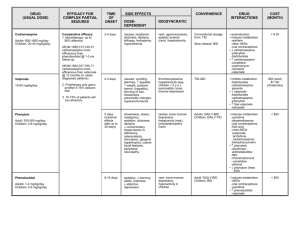
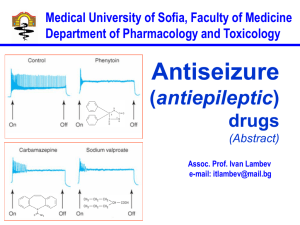
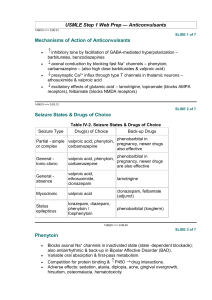
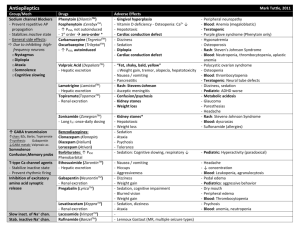
Management of Seizure Disorders Mark Kotlarewsky, MD FACP Department of Medicine Medstar Washington Hospital Center Learning objectives Understand the definition of seizure, epilepsy Understand the types of treatment, both medical and surgical Understand notable side effects of common antiepileptic drugs Understand treatment and management of epilepsy-related comorbidities Management of antiepileptic drugs in women Management of status epilepticus Conflicts of interest • None Definitions • seizure: abnormal, excessive, or synchronous neuronal activity in the cerebral cortex • 1-2 min, altered consciousness is common, confusion/fatigue after an episode, increased HR, tonic-clonic movement, paresthesias, aphasia • epilepsy: two or more unprovoked seizures • Seizure types Partial • • • • simple - does not impair awareness (eg. epileptic auras, jacksonian march) complex - impairs awareness by typically spreading to one or both temporal lobes secondarily generalized - when simple type spreads to involve both hemispheres diffusely Generalized • • • primary - tonic-clonic absence - impairment of consciousness myoclonic - muscle contractions in rapid succession without consciousness impairment Epilepsy types • partial • temporal lobe - mesial temporal sclerosis • generalized • juvenile myoclonic - morning myoclonus, absence Mesial temporal sclerosis Epilepsy-related comorbidities • psychiatric disorders - depression, suicide, anxiety • cognitive problems - visual/verbal memory, attention • osteoporosis, heart disease, hypertension, stroke, obesity, obstructive sleep apnea • sudden death • • • • • • • • Choosing an antiepileptic drug (AED) effectiveness for seizure type side effects drug-drug interactions comorbid conditions age gender lifestyle, patient preferences cost Choosing an AED by epilepsy type • • • • partial - nearly all, particularly lamotrigine, carbamazepine, oxcarbazepine, levetiracetam generalized - lamotrigine, levetiracetam, topiramate, zonisamide, NOT carbamazepine, gabapentin, pregabalin as they can sometimes exacerbate this type absence - ethosuximide, valproate atypical absence, myoclonic, atonic - valproate, lamotrigine, levetiracetam Initiating/adding treatment • • • • usually one drug, rather than two or more 2nd drug should have different mechanism, different side effect profile published therapeutic serum ranges should not be used if patient is doing well clinically (?) unclear whether generic substitutions lead to poorer control Mechanisms • • • • • • inhibitory transmission (benzodiazepines, clobazam, phenobarbital, tiagabine, vigabatrin) sodium channels (carbamazepine, lacosamide, lamotrigine, oxcarbazepine, phenytoin, rufinamide) calcium channels (ethosuximide) potassium channels (ezogabine) excitatory transmission (perampanel) multiple mechanisms (felbamate, valproate, gabapentin, levetiracetam, topiramate) AED side effects • • • • • sedation, ataxia folate deficiency renal metabolism - gabapentin, levetiracetam, pregabalin, topiramate, zonisamide hepatic metabolism - carbamazepine, phenytoin, valproate elderly: • • YES - gabapentin, lamotrigine, levetiracetam NO - oxcarbazepine, phenytoin, carbamazepine AED side effects • • • • suicide - levetiracetam, topiramate, vigabatrin Stevens Johnson Synrome, toxic epidermal necrolysis, drug rash - phenytoin, carbamazepine (allele screening hlab1502 in asians), oxacarbazepine, primidone, phenobarbital, zonisamide, lamotrigine osteoporosis - especially with: phenytoin, carbamazepine, phenobarbital, primidone and valproate; consider checking bone mineral density after five years use with caution in patients with cardiac conduction pathology: lacosamide, phenytoin, ezogabine AED side effects • • • • • • weight loss - zonisamide, felbamate, topiramate weight gain - pregabalin, gabapentin, valproate insomnia - felbamate, lamotrigine nephrolithiasis - topiramate, zonisamide valproic acid - exacerbates sx of polcystic ovarian disease carbamazepine - induces own metabolism Oral contraceptives • carbamazepine, phenytoin, phenobarbital, primidone tend to decrease contraceptive serum levels (also felbamate, topiramate, oxcarbazepine, rufinamide, clobazam, perampanel) • no interaction with levetiracetam, valproate • reduced lamotrigine concentrations, which then go up during the week of inactive tablets Pregnancy • • • • • • 4-6% rate of teratogenicity, 2-3x general population seizure control more important than teratogenicity aim: monotherapy at lowest dose for control avoid older AED’s: phenytoin, phenobarbital, valproate; latter two associated with oral cleft, cardiac, urinary tract, and neural tube defects, lower IQ topiramate: oral cleft, hypospadias better: lamotrigine, carbamazepine, levetiracetam, oxcarbazepine, gabapentin, but monitor levels closely Pregnancy • induces AED metabolism, esp. lamotrigine • phenytoin, carbamazepine, primidone, phenobarbital: hemorrhage in newborn due to vitamin K deficiency • folate: give 4mg starting 1-3 months prior to conception if on carbamazepine, valproic acid; standard dose for others Drug-drug interactions • phenytoin, carbamazepine, primidone, phenobarb, (oxcarbazepine, topiramate) • warfarin, OCP’s, anti-infectives, anticancer • between AED’s (eg. carbamazepine reduces lamotrigine levels, valproate increases them) • alcohol: 1-2 drinks in well-controlled patient OK, highest risk of seizure 7- Alternative tx • vagal nerve stimulation, deep brain stimulation of anterior nucleus of thalamus, responsive neurostimulator • epilepsy surgery - high rate of cure in patients with known lesions (eg. tumor, vascular malformation, mesial temporal sclerosis) • ketogenic/modified Atkins diet (hi fat, low carb) STATUS! • convulsive • • • • continued seizure activity >30 min; practically, initiate treatment within 5 min lorazepam fosphenytoin intubate, sedate, additional AED STATUS! • nonconvulsive • • • • 20% treated for convulsive status epilepticus, develop EEG seizure start management if altered mental status more than 20min post cessation of convulsive episode sensitivity of EEG increases longer it is done (95% at 48 hrs) paradoxical improvement with low dose benzodiazepines Case #1 • 35 yom w h/o simple partial seizure, failed levetiracetam due to side effects, recently switched to carbamazepine, presents c/o recurrent seizure What to do? 1. switch to lamotrigine 2. add lamotrigine 3. switch to ethosuximide 4. switch back to levetiracetam 5. check carbamazepine level Case #2 • 70yof w h/o osteoarthritis,1st degree AV block, hepatic disease, deep venous thrombosis on warfarin was diagnosed with partial seizure disorder and started on primidone; patient was lost to follow up but showed up in the ED with another DVT and a subtherapeutic INR What to do? 1. switch to valproic acid 2. switch to gabapentin 3. continue primidone, low INR is due to warfarin noncompliance 4. switch to lacosamide 5. switch to carbamazepine Case #3 • 31yof w h/o nephrolithiasis, renal insufficiency, and partial seizure disorder taking valproic acid and OCP is interested in having a child; aside from stopping her OCP... What do you recommend? 1. folic acid and carbamazepine 2. folic acid and lamotrigine 3. phenytoin 4. folic acid and topiramate 5. folic acid and valproic acid Case #4 • 21yom w h/o juvenile myoclonic epilepsy presents to the ED with uncontrolled seizure; after 15minutes of observed tonic-clonic seizure, and 6mg of IV lorazepam, the patient’s clinical status does not improve What to do next? 1. IV valproic acid, 30mg/kg at 3mg/kg/min 2. fosphenytoin 18 PE/kg at150PE/min 3. phenytoin 18mg/kg at 50mg/min 4. lorazepam 2mg 5. propofol 2-5 mg/kg bolus Thank you!