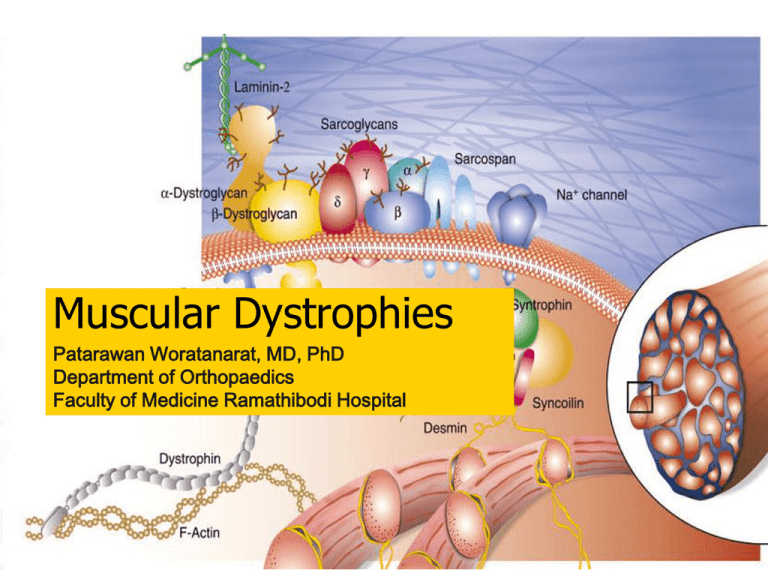
Muscular Dystrophies
Patarawan Woratanarat, MD, PhD
Department of Orthopaedics
Faculty of Medicine Ramathibodi Hospital
A 7-year-old boy presents with progressive
weakness of both legs for 4 years.
Definition
A group of
noninflammation
inherited distroders
progressive
degeneration and
weakness of skeletal
muscles
without cause in
peripheral / central
nervous system
Classification
Sex-linked: DMD, BMD, EDMD
Autosomal recessive: LGMD, infantile
FSHD
Autosomal dominant: FSHD, distalMD,
ocular MD, oculopharyngeal MD.
Duchenne Muscular dystrophy
Guillaume Benjamin Amand Duchenne
(French neurologist, 1860s)
Duchenne Muscular dystrophy
Etiology
single gene
defect
Xp21.2 region
absent
dystrophin
Duchenne Muscular dystrophy
Duchenne Muscular dystrophy
DMD: pathology
DMD: Epidemiology
Most common
male, Turner
syndrome
1:3500 live male
birth
1/3 new mutation
65% family history
DMD: Clinical manifestation
Onset : age 3-6 years
Progressive weakness
Pseudohypertrophy of
calf muscles
Spinal deformity
Cardiopulmonary
involvement
Mild - moderate MR
Pseudohypertrhophy of calf muscle, Tip toe gait
forward tilt of pelvis, compensatory lordosis
Disappearance of lordosis while sitting
DMD: Diagnosis
Gower’s sign
DMD: Diagnosis
Gait
absent DTR
Ober test
Thomas test
Meyeron sign
Macroglossia
Myocardial
deterioration
IQ ~ 80
Increase CPK (200x)
Myopathic change in
EMG
Bx: m. degeneration
Immunoblotting:
Absence dystrophin
DNA mutation analysis
Western blot
Normal dystrophin bands (230kD)
DMD: Natural history
Progress slowly and
continuously
muscle weakness
lower --> upper
extremities
unable to ambulate: 10
year (7-12)
death from pulmonary/
cardiac failure: 2-3rd
decade
DMD: Treatment
Prednisolone
Dystrophin replacement
Maintain function
PMR
orthosis
cardiopulmonary Rx
Counselling
DMD: Treatment
Surgery
Foot & ankle: Achillis, Tibialis posterior
release
Knee: Yount, hamstring release
Hip: Ober, modified Soutter procedure
DMD: Treatment
An 8-yr-old boy
Unable to stand
Percut. Tenotomy
Achillis tendon
Ambulate with
orthosis
DMD: Treatment
Surgery
Upper extremity: Spinal deformity: posterior spinal fusion + pelvis
Becker muscular dystrophy
Peter Emil Becker
(German doctor, 1950s)
Becker muscular dystrophy
Milder version of
DMD
Etiology
single gene defect
short arm X
chromosome
altered size &
decreased amount of
dystrophin
Becker muscular dystrophy
BMD: Epidemiology
Less common
1: 30000 live male birth
Less severe
Family history: atypical MD
BMD: Clinical manifestation
Similar & less severe than DMD
Onset: age > 7 years
Pseudohypertrophy of calf
Equinous and varus foot
High rate of scoliosis
Less frequent cardiac involvement
BMD: Diagnosis
The same as DMD
Increase CPK
(<200x)
Decrease dystrophin
and/or altered size
BMD
Natural history
Slower progression
ambulate until
adolescence
longer life expectancy
Treatment
the same as in DMD
forefoot equinous:
plantar release,
midfoot dorsalwedge osteotomy
Emery-Dreifuss muscular dystrophy
Etiology
X-linked recessive
Xq28
Emerin protein (in
neuclear membrane)
Epidemiology
Male: typical phenotype
Female carrier: partial
EDMD: Clinical manifestation
Muscle weakness
Contracture
Neck extension, elbow, achillis tendon
EDMD: Clinical manifestation
Scoliosis: common, low incidence of
progression
Bradycardia, 1st degree AV block
sudden death
EDMD
Diagnosis
Gower’s sign
Mildly/moderately
elevated CPK
EMG: myopathic
Normal dystrophin
Natural history
1st 10 y: mild weakness
Later: contracture,
cardiac abnormality
5th-6th decade: can
ambulate
Poor prognosis in
obesity, untreated
equinus contractures.
EDMD: Treatment
Physical therapy
Soft tissue contracture
Achillis lengthening, posterior ankle capsulotomy + anterior
transfer of tibialis posterior
Spinal stabilization
Prevent contracture: neck, elbow, paravertebral muscles
For slow progress elbow flexion contracture
For curve > 40 degrees
Cardiologic intervention
Cardiac pacemaker
Limb-girdle muscular dystrophy
Eitology
Autosomal recessive at chromosome 15q
Autosomal dominant at 5q
Epidemiology
Common
More benign
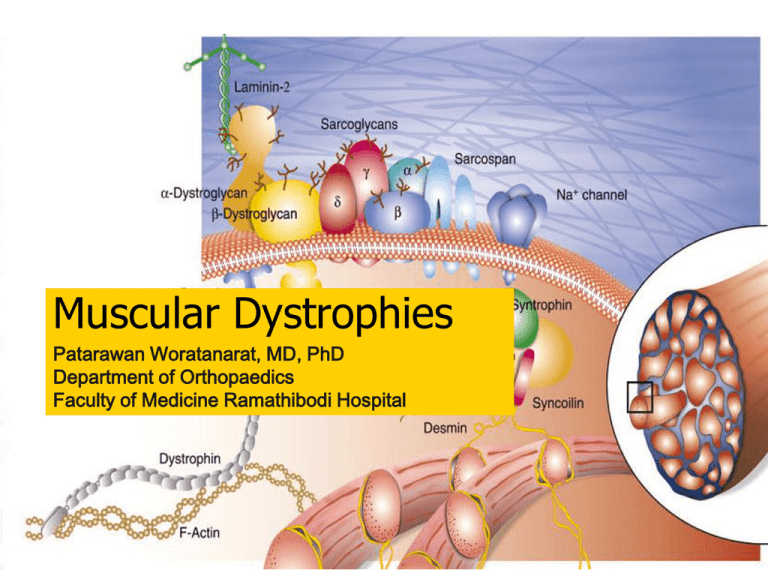
Limb-girdle muscular dystrophy
an absence of functional
sarcoglycans components of
the dystrophin glycoprotein
complex (DCG).
Other LGMD result from the
absence of functional
caveolin-3
Limb-girdle muscular dystrophy
Clinical manifestation
Age of onset: 3rd
decade
Initial: pelvic/shoulder
m. (proximal to distal)
Similar distribution as
DMD
LGMD
Classification
Pelvic girdle type
Diagnosis
common
Scapulohumeral type
rare
Same clinical as
DMD/BMD carriers
Moderately elevated
CPK
Normal dystrophin
LGMD
Natural history
Slow progression
After onset > 20 y:
contracture &
disability
Rarely significant
scoliosis
Treatment
Similar to DMD
Scoliosis: mild, no
Rx.
Fascioscapulohumeral muscular dystrophy
Etilogy
Autosomal dominant
Gene defect (FRG1)
Chromosome 4q35
Epidemiology
Female > male
Clinical
manifestation
Age of onset: late
childhood/ early
adult
No cardiac, CNS
involvement
FSMD: Clinical manifestation
Muscle weakness
face, shoulder, upper
arm
Sparing
Deltoid
Distal pectoralis
major
Erector spinae
“Popeye”
appearance
Lack of facial
mobility
Incomplete eye
closure
Pouting lips
Transverse smile
Absence of eye and
forehead wrinkles
FSMD: Clinical manifestation
Winging scapula
Markedly decreased
shoulder flexion &
abduction
Horizontal clavicles
forward
sloping
scoliosis
Rare
FSMD
Diagnosis
PE, muscle biopsy
Normal serum CPK
Natural history
Slow progression
Face, shoulder m.
pelvic girdle, tibialis
ant
Good life expectancy
Treatment
Posterior scpulocostal
fusion/ stabilization
(scapuloplexy)
Distal muscular dystrophy
Autosomal dominant
trait
Rare
Dysferlin (mb prot)
defect
Age of onset: after 45 y
Distal muscular dystrophy
Initial involvement:
intrinsic hands, claves,
tibialis posterior
Spread proximally
Normal sensation
DD: Classification
Welander distal myopathy
Finnish/Markesbery distal myopathy
Miyoshi distal myopathy
Nonaka distal myopathy
Gower: autosomal dominant, Chromosome 14
Hereditary inclusion-body myositis
Hereditary inclusion-body myuositis
Distal myopathy with vocal cord & pharyngeal
weakness
Congenital muscular dystrophy
Etiology
Autosomal recessive
Integrin, fugutin defect
Laminin 2 chain
merosin
CMD:
Epidemiology
Rare
Both male and female
Classification
Merosin-negative
Merosin-positive
Neuronal migration
Fukuyama
Muscle eye-brain
Wlaker-Warburg
CMD: Clinical manifestation
Stiffness of joint
Congenital hip
dislocation,
subluxation
Achillis tendon
contracture, talipes
equinovarus
Scoliosis
CMD
Diagnosis
Muscle Bx: Perimysial
and endomysial
fibrosis
Treatment
Physical therapy
Orthosis
Soft tissue release
Osteotomy
Summary
Clinical
DMD
LGMD
FSMD
DD
CMD
Incidence
common
less
Not
common
Rare
Rare
Age of onset 3-6 y
2nd decade
2nd decade
20-77 y
At/ after
birth
Sex
Male
Either sex
M=F
Either sex
Both
Inheritance
Sex-linked
recessive
AR, rare AD
AD
AD
Unknown
Muscle
involve.
Proximal to
distal
Proximal to
distal
Face &
shoulder to
pelvic
Distal
Generalized
Muscle
spread until
late
Leg, hand,
arm, face,
larynx,eye
Upper ex,
calf
Back ext,
hip abd,
quad
Proximal
-
Summary
Clinical
DMD
LGMD
FSMD
DD
CMD
Pseudo
hypertrophy
80%
calf
< 33%
Rare
no
No
Contracture
Common
Late
Mild, late
Mild, late
Severe
Scoliosis
Kyphoscoliosis
Common,
late
Late
-
-
?
Heart
Hypertrophy
tachycardia
Very rare
Very rare
Very rare
Not
observed
Intellectual
decrease
Normal
Normal
Normal
?
Course
Stead, rapid
Slow
Insidious
benign
Steady
Thank you
Infantile fascioscapulohumeral
muscular dystrophy
Clinical manifestation
Etiology
Autosomal recessive
Unidentified gene
Facial diplegia
Sensorinueral hearing
loss
Mobius type of facial
weakness
Walk with hands and
forearms folded across
upper buttocks
**Marked & progressive
lumbar lordosis (pathog)
Less common equinous,
scoliosis
IFSMD
Natural history
Infancy: facial
diplegia
Childhood:
sensorineural hearing
loss
2nd decade of life:
wheelchair bound,
severely
compromised
pulmonary function
Treatment
Flexible
equinous/equinovarus
foot: AFO + TAL
Hip flextion
contracture: no Rx in
ambulate pt.
Spinal deformity in
wheelchai ambulator:
orthosis+ post spinal
fusion with
instrumentation
Scapulothoracic
Ocular muscular dystrophy
Rare
Age of onset: adolescence
Extraocular muscle weakness
diplopia limit ocular movement
May involve proximal upper extremities
Slowly progressive
Oculopharyngeal muscular
dystrophy
Autosomal dominant
with complete
penetrane
Age of onset: 3rd
decade
Ptosis in middle life
OPMD
Pharyngeal
involvement
Dysarthria
Dysphasia
Repetitive
regurgitation
Frequently choking