CHRONIC OBSTRUCTIVE PULMONARY DISEASE
advertisement

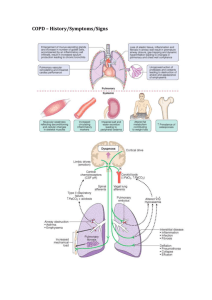
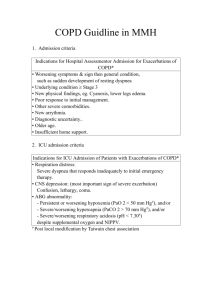
CHRONIC OBSTRUCTIVE PULMONARY DISEASE By Dr Aguilera Definition In 2001, the Global Initiative for Chronic Obstructive Lung Disease (GOLD) report was developed to define COPD by an expert panel which includes the National Heart, Lung and Blood Institute and the World Health Organization. COPD is “A disease state characterized by airflow limitation that is not fully reversible; it is usually both progressive and associated with an abnormal inflammatory response of the lungs to noxious particles or gases.” Definition Cont’d Previous Guidelines and Definitions included Chronic bronchitis and emphysema, but these are not included in the current definition. The GOLD report’s definition of COPD regards chronic bronchitis, emphysema and asthma as different aspects of the disease that are not mutually exclusive. Definition Cont’d Chronic Bronchitis Emphysema Defined by the presence of chronic productive cough for three months in each of two successive years in a patient in whom other causes of cough are excluded Is a pathological term describing the abnormal permanent enlargement of airspaces distal to the terminal bronchioles, accompanied by destruction of their walls without obvious fibrosis. Asthma Chronic inflammatory disease of the airways with bronchial hyper-responsiveness, reversible airway obstruction, and respiratory symptoms. (See previous lecture) Pathophysiology Bronchial inflammation Caused by inflammatory cells (macrophages, neutrophils and CD8 cytotoxic T cells) in a response to noxious stimuli release of enzymes (proteases) these cause destruction of connective tissue in the airways and alveolar walls. Also stimulate mucus production by goblet cells Different than what we see in Asthma (CD4 and eosinophils) Ciliary damage occurs directly by noxious stimuli (tobacco, occupational dusts and chemicals, and air pollution) Pathophysiology Cont’d Variability of Response to Noxious Stimuli Genetics imbalance of antiproteases May explain why only approximately 15% of smokers develop COPD Alpha-1-antitrypsin deficiency As a result, air trapping, collapse of alveoli and inability to clear debris from the airways occur, which manifest clinically as the COPD syndrome. Disease Interrelationships Chronic bronchitis Emphysema 1 COPD 2 5 3 4 8 7 6 10 9 Airflow Obstruction Asthma Epidemiology Approx 16 million people in U.S. have COPD 5th leading cause of death In 2000: ED visits = 1.5 million Hospitalizations = 726,000 Deaths = 119,000 Health care costs approx 15 billion/year Tobacco smoking accounts for 80-90% of cases 4th in people > 45 yrs Most deaths occur in people > 65 years Only 15% of smokers develop COPD Women are affected more than men with same tobacco exposure Alpha-1-antitrypsin accounts for <.1% of cases Homozygous (.02%) < Heterozygous (2-3%) - whites When to test for serum levels? In pts with COPD at young age, particularly in those with (+) FHx and no exposure to tobacco Replace with alpha-1-proteinase inhibitor (Prolastin) Diagnosis History Patients with COPD usually have been smoking at least 20 pack years before symptoms develop. Cough usually is the first symptom. This is followed by sputum production and then shortness of breath which worsen over time and may get worse with exacerbations. Wheezing may be present Exposure to risk factors: tobacco, occupational dusts and chemicals, air pollution Diagnosis Cont’d Physical Examination Usually normal early in the course of the disease Findings are variable as the disease progresses Chest Signs Prolonged expiration with/out wheeze; decreased breath sounds; Crackles especially with exacerbations; Increased anteroposterior diameter due to hyperinflation Distant heart sounds Extrathoracic Signs Leaning forward to relieve dyspnea; weight loss, cyanosis Manifestations of Cor Pulmonale Poor Px Diagnosis cont’d Pulmonary Function Test (PFT)/Spirometry Gold standard for diagnosis COPD FEV1/FVC ratio of < 70% defines the presence of obstructive disease. Cannot determine difference between COPD, chronic bronchitis or emphysema FEV1 is used to determine severity of disease Peak Expiratory Flow Rate (PEFR) is used to monitor response to therapy Lung function should be measured with bronchodilator evaluation. The absence of a significant response (>15% increase in FEV1) on one test should not be the reason to hold bronchodilator therapy. If improvement >20% and FEV1 becomes normal = Asthma If FEV1 increases but is still below normal = Mixed Asthma/COPD Diagnosis Cont’d Chest X-Ray (CXR) Arterial Blood Gas (ABG) Radiological changes don’t usually occur until COPD is advanced (overdistention, bullae formation Done to identify co-existing conditions Used in most cases to determine if a patient requires oxygen maintenance based on level of hypoxia Usually done when FEV1 < 40%, and in those with signs of respiratory failure (PO2<60 or PCO2>45) or right heart failure Can also give information regarding CO2 levels Complete Blood Count (CBC) Can identify erythrocytosis/polycythemia as a result of chronic hypoxemia and should be done in patients being considered for O2 supplementation Classification of COPD (Remember FEV1/FVC is used in the Dx COPD!) % Predicted FEV1 1995 ATS % Predicted FEV1 80-100% 2001 GOLD Report % Predicted FEV1 Symptoms Stage 0: At risk, but PFT’s are normal FEV1/FVC > 70% Cough and sputum production may be present Stage I: Mild > 80% predicted Cough and sputum production may be present 50-80% Stage I: Mild 50-80% predicted Stage IIA: Moderate 50-80% predicted Cough and sputum and dyspnea may be present 0-50% Stage II: Moderate 35-50% predicted Stage IIB: Moderate 30-50% predicted Cough, sputum and dyspnea with more exacerbations Stage III: Severe <35% predicted Stage III: Severe < 30% predicted or resp failure or RHF Cough, sputum and dyspnea with frequent exacerbations Overall Treatment of COPD 1st Step is to establish a diagnosis Spirometry in patients with Sx or RF CXR to exclude other conditions 2nd Step is to Classify the stage of disease Used to guide therapy For example, Stage II requires smoking cessation, an ABG, pharmacotx and consultation with a pulmonologist 3rd Step is to educate your patients This is the key component Main goals of treatment are to improve quality of life and decrease mortality Only 2 interventions decrease mortality: smoking cessation and long term O2 supplementation Overall Treatment Cont’d 4th Step is to begin Pharmacotherapy Inhaled Bronchodilators Improve symptoms and decrease airflow limitation Albuterol 2 puffs Q6hrs/PRN Ipratropium Common problems Usually first line therapy Start with 2 puffs QID and may increase to 6 puffs TID Inadequate education regarding meds and technique Suboptimal dosing Inadequate monitoring of response to treatment The use of long acting beta agonists (Salmeterol and Formoterol) in COPD is still in evolution. Overall Treatment Cont’d Inhaled Steroids Do not affect the decline in FEV1, thus the severity In mod-severe disease these meds showed a significant decrease in the frequency of symptoms and exacerbations Theophylline GOLD report recommends against its use due to availability of other drugs, high Sfx profile and drug interactions. Does work for some patients Keep levels between 8-12 mcg/ml Monitor regularly Be aware of drug interactions Overall Treatment Cont’d Oral Steroids Long term use is not recommended A beneficial response to a short course of an oral steroid does not predict benefit from the chronic use of oral steroids. Long term disease effects are unknown. Studies failed to show a difference in the # of exacerbations, symptoms or spirometry results when continuation vs withdrawal of prednisone was compared If considering long term oral steroids for a patient with severe disease, then use smallest dose possible. Usually done in conjunction with pulmonologist. Overall Treatment Cont’d 5th step is to prevent and treat complications Chronic Hypoxia Consequences include dyspnea, impaired cognition, ischemic CM, ploycythemia/ erythrocytosis with hyperviscosity syndromes, and pulmonary HTN Supplemental O2 can improve symptoms and prevent some of these complications. In fact, life expectancy increases. ABG evaluation at appropriate times MediCare guidelines PaO2 < 55mmHg; POx < 88% for any patient PaO2 55-59mmHg; POx = 89% for those with chronic hypoxic complications as listed above Overall Treatment Cont’d Immunizations Annual influenza shots Polyvalent pneumococcal vaccine at time of diagnosis and again in 5 years or at age 65, whichever comes later. Consultation with a specialist Pulmonologist Stage IIB and III Surgeon When considering lung volume reduction surgery or transplantation THE END