T.B. OSTEOMYELITIS
advertisement

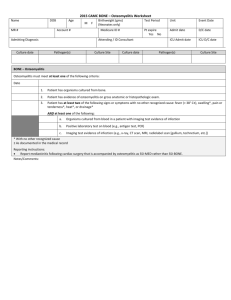
Chronic Osteomyelitis Factors responsible for chronicity Local factors: Cavity, Sequestrum, Sinus, Foreign body, Degree of bone necrosis General: Nutritional status of the involved tissues, vascular disease, DM, low immunity Organism: Virulence Treatment: Appropriateness and compliance Risk factors: Penetrating trauma, prosthesis, Animal bite Chronic Osteomyelitis Types A complication of acute Osteomyelitis Post traumatic Post operative Chronic Osteomyelitis Clinical picture Continuous or intermittent suppuration and sinus formation with acute exacerbations. Pain, fever, redness, and tenderness during acute exacerbations. Discharging sinus with +ve/-ve culture. Pathological fracture. Chronic Osteomyelitis Investigation Lab tests/ culture Plain X-ray: Bone rarefaction surrounded by the dense sclerosis, sequestration and cavity formation Sinogram Bone scan & gallium scan To detect chronic multifocal osteomyelitis CT Scan & MRI Biopsy Chronic Osteomyelitis Complications Recurrence & Recurrence & Recurrence Pathological fractures Growth disturbance Amyloid disease Epidermoid carcinoma of the fistula CHRONIC OSTEOMYELITIS Sequel of acute/open fracture/opt. C/F: pain, discharging sinus, scars Xray- bone resorption, sequestra, CT/MRI: extent of bone loss, oedema, hidden abscess Lab-raised ESR pus-cs TREATMENT Antibiotics. Local treatment. Operations. After care. TUBERCULOSIS A surgeon could gain experience in the management of TB. Of bone and joint only if he choose to work in econmically less developed countries. (edit, Br.Med.J>1968) T.B. OSTEOMYELITIS 1/3 population infected. Over 80,000 people in Nepal have TB. 22,000 develop Pul. TB every year. Total 50,000. 10,000 die of TB. LEADING CAUSE OF DEATH. 1 – 3% skeletal TB TB Cause by Mycobacterium tuberculosis, occasionally by M.bovis/africanum. Also known as tubercle bacilli as they produce lesion – tubercles. Acid fast bacilli. Transmission – airborne droplets. Risk- extent of exposure to droplets and susceptibility to infection. TB Primary infection Exposure to tubercle bacilli – Lungs – multiplication of bacilli in terminal alveoli (Ghon focus) – lymphatic drain it to hilar lymph nodes – (PRIMARY COMPLEX) – BLOOD – SPREAD. TB C/F:Cough >3wks.,sputum production, weight loss, monoarticular. Respiratory – haemoptysis, chest pain, breathlesness. Constitutional:fever/night sweat , tiredness , loss of appetite. Physical sign: non specific,muscle wasting, loss of ROM TB 3 days sputum. Ziehl-Neelsen stain. X-ray: cavitation, infilteration, lymphadenopathy. Full blood count:Relative lymphocytosis,^ ESR,Anemia. Serology. Lymphnode biopsy. CT/ MRI BONE TUBERCULOSIS Spread from primary complex to any bone/joints. Can effect any bone but the weight bearing bones are more likely to be affected. Spine –commonest, hip, knee , foot. STAGES OF ARTICULAR TB 1 – SYNOVITIS. 2 – EARLY ARTHRITIS. 3 – ADVANCED ARTHRITIS. 4 – ADV.ART. PATHOLOGICAL DISLOCATION / SUBLUXATION. 5 – AFTER MATH TERMINAL OF GROSS ARTHRITIS. STAGES C/F XRAY PROGNOSIS 1 synovitis ROM>75% SOFT TISSUE SWELLING, OSTEOPOROSIS NEAR NORMAL 2 early arthritis ROM50-75% JT.SPACE DIMINITION AND MARGINAL EROSION RESTORATION UPTO 75% 3 Adv. arthritis ROM >75% ALL DIRECTION DESTRUCTION OF JT. SURFACE ANKYLOSIS 4Adv. Arth path/disln DO DISORGANISE JT. DIS/SUB.LOCATION ANKYLOSIS 5 Aftermath GROSS DEFORMITY DEFORMED JT. , OA ANKYLOSIS TB - TYPES Caseous exudativemore destruction, exudation & abscess formation. Symptoms more marked. Onset is less insidious. Granular type – less destructive. Abscess formation rare. Dry lesion. adults TUBERCULOSIS Spine is the most common site of skeletal TB TUBERCULOSIS Pathology Blood borne - settles in vertebral body anteriorly usually more bone destruction, more sequestra, larger abscess, gaseous pus than pyogenic OM intervertebral discs preserved until late disease TB SPINE -Classification 12345- pre-destructive early destructive. mild angular kyphos. moderate angular kyphos. severe kyphos (humpback) STAGES –1 & 2 Predestructive – straightening of curvatures , spasm of perivertebral muscles, MRImarrow oedema. Early destructive – Diminished disk space and paradiscal erosion.MRI-marrow oedema and break of osseous margin.CT-marginal erosion /cavitaion STAGE 3,4&5 –Body destruction with Kyphos Mild 2-3 vertebra moderate severe >3 body >3 body Kyphosis – 10-30* 30-60* >60* TB SPINE –D/D AGE- anomalies. Infection. Tumour. Traumma. Osteoporosis ,Osteochondrosis. Spondylolisthesis. TB SPINE C/F:Back pain of variable duration, fever and weight loss. O/E: local tenderness, spasm, mild kyphosislate Gibbus, cold abscess and paraparesis. DIAGNOSIS: XRAY-erosion of the anterior edges of the superior and inferior boarders of adjacent vertebral bodies with narrowing of disc space. USG :paravertebral abscess. Biopsy/ CT scan TB HIP C/F: pain/limping, irritable hip –child. Gradual loss of range of movement, flexion deformity, wasting of thigh muscles. Xray: both hip to compare.Early changes – rarefaction of the bone and widening of the joint space, later destruction of the joint. Synovial bioposy. TB KNEE / ANKLE. C/F: pain and synovial swelling, muscle wasting., contracture, draining sinuses. X-ray. Synovial biopsy. PRINCIPLES OF MANAGEMENT OF TB General. Rest, mobilization & brace. Abscess, effusion & sinuses. Antitubercular drugs. surgery TB PROBLEMS Diagnosis. Treatment . Anti tuberculous drugs. Tuberculous lesion Resolve completely. Complete healing with varying degree of deformity / loss of function. Lesion may be complete walled off and the caseous tissue may calcified. Persist as a low grade ch.fibromatous granulating & caseating lesion. Infection may spread. Damage growth centre with shortening. CONCLUSION Slow progressive course of clinical symptoms and radiological signs of tuberculosis creates difficulty in early diagnosis. Anti tuberculous treatment is effective but the functional outcome depends on early diagnosis before the development of radiological evidence of joint destruction. Always keep TB in D?Diagnosis Thank you for not sleeping Now you can ask your questions ???