Surgical Foot Reconstruction for Posterior Tibial
T RAUMATIC D ROP F OOT
By: Larissa Torres Nixon, SPT
Regis University
July 16, 2010
V IDEO
http://www.youtube.com/watch?v=Q8KB2fhLDw
M&feature=related
P URPOSE :
Explain the importance of doing a thorough examination on patients with traumatic drop foot and the intervention options physical therapists can offer these patients.
O BJECTIVES :
Student will be able to describe the pathology for a person with traumatic drop foot.
Student will be able to explain information obtained during the examination and evaluation for this patient.
Student will be able to discern a more thorough evaluation process for this patient based on evidentiary support.
Student will be able to develop an intervention strategy using current literature evidence.
P ATIENT CONSULTATION :
Pt is a 25 y.o. male active duty Army (ADA)
Dx: Pt is status post multiple reconstruction surgery due to blast injury.
Rx: Please evaluate and treat.
W HAT IS D ROP F OOT ?
Traumatic drop foot is usually occupation or sport related.
7
Caused by chronic compression, traction or transection of the common peroneal or deep peroneal nerve.
7
Injury to the common peroneal nerve results in weakness of all muscles innervated by the superficial and deep branches.
7
T RAUMATIC D ROP F OOT : ( CONT )
Tibialis anterior muscle is the primary ankle DF.
2
Tibialis anterior has the highest activity at heel strike and after toe off during the swing phase.
2
Disruption leads to foot drop.
Common gait deviations include: flatfoot/forefoot contact, decreased push off, and excessive hip and knee flexion with ankle PF.
E XAMINATION :
Through patient history
Systems Review
Special tests
Posture/Gait observation
MMT
ROM
Sensory/proprioceptive testing
Scar mobility
Outcome measure: LEFS
EMG and NCV studies can be used to determine the degree of nerve damage and potential for nerve recovery. However, are not necessary to diagnose drop foot. 1
S UBJECTIVE H ISTORY :
Sx: c/o left drop foot, multiple trips/near falls over the past 3 months. Pain with first few steps after getting up.
Hx: MOS: 11B, was hit by an RPG August 30, 2009 on left lower leg while deployed in Afghanistan. Was
MEDDVAC’d to Germany then transferred state side.
S UBJECTIVE H ISTORY : ( CONT )
He had a series of
10 limb salvation surgeries from
September to
November 2009, including an external fixator placed at Walter
Reed Army
Medical Center.
S UBJECTIVE H ISTORY : ( CONT )
November 2009:
Pt had muscle flap of left latisimus dorsi transferred to left calf and skin graft from left thigh placed over site.
E XAMINATION F INDINGS :
Systems Review
Cardiovascular: posterior tibial and dorsal pedal pulses present
Neuromuscular: reflexes 3+ Lt quad tendon, 2+ Rt quad tendon/ bilat triceps surea
- Babinski bilat.
Endocrine: No significant findings
Integumentary: 8 fully healed screw wholes and fully healed skin graft
Musculoskeletal: also being treated by physical therapy for Lt shoulder injury that occurred from the same incident.
E XAMINATION F INDINGS : ( CONT )
Posture observation
Assymetirical WBing to
Rt LE
Excessive ER of Lt LE
Gait Observation
Forefoot contact at heel
strike
Excessive knee/hip flexion with swing phase
Toe drop on Lt throughout swing phase
Decreased stance time on Lt
MMT
Rt LE: 5/5 throughout
Lt hip flex: 5/5
Lt knee flex: 5/5
Lt knee ext: 4+/5
Lt ankle DF: 0/5
Lt ankle PF: 1/5
Lt ankle Inv: 1/5
Lt ankle Ever: 0/5
Great toe Ext: 0/5
Minimal ability to wiggle toes noted.
E XAMINATION F INDINGS : ( CONT )
PROM
Rt Ankle: 0 ̊ DF to 70 ̊ PF
Lt Ankle:
10 ̊ PF to 35 ̊ PF
Sensory/proprioceptive testing
Light tough: diminished L4, L5, S2 on Lt
10/10 monofilament test on plantar surface of foot
Balance: 30 seconds with EC on Rt, 7 seconds with eyes open on Lt
Proprioception: 4/10 correct on Lt ankle
Scar mobility
Poor scar mobility of 8 pin holes and lateral ankle incision.
Outcome measure: LEFS
38/80 (where 80/80 means no disability) 4
MCID is 9 points
E XAMINATION F INDINGS :
NCV:
Diminished NCV of Lt tibial nerve (35 ms), absent on Lt peroneal nerve
EMG:
Intact Lt femoral nerve, sciatic nerve
Diminished activity of the Lt tibial nerve with maximum contaction
No activity of Lt common peroneal nerve and it’s branches.
D IAGNOSIS & P ROGNOSIS :
Diagnosis:
Left drop foot with complete neural loss of the common peroneal nerve and it’s branches.
Prognosis:
Poor
If there are no signs for nerve recovery with EMG after 6 months then there will likely be no recovery of function.
3
I NTERVENTIONS & E VIDENCE :
For a patient with complete loss of muscle innervation
2,7
Maintain ankle ROM
Prevent PF contracture
Address gait impairments with AFO
Long term treatments may include
2,7
Talocrural and subtalar joint fusion
Posterior tibialis tendon transfer
No appropriate for this patient
BKA
O RTHOSES : D OES E VIDENCE MATCH MY
PATIENT ?
Eberly et al. 6
O RTHOSES : D OES E VIDENCE MATCH MY
PATIENT ?
Patients with common peroneal nerve palsey require a more solid, rigid
AFO than those with only deep peroneal nerve palsey.
8
He is still waiting to receive his AFO.
T AKE AWAY:
These returning injured soldiers will be PT patients both acutely and later in our careers.
If you have a patient with a traumatic injury always ask if the patient has pictures from the initial injury or just prior to surgery.
EMG and NCV studies done in the physical therapy clinic can provide helpful information for diagnosis and prognosis of a patients injury.
C HECK FOR UNDERSTANDING :
What are the causes of traumatic foot drop?
Which nerve(s) cause foot drop when they are damaged?
What are 2 physical therapy interventions for a patient with traumatic foot drop?
R EFERENCES :
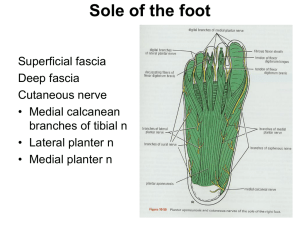
Images:
Photos provided by the featured patient
Family practice notebook.com http://www.fpnotebook.com/_media/AnkleAnatomyMuscleAP.gif
Twin Oaks Orthotics & Prosthetics: http://www.bing.com/images/search?q=AFO&FORM=BIFD#focal=57a9fe3e43ec50b4ffe5eef02b ec67e6&furl=http%3A%2F%2Fwww.twincityop.com%2Fsitebuildercontent%2Fsitebuilderpict ures%2FAFO_Family.jpg
Articles:
1.
2.
3.
4.
5.
Aminoff M. Electrophysiologic testing for the diagnosis of peripheral nerve injuries.
Anesthesiology [serial online]. May 2004;100(5):1298-1303.
Baima J, Krivickas L. Evaluation and treatment of peroneal neuropathy. Current Reviews
In Musculoskeletal Medicine [serial online]. June 2008;1(2):147-153.
Berry H, Richardson P. Common peroneal nerve palsy: a clinical and electrophysiological review. Journal Of Neurology, Neurosurgery, And Psychiatry [serial online]. December
1976;39(12):1162-1171.
Binkley J, Stratford P, Lott S, Riddle D. The Lower Extremity Functional Scale (LEFS): scale development, measurement properties, and clinical application. Physical Therapy
[serial online]. April 1999;79(4):371-383.
Chémali K, Tsao B. Electrodiagnostic testing of nerves and muscles: when, why, and how to order. Cleveland Clinic Journal Of Medicine [serial online]. January 2005;72(1):37-48.
6.
7.
8.
Eberly V., Kubota K., Weiss W. To brace or not to brace: Making evidence-based decisions with our clients with neurologic impairments. Paper presented at: Combined Sections
Meeting of the American Physical Therapy Association; February 1-5, 2006; San Diego, CA.
Elman L, McCluskey L. Occupational and sport related traumatic neuropathy. The
Neurologist [serial online]. March 2004;10(2):82-96.
Geboers J, Drost M, Spaans F, Kuipers H, Seelen H. Immediate and long-term effects of ankle-foot orthosis on muscle activity during walking: a randomized study of patients with unilateral foot drop. Archives of Physical Medicine & Rehabilitation [serial online].
February 2002;83(2):240-245.