Stroke Audit in the UK

Stroke Care in the UK
Tony Rudd
Organisation of Services
• 120,000 new strokes per year
• Approx 200 hospitals treating acute stroke patients
• Most services providing combined acute and rehabilitation services
• Specialist rehabilitation services in community e.g. Early supported discharge
• General practitioners doing most of secondary prevention
Stroke: Aggregated Audit Score:
Country Comparison
England
Northern Ireland
Wales
The Islands
10 20 30 40 50 60 70
Total organisational score 2006
80 90 100
Results: Stroke unit provision – comparison over time
Stroke unit in hospital
Median (IQR) stroke beds
Specialist community/ domiciliary rehabilitation team
2002
73%
20 (14-27)
31%
2004
79%
20 (15-29)
27%
2006
91%
24 (16-30)
2008
92%
25 (20-34)
32% 70%
Time from Stroke to Scan
250
200
150
100
50
0
0
500
450
400
350
300
4 8 12 16 20 24 28 32 36 40
Time from stroke to first brain scan (hours)
44 48
Time of Day Scanning Performed
1,200
1,000
800
600
400
200
0
0 2 4 6 8 10 12 14
24-hour clock
16 18 20 22 24
Thrombolysis Provision
Less than
24/7 off-site only, 1.5%
No provision,
11.9%
24/7 service provided onsite, 28.4%
Less than
24/7 on-site,
36.3%
24/7 service off-site only,
12.9%
24/7 service on-site and offsite, 9.0%
Intercollegiate Stroke Working Party
Thrombolysis Service
Thrombolysis
National median: 14
National total: 3284
Intercollegiate Stroke Working Party
National Initiatives for Change
NAO 2005
National Stroke
Strategy 2007
Stroke Improvement Programme
National Sentinel
Audit 2008
NICE and ICWP
Stroke Guidelines
2008
Transforming Stroke Care in London
Case for change
Patients treated in a
Stroke Unit
%
Physiotherapist assessment within
72 hours of admission
%
90%
100 100
95 93
85 85 84 82
72
66 64
60
59 58
55
50
45 45 45
38
35
30
20
18 15
8
5 3
0 0
90% 84
100 100
75
82
90
26
91
75
94
68
87
43
49
57
70
43
29
64
32
68
75
87
53
73
96
63
61 65 64
Emergency brain scan within 24 hours of stroke
%
90%
79
95
70
93
100
89
65
34
70
100
75
91 91
45
64
81
74
52
90
77
38
83 86
28
59
76
77
57
70
69
In 2004 the Sentinel Stroke Audit showed that stroke services in London were poor…
11
11
More strokes occurred in outer London but most providers were in inner London
GAPS
OVERLAPS
GAPS
GAPS
The more intense the red the greater number of providers available to provide service to the area.
12
Story so far
The development of the strategy was subject to wide engagement with the model of care agreed by clinicians and user groups
*
New acute model of care
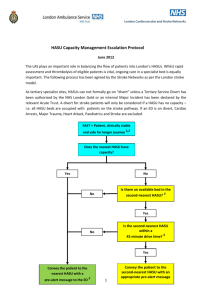
999
30 min
LAS journey*
HASU
After 72 hours
SU
Discharge from acute phase
Community
Rehabilitation
Services
HASUs
• Provide immediate response
• Specialist assessment on arrival
• CT and thrombolysis (if appropriate) within 30 minutes
• High dependency care and stabilisation
• Length of stay less than 72 hours
Stroke Units
• High quality inpatient rehabilitation in local hospital
• Multi-therapy rehabilitation
• On-going medical supervision
• On-site TIA assessment services
• Length of stay variable
Prophets of doom predictions
• It would not be possible to implement major system reorganisation in London for a condition as complex as stroke
• Staffing requirements would not be achievable
• Patients would not accept being taken to a hospital that is not local to them
• It would not be possible to transport people within 30 minutes to a HASU
• Repatriation would fail and HASUs would quickly become full
• Trusts would fight to retain services
• Even if acute services work it would fail because it would be impossible to change community services
• The new model would be unsustainable
Following bidding and evaluation a preferred model was agreed and consulted on
15
London Stroke Care: How is it working?
• 1 st February 8 Hyperacute (HASU) stroke units opened taking all patients who might be suitable for thrombolysis
• 19 th July all stroke patients taken to one of the
HASUs
• Over 400 additional nurses and 87 additional therapists recruited to work in stroke care in
London by July 2010
The number of stroke patients taken by London
Ambulance Service to a HASU has been increasing as implementation progresses
100%
90%
80%
70%
60%
50%
40%
30%
20%
10%
0%
O ct
-0
9
N ov
-0
9
D ec
-0
9
Ja n-
10
Fe b-
10
M ar
-1
0
A pr
-1
0
M ay
-1
0
Ju n-
10
Ju l-1
A ug
-1
0
0
- i nd ic at iv e
Non-HASU
HASU
17
Performance data shows that London is performing better than all other SHAs in England
Thrombolysis rates have increased since implementation began to a rate higher than that reported for any large city elsewhere in the world
16%
14%
12%
10%
8%
6%
4%
2%
0%
3.5%
10%
12%
Feb – Jul 2009 AIM Feb – Jul 2010
% of TIA patients’ treatment initiated within 24 hours
% of patients spending 90% of their time on a dedicated stroke unit
60
55
50
45
40
75
70
65
90
85
80
London
England
Target
Q1 Q2
2009/10
Q3 Q4 Q1
2010/11
70
65
60
55
50
45
40
90
85
80
75
Q1 Q2
2009/10
Q3 Q4 Q1
2010/11
London
England
Target
18
Efficiency gains are also beginning to be seen
HASU destination on discharge Average length of stay
10
8
6
4
2
0
20
18
16
14
12
Apr May Jun Jul Aug Sep Oct Nov Dec Jan Feb Mar Apr May Jun Jul Aug
2009/10 2010/11
60%
50%
40%
30%
20%
10%
0%
Home Other Stroke Unit RIP (blank)
• The average length of stay has fallen from approximately 15 days in 2009/10 to approximately 11.5 days in 20010/11 YTD
• This represents a potential saving of approximately [DN - insert figure]
• Approximately 35% of patients are discharged home from a HASU. The estimate at the beginning of the project was 20%.
19
London Stroke Care: How is it working?
• No significant problems with repatriation to
SUs. Good exchange of patient information.
• Significantly improved quality of care in SUs
• Evidence of constructive collaboration between hospitals
– SU Consultants joining HASU rotas and participating in post-take rounds and educational meetings
• Very positive anecdotal patient feedback
Areas where issues remain
• Community services in many areas still insufficient
– Early supported discharge
– Longer term rehabilitation
– Vocational rehabilitation
• Collecting data to prove the model is worth it
The Future
• Reorganisation of health care in UK with less central control
– Abolition of strategic health authorities
– General practitioners commissioning care
• May mean that major changes to stroke care will be difficult
• Probably funding cuts