Barnard.Lake Morey. Difficult to Manage symptoms
advertisement
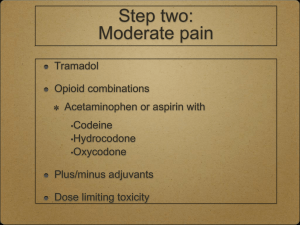
Dr. Diana Barnard Dr. Ursula McVeigh Review common causes and presentations of Nausea, Vomiting, Bowel obstruction, and Pain Crisis Review practical approaches to symptom management Provide opportunity for dialogue and questions Improve the quality of care and decrease the frustrations of care providers! Review causes of N/V Review different medication classes based on etiology Review etiology of bowel obstruction Review medication and non medication management Wood G et al. Management of Intractable Nausea and Vomiting in Patients at the End of Life: “I Was Feeling Nauseous All of the Time . . . Nothing Was Working” JAMA. 2007;298(10):1196-1207. Wood G et al. Management of Intractable Nausea and Vomiting in Patients at the End of Life: “I Was Feeling Nauseous All of the Time . . . Nothing Was Working” JAMA. 2007;298(10):1196-1207. Cause: Vestibular Motion sickness Mediated thru Cholinergic, histamine receptors Treatment Limit triggering movement Anti-cholinergic-Scopolamine patch –one every 3 days Anti-histamines- Diphenhydramine, Promethazine, Meclizine Requires medications that cross the blood:brain barrier and are therefore sedating- meclizine 12.5-25 mg Low dose benzodiazepines also may be helpful- ativan .5mg of valium 2.5 mg due to anxiety triggering component Cause: Opiods Common with initiation or dose escalation and often resolves within 3-5 days. Stimulation of the Chemoreceptor Trigger Zone (CTZ) Gastroparesis Constipation Treatment of Opiate related N/V Switch Opiates –limited benefit for some Pre-medicate, or once present –treat agressively around the clock with meds ; then taper back as tolerated Metoclopromide (Reglan) D2 receptor in GI tract Dose range is 5-20 mg qid before meals and at bedtime. Haldol – effective and under-utilized D2 receptor in CTZ Dose range is 0.5-2.o mg PO/intensol/SQ/IV every 6 hours Non sedating at lower doses Prochlorphenazine (compazine) D2 receptor in CTZ Dose 10mg PO or 25 mg PR every 6 hours Bowel stimulants Senna dose range 2-12 tabs per day) Miralax 17 grams per day and taper up Cause: Metastatic or primary disease in the brain Leads to increased intracranial pressure Meningeal irritation causes release of hormones which trigger the CNS vomiting center Treatment Steroids. Start with generous dose (e.g dexamethasone 8 mg bid) and taper down over days to weeks depending on effect and prognosis Steroids work fast, effect can be dramatic Radiation Therapy can also have fast, dramatic effects on N/V and other CNS symptoms associated with Edema in /around the brain. Cause: Chemotherapy related N/V 5HT3 released in gut CTZ stimulation Anxiety which triggers central pathways Treatment-premedicate Dexamethasone 2-8 mg po on day of chemo Ondansetron (Zofran) 4-8 mg PO or IV every 4-8 hours 5HT3 antagonist Lorazepam (ativan) 0.5-2.0 mg PO/intensol/SL/IV every 4-8 hours Cause: Constipation Treatment Diagnose by history and exam ( rectal exam, x-ray) First, relieve existing constipation Stimulants- Miralax, lactulose, MOM, enemas, suppositories Prevent future Constipation Colace (stool softener)is NOT enough Goal is normal BM frequency for patient of every 1-2 days Senna 2 tabs PO bid-taper up to 6 tabs bid Miralax 17 grams 1-2 times a day Taper meds until goal is consistantly achieved; taper down but DO NOT stop if diarrhea developes Patient education , tracking BMs very important Cause: Bowel obstruction Most common with colon, ovarian cancer Presents with nausea, vomiting and PAIN Identify most likely cause and location Ileus- is it temporary or reversible? Partial SBO- could there be disease progression? Transition Point tumor/mass in intestine Due to diffuse intra-abdominal tumor, ascites All trigger CTZ, 5HT3 Treatment Meds more likely to be effective in partial obstruction Goal is to reduce bowel distension, spasm Metoclopromide trail (5-20 mg qid)- only if PARTIAL Steroids to reduce inflammatory response (Dexamethasone 8 mg po bid ; taper if effective, d/c if not effective Haldol 0.5-4.0 mg PO/Intensol/SC/IV every 6 hours Good Pain control with opiates Octreotide 50-100 micrograms SQ/IV TID; long term IM depo form Mimics somatostatin to decrease secretions, reduce paristalsis Very expensive- useful in carcinoid related diarrhea; efficacy in obstruction and use in non tertiary care centers lacking If complete obstruction Surgery can be effective but burdensome. Not appropriate for limited life expectancy (<2 months) due to lack of success, complications, poor healing NG tube effective often necessary for immediate relief Effective, bothersome, requires suctioning Venting G Tubes for small bowel obstruction Stents for Esophageal, gastroduodenal or Large Bowel obstruction REMEMBER: Goals of care Accurate Prognosis Informed consent (understanding of risks, benefits, alternatives) Shared Decision Making vitale, chalanging Concept of I want to live vs. I want to live for an event Venting G tubes- Increasingly offered for SBO Benefits Non surgical procedure Comfort without a tube in your nose Allows some po intake- range of possibilities If early in illness, can be clamped, allow absorption of nutrients, building “strength” Burdens TIME in or out of hospital IR procedure (lab draw, medication, waiting) Healing delayed / impaired in presence of ascites Gastrointestinal stents for focal intestinal cancers Benefits non surgical treatment Effect can be long lasting; depending on prognosis Early in non operable presentation, allows intake of a more “regular” diet symptom relief can be dramatic, last a while Burdens Requires endoscopy/colonoscopy, with GI prep, sedation Effect is time limited as disease progresses Risks: TIME, migration, perforation, partial relief of symptoms Availability in hospitals variable and limited by experience of GI providers PEARLS: Consider etiology of N/V/Obstruction Pre-medicate Opiates with anti-emetics Don’t forget CONSTIPATION Many causes are multi-factorial; use what has worked If one class of medication is not working, switch classes Think about non pill form (PR, Liquid, ODT) Haldol is a very useful medication Obstructive symptoms are challenging, difficult to manage, possibly becoming more common For Intractable symptoms, remember to focus on the GOALS of care…Is going to the hospital a good or bad thing??? An EMERGENCY which requires rapid response A patient in pain will have limited capacity to consider any other issues until pain is well managed Clear principles and guidelines exist in the literature 2009 NCCN Guidelines Side effects can be avoided and/or managed Very different from Chronic pain management Effective communication is key Patient, family, care staff, prescribing provider GOAL: Rapid symptom relief BASIC PAIN PRINCIPLES APPLY Give repeated doses until comfort reached Re-evaluate OFTEN Calculate total dose needed to achieve comfort and then dose on a schedule, monitor effect UNDERtreatment is as concerning as OVERtreatment SEDATION comes before Respiratory depression Reference and follow established guidelines If opiate naïve give 2-5 mg morphine IV; recheck in 15 minute Give 5-15 mg PO; recheck in 1 hr Time frame for peak therapeutic effect AND peak sideeffects If on regular opiates Calculate total use in past 24 hours and give 10-20% of this dose (TDD) PO or IV and reassess 10-20 % TDD IV Reassess at peak IV: 15 minutes; PO: 1hr No Change in Pain Increase dose 50%- 100% and reassess IV 15 min/PO 1hr Some relief Repeat same dose And reassess: Pain decreased 50% Reassess 2-3 hrs IV 15 min/ PO 1hr National Comprehensive Cancer Network Cancer Pain Guidelines 2009 Tools for success: Be deliberate, use guidelines, monitor your patient Don’t be irrationally afraid of overdosing Re-evaluate dose and effect frequently Use the medication you are most familiar with; be willing to try something new if not effective For PO meds, use short acting medications for crisis, then add long acting forms for more even effect If on IV infusion, once basal rate has started remember it takes 5 half lives to reach steady state (MS4 and HM = 10 hrs), so additional boluses will be needed in the interim ORAL medication route: Continue long acting scheduled medications PRN doses for breakthru pain should be 10-20% of the total daily dose on a routine basis In a pain crisis, increase the scheduled dose by 50-100% and give extra doses of prn medication, until comfort achieved. Convert total dose into new scheduled medication dosing and INCREASE breakthru dose accordingly PCA guidelines (IV, SQ) SQ route highly effective; requires coordination SQ rate limit is 2 cc per hour Start with basal rate based on previous 24 hour need Demand dose should be EQUAL to basal rate Demand dose can be offered every 10 minutes Total hourly dose can be “locked out” It will take about 8 hours for basal rate to have effect Additional bolus doses will be needed until then PCA doses may be used more in first hours Rapid dose escalation issues Always consider acute /reversible cause for pain crisis One change at a time helpful for cause/effect, but rapid response may require multiple changes Pain may be “total pain” or psychic pain Adding anxiolytics (e.g ativan) very helpful .5-2 mg PO every 4-8 hours scheduled or as needed Rotating / switching narcotics may be helpful Calculate equivalent dose, then 30-50% dose reduction for incomplete cross tolerance. “Intolerance” Asses symptom carefully; consider dose adjustment before changing opiates too quickly Sedation More common when opiate naïve Occurs well before respiratory depression Decrease dose 20% ; cautiously more to avoid uncontrolled pain Nausea Pre-medicate for first few days Constipation Avoid first; if present, treat aggressively Intolerance of dose form Consider patch, intensol, subcutaneous Rectal forms can be compounded Limited research available for topical dosing Opioid toxicity More likely with large doses, rapid escalation Includes hyperalgesia, twitching, myoclonus, seizures, delirium Consider hydration if c/w GOC Decrease dose (25%) or rotate opiates Add Lorazepam to suppress myoclonus if sedation OK/EOL Consider and document reasons for switching Use Equal Analgesic tables for conversion Different charts/tables exist They are meant as a guide, NOT absolute conversion like a measurement ( 1 cup = 8 ounces) Patients vary in response to different opiates Decrease total equal analgesic dose by 30-50% for incomplete cross tolerance Check and recheck your math! Re-evaluate frequently for best practice “dose finding” MORPHINE IR/ER/Intensol/SQ/IV Many fears, bad experiences, family stories No such thing as a good drug or bad drug If persistant fear, chose something else Particularly useful in dyspnea, but likely a class effect Itching, nausea, fuzzy-headedness at age 2o with wisdom teeth are not symptoms of allergies. Hydromorphone Preferred drug at FAHC for renal impairment which causes accumulation of metabolites… but occurs with many meds IV/PO, no intensol formulas, new long acting formula Oxycodone Avoid combination with Tylenol to limit toxicity as doses are increased ER,IR, intensol formulas NO IV formula High street value, especially in Oxycontin form Should not stop appropriate use Careful monitoring of amounts of medication- especially with frequent dose changes Remind patients about safety (accidental or intentional diversion) FENTANLY IV/patch forms. Various po forms – safety issues Patch can be beneficial for stable medication effect and to avoiding po meds Lipophillic so best to have subcutaneous fat for reservoir. Takes 12 plus hours to have some effect Takes 24 hours to get to steady state AND to leave the body if poorly tolerated Expensive, especially if using two patches ?less constipating ?less nauseating Methadone Most practitioners have a DEA license to prescribe for PAIN, not for ADDICTION Cheap Effective, especially for neuropathic pain Pharmacokinetics –long time to steady state (3-7 days), very long half life so dose changes must be SLOW Can be high risk; requires experience Not commonly used Like Oxycontin (and all narcotics), has high street value PO IV Morphine 30mg 10mg Hydrocodone 60mg Hydromorphone 7.5mg Oxycodone 20mg Codeine 200mg Fentanyl 1.5mg 100 mcg Route Onset (min) Peak (min) Duration of T ½ effect (hrs) (hr) SS IV 5 10 1-4 2 8 PO 30 60 3-4 3 3 8 1-4 2 PO 20 100 3-4 3 Oxycodone PO 20 60 3-4 3 Fentanyl IV <1 6 3-4 3 TD 6-12 hr 1-3 d IV 15 60 4 PO 60 120 6 Morphine Hydromorphone IV Methadone 8 4d 8-60 2d12 Trescot. Opioid pharmacology. Pain Physician, 2008 Dose Cost/month Methadone 5mg po TID $10 Morphine ERT 60mg BID $200 Fentanyl TD 50mcg/hr q3d $240 Oxycontin ERT 40mg BID $420 CRI HD Notes Fentanyl OK OK Limited data Not dialyzed Methadone OK OK Not dialyzed Hydromorphone Caution Caution Lower dose, longer interval Oxycodone Caution Caution Poor data Morphine Avoid Avoid active metab Codeine Avoid Avoid Active metab Dean, Opioid in Renal Failure and Dialysis Patients. JOSM, 2004 Normal Cirrhosis Notes T 1/2 T 1/2 Fentanyl 263 min 304 min No change Drug of choice Methadone 11-35 hr 11-35 hrs ↓dose w/ svr failure Hydromorphone 2.5 no data ↓ dose Morphine 3 hr 5 hr ↓ dose Oxycodone 3 hr 14 hr ↓ dose and freq. Rhee, Palliation and Liver Failure: Palliative Medications Dosage Guidelines. JPM, 2007