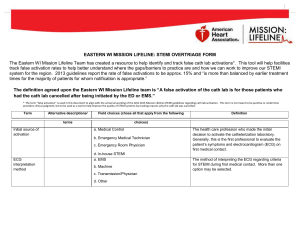
ACS Diagnostics
advertisement
DIAGNOSTICS OF Acute Coronary Syndromes At the end of this self study the participant will: • Verbalize meanings of specific ECG changes: – ST Elevation – ST Depression • Describe common tests used for patients with suspected Acute Coronary Syndromes 1 Abbreviations: • ACS = Acute Coronary Syndrome • STEMI = ST Elevation Myocardial Infarction • AMI = Acute Myocardial Infarction • PCI = Percutaneous Coronary Intervention (e.g., angioplasty, stents) 2 Time is Still Muscle! 4 D’s of Timely Reperfusion • • • • Door to Data (ECG) Door to Decision Door to Drug Door to Dilatation Goal < 10 min. Goal < 20 min. Goal < 30 min. Goal < 90 min. • Door can be time of patient arrival, or time the patient tells nursing staff of possible ACS signs and symptoms 3 Door to Data: 10 minutes • INITIAL DIAGNOSIS – 12-LEAD ECG • ST Elevation – ST elevation MI (STEMI) – All High Risk • No ST elevation – Acute Coronary Syndrome OR Non ST elevation MI (Non STEMI) » High, Intermediate or Low Risk 4 Lead Placement to obtain a 12lead. V lead (chest lead) placement must be exact. 5 Normal 12 Lead EKG Configurations In order to more easily recognize abnormalities in the 12 lead ECG one must first be able to recognize the normal 12 lead ECG Look for: •Flat baseline •Little to no artifact (waveforms are clear) 6 12-lead changes seen in ACS ~ 2.0 MM patients admitted to CCU or telemetry annually ST Elevation 0.6 MM ST-elevation MI 7 ST depression 1.4 MM Non-ST elevation ACS T wave inversion Ischemia 8 Injury 9 ECG Progression in AMI ST-segment elevation may occur within the first few hours of infarction. ST-segment elevation is indicative of injury that is leading to infarction. When ST-segment elevation is seen, time is limited and the healthcare provider must act quickly to initiate a reperfusion strategy in order to salvage the most myocardium. 10 From Garcia, et.al. (2001). 12 Lead ECG. The Art of interpretation, pg. 408. Used by permission. Non-diagnostic ECGs • According to the National Registry of Myocardial Infarction, only 39% of Acute MI patients have STEMI on admit • Subsequent STEMI occurs within 12 hrs of symptoms • Acute MI patients who present & maintain normal or nonspecific ECGs have lower mortality rates; Increased mortality risk associated with development of STEMI Fesmire, FM, et al. Ann Emerg Med. 1998: 31: 3-11. Littrell, KA, et al. JACC. 2001: 37 Suppl A p. 1282-101. French, WJ, et al. NRMI 4 Special Report, June 2001 Welch, RD, et al. JAMA, 2001: 286: 1977-1984. 11 Door to decision: 20 minutes • Based on ECG and patient presentation • Does not require lab data nor advanced assessments such as angiography (cardiac catheterization) • If decision is AMI, treatment planned – Door to Drug 30 minutes – Door to Dilatation (PCI) 90 minutes • If decision is not AMI, further evaluation is required 12 ACS DIAGNOSIS • CARDIAC ENZYMES – Negative • Unstable Angina • Non-cardiac? – Positive • MI 13 Serum Enzyme Changes Onset Peak Time CPK-MB 4-6 hours 12-24 hours 2-3 days Troponin-I 4-6 hours Myoglobin 1-2 hours 12-24 hours Up to 10 days 4-6 hours 24 hours 14 Duration Diagnostic Tests Echocardiogram evaluates: • Wall motion and valve function • Ejection fraction (EF) – % of blood pumped out of ventricle with each beat – normal = 60-70%; – failure = < 40% – The greater the damage, the greater the muscle loss, the lower the EF 15 Diagnostic Tests Stress Testing: only performed if enzymes are negative. • ECG • Perfusion Studies (indicate capillary perfusion = better predictor) – Exercise Thallium – Dobutamine Stress Echo – Adenosine Thallium 16 Cardiac Catheterization (Angiography) • Access: radial, brachial or femoral arteries If we can upload from YouTube, there’s a terrific video (no audio) of a cath http://www.youtube.com/watch? v=yzxSrLa1d0g 17 Photo under fluoroscopy 18 Possible Post-Cath Complications • • • • • 19 Hypotension Active Bleeding Limb Ischemia Recurrent Ischemia/MI Arrhythmias: Ventricular and Bradycardia • Contrast Reaction • Contrast Nephropathy • Congestive Heart Failure • Neuro Deficits Post Cath Care Sheaths are used with all PCI’s – Assess for bleeding at site, and under the site; outline ecchymotic areas – Note any perfusion changes around site – Palpate abdomen for firmness or distention – Be alert to changes in oxygenation assessment and hemodynamic status • If bleeding is seen at site, place immediate manual pressure • Monitor peripheral pulses 20 Next: ACS Treatments 21