Peripheral Nerve Stimulation in
Trigeminal Neuralgia
Department of Neurosurgery, Massachusetts General Hospital
Grand Rounds
Nikhil Agrawal
MD Candidate
Brief Case Presentation
HPI: 56y M with history of HTN, depression/anxiety, right sided refractory
facial pain (V1 distribution) for 8 years s/p microvascular decompression, RF
rhizotomy, supraorbital alcohol injection, and left motor cortex stimulator
PMH: Anxiety , Depression, HTN, Trigeminal Neuropathic Pain
Exam: Intact
Pre-op Diagnosis: Severe medically intractable right-sided facial
pain.
Operation: Placement of right-sided cranial stimulators.
Post Operative Course: Patient feels significant relief from pain
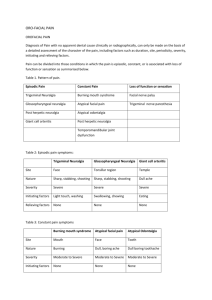
Burchiel Classification of Facial Pain
Spontaneous Onset
• TN Type 1 (Classic TN)
– > 50% episodic pain
• TN Type 2 (Atypical TN)
– > 50% constant pain
Trigeminal Injury
• Symptomatic TN (Multiple sclerosis)
• Trigeminal neuropathic pain (post-traumatic)
• Trigeminal deafferentation pain (RF lesion, GKR, etc.)
• Post-herpetic facial pain
• Secondary TN
– Tumors, aneurysm, AVM, etc.
• Atypical facial pain (somatiform pain disorder)
Trigeminal Neuralgia
Etiology
• Exact cause unknown
• Maxillary and mandibular sensory branches affected
• Four Theories
-Constant pressure causing irritation from the
superior cerebellar artery
- infections from herpes virus, teeth, or brainstem infarct
-Multiple Sclerosis
-Tumor causing pressure and irritation
Surgical Treatment of TN
• Microvascular decompression (MVD)
• Percutaneous ablative procedures
– Radiofrequency gangliolysis
– Glycerol rhizolysis
– Balloon compression
• Stereotactic radiosurgery
– Gamma knife
– Linac-based
• Peripheral ablative procedures (V1 and V2 pain)
– Peripheral branch neurectomy
– Alcohol neurolysis
• Open destructive procedures
– Partial sensory rhizotomy
– Subtemporal ganglionectomy (Frazier-Spiller procedure)
• Peripheral Nerve stimulation
© Slavin et al., 2007
MVD vs. Percutaneous Procedures
INITIAL PAIN RELIEF
• MVD
• RF rhizotomy
• Balloon
• Glycerol
98%
98%
93%
91%
RECURRENCE RATES
• Glycerol
• RF rhizotomy
• Radiosurgery
• Balloon
• MVD
54% (4 years)
23% (9 years)
25% (3 years)
21% (2 years)
15% (5 years)
Taha J, Tew J: Neurosurgery 38:865—871, 1996
MICROVASCULAR DECOMPRESSION SURGERY IN THE
UNITED STATES, 1996 TO 2000: MORTALITY
RATES,MORBIDITY RATES, AND THE EFFECTS OF
HOSPITAL AND SURGEON VOLUMES
• The authors demonstrate that the mortality
associated with MVD is significantly lower when
performed by high volume surgeons and that
morbidity is lower for high-volume surgeons and
high-volume hospitals.
• Overall mortality was low (0.3%)
Kalkanis SN, Eskandar EN, Carter BS, Barker FG 2nd.Neurosurgery 52:12511262, 2003
Peripheral Stimulation: Facial
pain
Most Common technique:
◦ Occipital Nerve Stimulation
Occipital stimulation
“BOTH” stimulation
Other techniques:
◦ Trigeminal branch stimulation
Supraorbital
Supratrochlear
Auriculotemporal
Trigeminal Branch Stimulation
• Stimulation of supraorbital, infraorbital nerves
• Indications
–
–
–
–
Trigeminal neuropathic pain
Trigeminal deafferentation pain
Post-herpetic neuralgia
Chronic daily headache
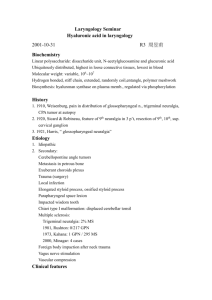
Summary of Cases
Case
Age/Sex
Pre-op Diagnosis
Duration of
Sympto
ms
Trigeminal
Branch
Pain Relief
Follow Up
Duration
1
71/M
TNP :Secondary to
enucleation
11 years
V1 and V2
100%
27 months
2
52/M
TNP :Secondary to
zygomaticomaxillary fracture
18 months
V1 and V2
100%
23 months
3
44/M
Postherpetic neuralgia
18 months
V1
60%
6 months
Stidd DA, et al . Pain Physician. 2012 Jan-Feb;15(1):27-33
Peripheral Trigeminal Branch Stimulation for
Neuropathic Pain
Johnson M, Burchiel K, Neurosurgery, 2004
5
6
4
4
2
3
0
0
25
Pain Relief
8
6
4
2
0
50
75
100
2
1
Increase
No
Reduced
Change
Post Operative Medication Use
0
Slightly
Somewhat
Mostly
Patient Satisfaction Rating
Completely
Peripheral Trigeminal Branch
Stimulation for Neuropathic Pain
• Effective for trigeminal
neuropathic pain
• Less effective for PHN
• Simple, low morbidity
• Pain relief seems relatively
durable
• Major problem is erosion of
connector
Conclusion
• “Though there are no randomized trials,
peripheral neuromodulation has been shown to
be an effective means of treating TNP
refractory to medical management in a growing
number of case series. PNS is a safe procedure
that can be performed even on patients that are
not optimal surgical candidates and should be
considered for patients suffering from TNP that
have failed medical management.”-Dr Stidd
References
1.Loeser, J.D. Tic douloureux and atypical facial pain, In: Wall PD, Melzack R, eds.
Textbook of Pain. 3rd edition. Edinburgh: Churchill/Livingstone, 1994: p 699710.
2. David A. Stidd, MD1, Adam Wuollet, MD1, Kirk Bowden, DO1, Theodore Price
PhD1, Amol Patwardhan, MD, PhD1 Pain Physician 2012; 15:27-33
3.Madland G. and C. Feinmann, Chronic facial pain: a multidisciplinary problem. J
Neurol Neurosurg Psychiatry, 2001;71:p. 716-719.
4. Osenbach, R., Neurostimulation for the Treatment of Intractable Facial Pain. Pain
Medicine. 7(s1).
5. Johnson, M. and K. Burchiel, Peripheral Stimulation for Treatment of Trigeminal
Postherpetic Neuralgia and Trigeminal Posttraumatic Neuropathic Pain: A Pilot
Study, 2004: 55(1): p. 135-142.
6. Broggi G, Ferroli P, Franzini A, Servello D, Dones I: Microvascular decompression
for trigeminal neuralgia: Comments on a series of 250 cases, including 10
patients with multiple sclerosis. J Neurol Neurosurg Psychiatry68:59–64, 2000.
7.. Burchiel KJ, Clarke H, Haglund M, Loeser JD: Long-term efficacy of
microvascular decompression in trigeminal neuralgia. J Neurosurg 69:35–
38,1988.
Special Thanks To:
•
•
•
•
•
•
Dr. Emad N. Eskandar
Dr. Daniel Cahill M.D. Ph.D.
Dr. William Curry, M.D.
Dr. Jean-Valéry Coumans, M.D.
Dr Pankaj K. Agarwalla, M.D.
Dr. Matthew Mian, M.D