Febrile Neutropenia
Mervat Hesham
2009
Febrile Neutropenia
•
•
•
•
•
Who should receive empirical Rx?
When should empirical Rx be started?
What is appropriate initial Rx?
How should initial Rx be modified?
How long should empirical Rx be
continued?
Febrile neutropenia
*Fever
Single oral temperature > 38.3ºC
OR
– 38º C for more than 1 hour
*Neutropenia
– Neutrophils< 0.5x109/L (500/mm3)
OR
– Neutrophils <1.0 x109/L, predicted fall to < 0.5 x
109/L
• Tympanic temperature (oral temperatures may be falsely
high in presence of mucositis)
Neutropenia: (ANC)
mild
moderate
Severe
1.0 to 1.5 x 103/l
0.5 to 1.0 x 103/l
<0.5 x 103/l
Possible sites of infection
•
•
•
•
•
•
•
•
•
URTI
Dental sepsis
Mouth ulcers
Skin sores
Exit site of central venous catheters
Anal fissures
GIT
marrow aspiration sites
nails and nail peds, scalp
Factors Associated with Increased
Risk of Infection
• Duration and severity of neutropenia
• type and intensity of chemotherapy
• altered phagocytic, cellular and humoral
immunity
• breaches of skin and mucosal barrier
• catheter or other foreign bodies
• underlying diseases or therapy
• corticosteroids
Pathogens
• 60% - 70% of fevers during neutropenia have
no identifiable etiology i.e fever of unknown
origin.
• Bacteremia seen in 10%- 20% of patients with
fever and neutrpenia,
Gram positive bacteremia 70%
Gram negative bacteremia 30%
Common pathogen in neutropenia
Bacteria:
Gram positive organisms
• Staphylococcus aureus
• Coagulase-negative staphylococcus
• alpha and beta hemolytic streptococcus
Gram negative organisms
• Escherichia coli
• Klebsiella pneumoniae
• Pseudomonas aeruginosa
Fungi:
• Candida , Aspergillus
Febrile Neutropenia Evaluation:
• A. General measures:
Attempt to reduce acquisition of resistant hospital
pathogens in neutropenic patients by using the
following precautions:
• 1. Single-bed room (“protective isolation”).
• 2. Wash hands with antibacterial soap prior to all
patient contact.
• 3. No live plants.
• 4. Limit visitors.
• 5. Meticulous skin care, especially IV catheter sites.
• 6. Foley catheters, rectal thermometers, and
suppositories should be avoided.
• B. Avoid routine use of antipyretics and
corticosteroids so that temperature trends
and response to antibiotics can be
monitored. Acetaminophen may be used for
discomfort associated with fever.
• C. Examine the patient frequently
History :
(cycle/course of chemotherapy,prophylactic
agents, corticosteroids , immunosuppresive
agents,previous infections or procedures).
• Physical examination :
*Signs(perianal erythema and tenderness,
Minimal erythema or serous discharge at the site
of a Hickman catheter, Signs & Symptoms of
Sepsis
(any one or more of the following
signs):
1. Hyperpyrexia (Temperature > 104oF).
2. Hypothermia (< 96oF).
3. Chills not associated with transfusions or
drugs
4. Hypotension (BP change > 30% or SPB
< 90 mmHg; refer to age specific guidelines
for children).
5. Hypoxemia (O2 saturation < 90% or >
5% change from baseline).
6. Moderate/severe End Organ
Dysfunction (increased Scr or LFTs).
7. Altered Mental Status.
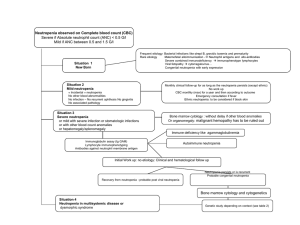
D . Risk assessment:
•
•
•
•
•
•
•
•
•
•
•
Low risk:
ANC > 100 /mm3 ,
Normal CXR ,
Duration of neutropenia < 7 d,
Resolution of neutropenia <10 d,
No appearance of illness,
No comorbidity complications ,
Malignancy in remission.
High risk :
ANC < 100 /mm3 ,
Duration of neutropenia > 7 d .
ُُE . Investigation
• Full Blood Count
-White cells, haemoglobin, platelets
• Biochemistry
-Electrolytes, urea, creatinine, Liver function
• Microbiology
-Blood cultures (peripheral and all central line lumens)
-Exit site swabs
-Wound swabs
-Urine analysis and culture.
-Stool analysis and culture.
-+/- Cerebrospinal fluid
• Radiology
Baseline chest X-ray and any other X-ray indicated by exam. -+/- CT
abdo/pelvis
• F. Re-evaluate the patient daily (or more
often if clinically indicated) for localizing
signs of infection and for response to
therapy. Unless the patient’s clinical status
changes, allow at least 48 hours prior to
modifying antibiotics.
• G. Be alert for reappearance of fever in a
patient who initially defervesces. This may
indicate superinfection with resistant
bacteria or with fungi.
Empirical Antibacterial Therapy
Empiric antibiotic therapy Broad spectrum
empiric antibiotic therapy must be started
properly prior to organism identification.
Survival is greater than 90% when patients
are treated with appropriate empiric
therapy.
Initial Empiric Antibiotics
Rationale
• Severe risk of bacterial sepsis
• Insensitivity of diagnostic tests
• Delays in identification of pathogens
Febrile Neutropenia
•
•
•
•
•
Who should receive empirical Rx?
When should empirical Rx be started?
What is appropriate initial Rx?
How should initial Rx be modified?
How long should empirical Rx be
continued?
Initial Empiric Antibiotics
Considerations
•
•
•
•
•
•
•
Broad spectrum of bactericidal activity
Local prevalence, susceptibility pattern
Antibiotic toxicity : well-tolerated, allergy
Host factors : severity of presentation
Prior antibiotic usage
Antibiotic costs
Ease of administration
Initial Empiric Antibiotics
Recommended choices
• Monotherapy
• Duotherapy without vancomycin
• Vancomycin plus one or two drugs
Oral Antibiotics and Outpatient
Management
• Current studies : potentially be safe
and effective in low-risk patients
Monotherapy
Choices
• Ceph 3 : ceftazidime
• Ceph 4 : cefepime
• Carbapenem : imipenem , meropenem
IDSA guidelines-2002
Combination Therapy
Advantages
•
•
•
•
Increased bactericidal activity
Potential synergistic effects
Broader antibacterial spectrum
Limits emergence of resistance
Combination Therapy
Disadvantages
•
•
•
•
Drug toxicities
Drug interactions
Potential cost increase
Administration time
Combination Therapy
Choices
• Aminoglycoside + Anti-pseudomonal
carboxypenicillin
• Aminoglycoside + Anti-pseudomonal
cephalosporin
• Aminoglycoside + Carbapenem
Vancomycin as Empiric Rx
When to use ?
• Known colonization with MRSA or PRSP
• Clinically suspected serious catheterrelated infections (eg bacteremia)
• Hypotension or cardiovascular impairment
• Initial positive results of blood culture for
G+ bacteria
Febrile Neutropenia
•
•
•
•
•
Who should receive empirical Rx?
When should empirical Rx be started?
What is appropriate initial Rx?
How should initial Rx be modified?
How long should empirical Rx be
continued?
Initial Antibiotic Modifications
Considerations
•
•
•
•
Persistence of fever
Clinical deterioration
Culture results
Drug intolerance/side effects
Persistent Fever
Causes
•
•
•
•
•
•
Nonbacterial infection
Resistant bacteria
Slow response to antibiotics
Fungal sepsis
Inadequate serum & tissue levels
Drug fever
Persistent Fever > 5 Days
Choices of Mx
• Continue initial Rx
• Change or add antibiotics
• Add an antifungal drug(Ampho B)
Febrile Neutropenia
•
•
•
•
•
Who should receive empirical Rx?
When should empirical Rx be started?
What is appropriate initial Rx?
How should initial Rx be modified?
How long should empirical Rx be
continued?
Duration of Antibiotic Therapy
When to stop?
• No infection identified after 3 days of Rx
• ANC >
500 for 2 consecutive days
• Afebrile > 48 hr
• Clinically well
Empiric anti-fungal therapy
•
Give Antifungal therapy if
Prolonged neutropenic fever (>4 days) and on Broad spectrum
antibiotics
* Esophagitis , localized pulmonary infiltrate.
* Failure of treatment of diffuse pulmonary infiltrate by I.V TMP and
erythromycin .
* Sinus tenderness or nasal ulcerative lesion.
•
Rationale
Fungal infections difficult to diagnose
High mortality, excess morbidity with delays in treatment
•
•
Advantages
Fewer fungal deaths
Disadvantages
>50% of patients will be treated unnecessarily
Toxicity of antifungals and costs +++
Empirical antianaerobe therapy
• In perianal tenderness .
• severe oral mucositis and gingivitis,
acute abdominal pain ( typhilitis ,
appendicitis) .
Supportive measures in
febrile neutropenia
Colony Stimulating factors
(G-CSF, GM-CSF)
Colony Stimulating factors in
febrile neutropenia
• Theoretical benefits
Reduce duration neutropenia
Reduce severity neutropenia
Reduce hospital stay
Reduce duration antibiotic therapy
Reduce alterations in chemotherapy regimens (dosage and
timing)
Reduce infection-related mortality
Improve the effective delivery chemotherapy
Guidelines for use of CSF in
febrile neutropenia
• Primary prophylaxis
In chemo regimens with >40% risk of FN,
most cost effective
Consider in pre-existing neutropenia, poor
performance status, advanced malignancy
• Secondary prophylaxis
If previous profound neutropenia,
subsequent dose reduction preferred
rather than giving CSF support with
maximum intensity chemotherapy
Guidelines for use of CSF in
other clinical settings
• AML induction
– Reduced duration neutropenia
– No associated decrease in nadir, no reduction
hospital stay, antibiotic usage or mortality risk
– Trials esp in elderly variable
• Combined chemotherapy and radiotherapy
(mediastinal)
– Relative Contraindication: increased risk
thrombocytopenia
• Febrile neutropenia with complicated sepsis
– Adjuvant CSF given, benefit not confirmed
Hematopoietic growth factors :
(a) Patients already on growth factors should
continue on therapy if febrile neutropenia
develops. There is no rationale to increase
the dose.
(b) Patients not on a growth factor should not
be started unless certain prognostic factors
predictive of clinical deterioration are
present, including signs/symptoms of
sepsis, pneumonia, or fungal infection.
(c) Do NOT give growth factors if the patient is
receiving concurrent radiation therapy – a
more prolonged neutropenia may result.
Febrile Neutropenia
Conclusions
• Significant morbidity & mortality
• Choice of initial empiric therapy dependent
on epidemiologic & clinical factors
• Monotherapy as efficacious as
combination Rx
• Modifications upon reassessment
• Duration dependent on ANC
• Antipseudomonal penicillin
* I/V Piperacillin 200-300mg/kg/daily
( IV Divided q4–6h)
*I/V Ticarcillin
•
300mg/kg/daily
( IV Divided q4–6h)
Aminoglycosides
*I/V Gentamicin 6.0–7.5 mg/kg/daily.
(Loaded with 2mg/kg IV Divided q8h)
*I/V Amikacin 7.5mg/kg/12 hourly
( 15 mg/kg/day IV Divided q8h)
Monotherapy:
• Monotherapy with certain broad spectrum antibiotic
shown to be as effective as combination antibiotic
regimen for empiric therapy.
• Include,
• Ceftazidime (3rd generation cephalosporin)(
Fortum )
100–150 mg/kg/day IV Divided q8h
• Imipenam-cilastatin ( carbepenam )
I/V 12.5mg/kg/6 hourly
Meropenem
0–120 mg/kg/day IV Divided q8h
( maximum dose 6 g/day)
• Cefepime (4th generation cephalosporin) ( Maxipim)
50 mg/kg per dose IV Divided q8h
or I/V 1-2gm/ 8 hourly
Oral antibiotic therapy:
• Are acceptable for selective stable low risk
patients.
• Oral ciprofloxacin 750mg/8 hourly
plus
Amoxicillin/clavulanate500mg/8 hourly.
Antifungal therapy
• Amphotericin B (Fungizone)
IV Test dose 0.1 mg/kg to a
maximum dose of 1 mg over 1 hour; if tolerated, may use 0.4
mg/kg
and increase to 1 mg/kg/day
• Voriconazole( fevend )
IV, PO 6 mg/kg every 12 hours, IV for first 24 hours and then
4 mg/kg every 12 hours.
Oral dose:
>40kg, 200 mg bid, may increase to 300 mg bid,
<40 kg 100 mg bid, may increase to 150 mg bid
• Fluconazole ( diflucan )
IV, PO 2 mg/kg/day (maximum dose 600 mg/day)
( I/V or oral fluconazole 200mg loading dose then 100mg/daily for
10-14 days for candidiasis)
Antiviral therapy
• Acyclovir- (Zovirax) :Varicella in
immuno compromised host
*IV For children <1 year of age:
30 mg/kg/day in 3 divided
doses for 7–10 days; some
* IV For children >1 year of age:
1500 mg/m2 of body surface
area per day in 3 divided
doses for 7–10 days.
• Ganciclovir (Cytovene)
1- Acquired CMV retinitis in
immunocompromised Host
*IV 10 mg/kg/day in 2 divided
doses for 14–21 days;
*For long-term suppression, 5 mg/kg/day
for 5–7 days/week.
2- Prophylaxis of CMV in high-risk host :
IV 10 mg/kg/day in 2 divided doses for 1
wk, then 5 mg/kg/day in 1 dose for 100 days.
Anaerobic coverage:
• Metronidazole
30 mg/kg/day IV (divided q6h)
(loading dose initially 15 mg/kg)
• Vancomycin
40 mg/kg/day (maximum 2 g/day)
IV Divided q6–8h
• Clindamycin
40 mg/kg/day IV Divided q6–8h