mv-weaning - Mecriticalcare.net
advertisement
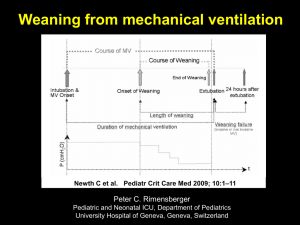
Weaning Modes and Protocol • Causes of Ventilator Dependence • Assessment for Discontinuation Trial • Spontaneous Breathing Trial (SBT) – Extubation Criteria • • • • • 2 Failure of SBT Weaning Modes Weaning Protocols Role of Tracheostomy Long-term Facilities Stages of Mechanical Ventilation 2 Causes of Ventilator Dependence Who is the “ventilator dependent’? • Mechanical ventilation > 24 h or • Failure to respond during discontinuation attemps 4 Causes of Ventilator Dependence Causes Description Neurologic controller Central drive Peripheral nerves Respiratory system Mechanical loads Ventilatory muscle properties Gas exchange properties Cardiovascular system Cardiac tolerance of ventilatory muscle work peripheral oxygen demands Psychological issues 5 Assessment for Discontinuation Trial Criteria for discontinuation trial: • Evidence for some reversal of the underlying cause for respiratory failure • Adequate oxygenation and pH • Hemodynamic stability; and • The capability to initiate an inspiratory effort 6 Assessment for Discontinuation Trial Extubation failure • 8-fold higher odds ratio for nosocomial pneumonia • 6-fold to 12-fold increased mortality risk • Reported reintubation rates range from 4 to 23% for different ICU populations 7 Assessment for Discontinuation Trial Criteria Used in Weaning/Discontinuation in different studies 8 Assessment for Discontinuation Trial Measurements used To Predict the Outcome of a Ventilator Discontinuation Effort in More Than One Study 9 Spontaneous Breathing Trial • Formal discontinuation assessments should be performed during spontaneous breathing • An initial brief period of spontaneous breathing can be used to assess the capability of continuing onto a formal SBT. 10 Spontaneous Breathing Trial • How to assess patient tolerance? – – – – 11 the respiratory pattern the adequacy of gas exchange hemodynamic stability, and subjective comfort. Spontaneous Breathing Trial Criteria Used in Several Large Trials To Define Tolerance of an SBT* *HR heart rate; Spo2 hemoglobin oxygen saturation. Spontaneous Breathing Trial • The tolerance of SBTs lasting 30 to 120 min should prompt consideration for permanent ventilator discontinuation 13 Spontaneous Breathing Trial Frequency of Tolerating an SBT in Selected Patients and Rate of Permanent Ventilator Discontinuation Following a Successful SBT* *Values given as No. (%). Pts patients. †30-min SBT. ‡120-min SBT. Do Not Wean To Exhaustion Weaning to Exhaustion • • • • • • • RR > 35/min Spo2 < 90% HR > 140/min Sustained 20% increase in HR SBP > 180 mm Hg, DBP > 90 mm Hg Anxiety Diaphoresis Mechanical Ventilation Rest 24 hrs PaO2/FiO2 ≥ 200 mm Hg PEEP ≤ 5 cm H2O Intact airway reflexes No need for continuous infusions of vasopressors or inotrops > 100 RSBI <100 Stable Support Strategy Assisted/PSV 24 hours Daily SBT Low level CPAP (5 cm H2O), Low levels of pressure support (5 to 7 cm H2O) “T-piece” breathing 30-120 min Yes RR > 35/min Spo2 < 90% HR > 140/min Sustained 20% increase in HR SBP > 180 mm Hg, DBP > 90 mm Hg Anxiety Diaphoresis No Extubation Extubation Criteria Ability to protect upper airway – Effective cough – Alertness Improving clinical condition Adequate lumen of trachea and larynx – “Leak test” to identify patients who are at risk for post-extubation stridor Extubation Criteria Post Extubation Stridor • The Cuff leak test during MV: – – – – Set a tidal Volume 10-12 ml/kg Measure the expired tidal volume Deflated the cuff Remeasure expired tidal volume (average of 46 breaths) – The difference in the tidal volumes with the cuff inflated and deflated is the leak • A value of 130ml 85% sensitivity 95% specificity Extubation Criteria Post Extubation Stridor • Cough / Leak test in spontaneous breathing – Tracheal cuff is deflated and monitored for the first 30 seconds for cough. – Only cough associated with respiratory gurgling (heard without a stethoscope and related to secretions) is taken into account. – The tube is then obstructed with a finger while the patient continues to breath. – The ability to breathe around the tube is assessed by the auscultation of a respiratory flow. Extubation Criteria • The risk of postextubation upper airway obstruction increases with – – – – 21 the duration of mechanical ventilation female gender trauma, and Repeated or traumatic intubation Failure of SBT • Correct reversible causes for failure – – – – – – adequacy of pain control the appropriateness of sedation fluid status bronchodilator needs the control of myocardial ischemia, and the presence of other disease processes • Subsequent SBTs should be performed every 24 h 22 Failure of SBT Respiratory Increased resistance Decreased compliance Increased WOB and exhaustion Auto-PEEP Cardiovascular Backward failure: LV dysfunction Forward heart failure Metablic/Electrolytes Poor nutritional status Overfeeding Decreased Mg and PO4 levels Metabolic and respiratory alkalosis Infection/fever Major organ failure Stridor Failure of SBT • Left Heart Failure: – Increased metabolic demands – Increases in venous return and pulmonary edema • Appropriate management of cardiovascular status is necessary before weaning will be successful Failure of SBT Factors affecting ventilator demands Failure of SBT Therapeutic measures to enhance weaning progress Weaning Modes • Patients receiving mechanical ventilation for respiratory failure who fail an SBT should receive a stable, nonfatiguing, comfortable form of ventilatory support 27 Weaning Modes Modes of Partial Ventilator Support *SIMV synchronized intermittent mandatory ventilation; PSV pressure support ventilation; VS volume support; VAPS(PA) volume assured pressure support (pressure augmentation); MMV mandatory minute ventilation; APRV airway pressure release ventilation. 28 Weaning Modes PSV: Pressure Support • Gradual decrease in the level of PSV on regular basis (hours or days) to minimum level of 5-8 cm H2O • PSV that prevents activation of accessory muscles • Once the patient is capable of maintaining the target ventilatory pattern and gas exchange at this level, MV is discontinued Weaning Modes SIMV: synchronized intermittent mandatory ventilation • Gradual decrease in mandatory breaths • It may be applied with PSV • Has the worst weaning outcomes in clinical trials • Its use is not recommended 30 Weaning Modes New Modes • • • • • 31 VS, Volume support Automode MMV, mandatory minute ventilation ATC, automatic tube compensation ASV, adaptive support ventilation Weaning Protocols • With the assisted modes, to achieve patient comfort and minimize imposed loads, we should consider: – sensitive/responsive ventilator-triggering systems – applied PEEP in the presence of a triggering threshold load from auto-PEEP – flow patterns matched to patient demand, and – appropriate ventilator cycling to avoid air trapping are all important to 32 Weaning Protocols • Weaning protocols – Developed by multidisciplinary team – Implemented by respiratory therapists and nurses to make clinical decisions – Results in shorter weaning times and shorter length of mechanical ventilation than physician-directed weaning • Sedation protocols should be developed and implemented 33 Role of Tracheotomy • Candidates for early tracheotomy: – – – – 34 High levels of sedation Marginal respiratory mechanics Psychological benefit Mobility may assist physical therapy efforts. Role of Tracheotomy • The benefits of tracheotomy include: – – – – – – – 35 improved patient comfort more effective airway suctioning decreased airway resistance enhanced patient mobility increased opportunities for articulated speech ability to eat orally, and more secure airway Role of Tracheotomy • Concerns: – Risk associated with the procedure – Long term airway injury – Costs 36 Long-term Facilities • Unless there is evidence for clearly irreversible disease (e.g., high spinal cord injury or advanced amyotrophic lateral sclerosis), a patient requiring prolonged mechanical ventilatory (PMV) support for respiratory failure should not be considered permanently ventilatordependent until 3 months of weaning attempts have failed. 37 Long-term Facilities • Critical-care practitioners should familiarize themselves with specialized facilities in managing patients who require prolonged mechanical ventilation • Patients who failed ventilator discontinuation attempts in the ICU should be transferred to those facilities 38 Long-term Facilities • Weaning strategies in the PMV patient should be slow-paced and should include gradually lengthening SBTs • Psychological support and careful avoidance of unnecessary muscle overload is important for these types of patients 39 Thank You Introduction • 75% of mechanically ventilated patients are easy to be weaned off the ventilator with simple process • 10-15% of patients require a use of a weaning protocol over a 24-72 hours • 5-10% require a gradual weaning over longer time • 1% of patients become chronically dependent on MV Readiness To Wean • • • • • Improvement of respiratory failure Absence of major organ system failure Appropriate level of oxygenation Adequate ventilatory status Intact airway protective mechanism (needed for extubation) Oxygenation Status • PaO2 ≥ 60 mm Hg • FiO2 ≤ 0.40 • PEEP ≤ 5 cm H2O Ventilation Status • Intact ventilatory drive: ability to control their own level of ventilation • Respiratory rate < 30 • Minute ventilation of < 12 L to maintain PaCO2 in normal range • Functional respiratory muscles Intact Airway Protective Mechanism • • • • • Appropriate level of consciousness Cooperation Intact cough reflex Intact gag reflex Functional respiratory muscles with ability to support a strong and effective cough Function of Other Organ Systems • Optimized cardiovascular function – Arrhythmias – Fluid overload – Myocardial contractility • Body temperature – 1◦ degree increases CO2 production and O2 consumption by 5% • Normal electrolytes – Potassium, magnesium, phosphate and calcium • Adequate nutritional status – Under- or over-feeding • Optimized renal, Acid-base, liver and GI functions Predictors of Weaning Outcome Predictor Value Evaluation of ventilatory drive: P 0.1 < 6 cm H2O Ventilatory muscle capability: Vital capacity Maximum inspiratory pressure > 10 mL/kg < -30 cm H2O Ventilatory performance Minute ventilation Maximum voluntary ventilation Rapid shallow breathing index Respiratory rate < 10 L/min > 3 times VE < 105 < 30 /min Maximal Inspiratory Pressure • Pmax: Excellent negative predictive value if less than –20 (in one study 100% failure to wean at this value) An acceptable Pmax however has a poor positive predictive value (40% failure to wean in this study with a Pmax more than –20) Frequency/Volume Ratio • Index of rapid and shallow breathing RR/Vt • Single study results: – RR/Vt>105 95% wean attempts unsuccessful – RR/Vt<105 80% successful • One of the most predictive bedside parameters. Measurements Performed Either While Patient Was Receiving Ventilatory Support or During a Brief Period of Spontaneous Breathing That Have Been Shown to Have Statistically Significant LRs To Predict the Outcome of a Ventilator Discontinuation Effort in More Than One Study* Weaning to Exhaustion • • • • • • • RR > 35/min Spo2 < 90% HR > 140/min Sustained 20% increase in HR SBP > 180 mm Hg, DBP > 90 mm Hg Anxiety Diaphoresis Work-of-Breathing • Pressure= Volume/compliance+ flow X resistance • High airway resistance • Low compliance • Aerosolized bronchodilators, bronchial hygiene and normalized fluid balance assist in normalizing compliance, resistance and work-of-breathing Auto-PEEP • Increases the pressure gradient needed to inspire • Use of CPAP is needed to balance alveolar pressure with the ventilator circuit pressure • Start at 5 cm H2O, adjust to decrease patient stress • Inspiratory changes in esophageal pressure can be used to titrate CPAP 0 Gradient -5 -5 0 Gradient Auto PEEP +10 -5 -15 PEEP 10 Gradient Auto PEEP +10 5 -5 Preparation: Factors Affecting Ventilatory Demand Integrative Indices Predicting Success Measured Indices Must Be Combined With Clinical Observations Three Methods for Gradually Withdrawing Ventilator Support Although the majority of patients do not require gradual withdrawal of ventilation, those that do tend to do better with graded pressure supported weaning than with abrupt transitions from Assist/Control to CPAP or with SIMV used with only minimal pressure support. Thank You