The Chronic Myeloproliferative Disorders
• Polycythemia vera (PV)
• Essential thrombocytosis (ET)
• Primary myelofibrosis (PMF)
– All 3 are clonal stem cell disorders in which there is:
• “Overproduction” of 1 or more of the formed elements of the
blood
• Splenomegaly due to extramedullary hematopoiesis
• Myelofibrosis
• Transformation to acute leukemia at variable but low rates
• The 3 disorders were recently reclassified by the
WHO as myeloproliferative neoplasms
The Revised WHO Classification of the
Chronic MPDs
MYELOPROLIFERATIVE NEOPLASMS
• Chronic myeloid leukemia, BCR-ABL1-positive
• Chronic neutrophilic leukemia
• Polycythemia vera
• Essential thrombocytosis
• Primary myelofibrosis
• Chronic eosinophilic leukemia, not otherwise specified
• Mastocytosis
• Myeloproliferative neoplasms, unclassifiable
Vardiman JW, et al. Blood. 2009;114:937..
Rationale for Classifying PV, ET, and PMF
Separately From the Myeloproliferative
Neoplasms
• These 3 disorders share in common mutations in
the JAK2 and MPL genes
• There is an inherent (germline) patient proclivity
to JAK2 and MPL mutations
• Constitutive signal transduction in these disorders
occurs through normal signaling pathways
• Phenotypic mimicry and clinical overlap occur
between these 3 disorders but not between them
and the other MPNs
• Targeted therapy has been developed for PV, ET,
and PMF
The Phenotypic Mimicry of the Chronic
Myeloproliferative Disorders
Essential
Thrombocytosis
“Isolated
Thrombocytosis”
Primary
Myelofibrosis
Polycythemia
Vera
“All pathways lead to polycythemia vera”
Acute
Leukemia
Cytokine Receptors Utilizing Janus Family Kinases
Reprinted from Vainchenker W, Dusa A, Constantinescu SN. JAKs in pathology:
role of Janus kinases in hematopoietic malignancies and immunodeficiencies.
Semin Cell Dev Biol. 2008;19(4): 385-393, with permission from Elsevier.
Hematopoietic Stem Cell Hierarchy
Pluripotent
Hematopoietic
Stem Cell
Common
Hematopoietic
Stem Cell
T Lymphocytes
B Lymphocytes
Erythroid Progenitors
Granulocyte-Monocyte
Progenitors
JAK2V617F
Polycythemia vera is the ultimate consequence
of the JAK2V617F mutation
Megakaryocytic
Progenitors
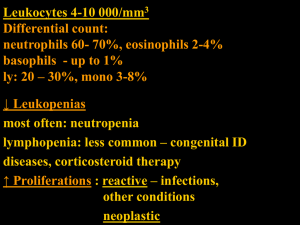
JAK2V617F Expression in the Chronic
Myeloproliferative Disorders
JAK2V617F+
JAK2V617F–
PV
PMF
ET
92%
8%*
42%
58%
45%
55%
*Some of these patients have JAK2 exon 12 mutations
Effect of JAK2V617F Expression on Clinical
Phenotype
PV
ET
PMF
-
Older
Higher (+/+)
Higher
Leukocyte count
-
Thrombosis
-
Higher
More
(venous)
PV
-
Older
Fewer
transfusions
Higher
Age
Hemoglobin
Pruritus
Transformation
Survival
More (+/+)
Fibrosis (+/+)
-
+
Longer(?)
JAK2V617F Is Not the Initiating Mutation in
the 3 MPDs
Hematopoietic stem cells do not require JAK2 for their survival or
proliferation
JAK2V617F is not present in some patients with familial
polycythemia vera
JAK2V617F can arise as a secondary event in clones expressing a
cytogenetic abnormality or another mutation
Leukemic transformation in patients with JAK2V617F-positive MPD
can occur in a JAK2V617F-negative type cell
BUT: JAK2 is the major final common signaling pathway in all
chronic MPDs and, therefore, whether mutated or not, is an
appropriate therapeutic target
Polycythemia Vera
• Polycythemia vera is a chronic
myeloproliferative disorder in which there
is overproduction of morphologically
normal red blood cells, white blood cells,
and platelets in the absence of a definable
stimulus
• Erythrocytosis is the feature that
distinguishes polycythemia vera from the
other 2 chronic myeloproliferative
disorders
• There is currently no specific clonal
diagnostic marker for polycythemia vera
Causes of Absolute Erythrocytosis Causes of Relative Erythrocytosis
Hypoxia
Carbon monoxide intoxication (tobacco
abuse, environmental)
High-affinity hemoglobins
High altitude
Pulmonary disease
Right-to-left shunts
Sleep apnea syndrome
Neurologic disease
Renal
Disease
Renal artery stenosis
Focal sclerosing or membranous
glomerulonephritis
Renal transplantation
Tumors
Hypernephroma
Hepatoma
Cerebellar hemangioblastoma
Uterine fibromyoma
Adrenal tumors
Meningioma
Pheochromocytoma
Drugs
Androgenic steroids
Recombinant erythropoietin
Familial (with normal hemoglobin function; Chuvash; EPO
receptor mutations; 2,3 BPG deficiency)
Polycythemia vera
JAK2V617F
JAK2 exon 12 mutations
Loss of Fluid
From the
Vascular Space
Emesis
Diarrhea
Diuretics
Sweating
Polyuria
Hypodipsia
Hypoalbuminemia
Capillary leak syndromes,
burns
Peritonitis
Chronic Plasma
Volume
Contraction
Hypoxia from any cause
Androgen therapy
Recombinant erythropoietin therapy
Hypertension
Tobacco use
Pheochromocytoma
Ethanol abuse
Sleep apnea
Only ~5 % of patients with
absolute erythrocytosis are
likely to have polycythemia vera
Proposed Revised WHO Criteria for
Polycythemia Vera
Major
criteria
Minor
criteria
1. Hemoglobin > 18.5 g/dL in men, 16.5 g/dL in women or other
evidence of increased red blood cell volume*
2. Presence of JAK2617V > F or other functionally similar mutation
such as JAK2 exon 12 mutation
1. Bone marrow biopsy showing hypercellularity for age with
trilineage growth (panmyelosis) with prominent erythroid,
granulocytic, and megakaryocytic proliferation
2. Serum erythropoietin level below the reference range for normal
3. Endogenous erythroid colony formation in vitro
Diagnosis requires the presence of both major criteria and 1 minor criterion or the presence of the first
major criterion together with 2 minor criteria.
*Hemoglobin or hematocrit greater than 99th percentile of method-specific reference range for age, sex,
altitude of residence or hemoglobin greater than 17 g/dL in men, 15 g/dL in women if associated with a
documented and sustained increase of at least 2 g/dL from an individual’s baseline value that cannot be
attributed to correction of iron deficiency, or elevated red blood cell mass greater than 25% above mean
normal predicted value.
Tefferi A, et al. Blood. 2007;110;1092.
Algorithm for the Diagnosis of Polycythemia Vera
Elevated hemoglobin or hematocrit
Elevated red cell mass
Red cell mass and plasma
volume measurements
Both
normal
O2 saturation
> 93%
< 93%
Hypoxic erythrocytosis
JAK2V617F
+
Normal red cell mass
Decreased plasma volume
–
Polycythemia
vera
Serum
erythropoietin level
Normal or low
Polycythemia vera
EPO-receptor mutation
Renal disease
Tumors
High-affinity hemoglobins
Spivak JL, Silver RT. Blood. 2008;12:231..
Tobacco use
Androgens
Diuretics
Pheochromocytoma
Elevated
Renal disease
Tumors
VHL mutation
High-affinity hemoglobins
Essential Thrombocytosis
• Also known as essential thrombocythemia,
hemorrhagic thrombocytosis, idiopathic
thrombocytosis, or primary thrombocytosis
• Disorder of unknown etiology
• Principal clinical feature is the overproduction of
platelets in the absence of a definable cause
• No specific diagnostic marker
Causes of Thrombocytosis
• Tissue inflammation
– Collagen vascular disease, inflammatory bowel disease
• Malignancy
• Infection
• Myeloproliferative disorders
– Polycythemia vera, primary myelofibrosis, essential thrombocytosis,
chronic myelogenous leukemia
• Myelodysplastic disorders
– 5q-syndrome, idiopathic refractory sideroblastic anemia
• Postsplenectomy or hyposplenism
• Hemorrhage
• Iron deficiency anemia
• Surgery
• Rebound
– Correction of vitamin B12 or folate deficiency, post-ethanol abuse
• Hemolysis
• Familial
– Thrombopoietin overproduction, constitutive Mpl activation, K39N
Diagnostic Criteria for Essential Thrombocytosis
Persistent thrombocytosis more than 400 x 109/L in the absence of a reactive
cause*
Absence of iron deficiency (normal serum ferritin for sex)
JAK2V617F assay (peripheral blood; expression establishes the presence of an
MPD but not its type; absence does not exclude an MPD)
Hemoglobin less than 16 g/dL in a man or less than 14 g/dL in a woman
(hematocrit < 47% in a man or < 44% in a woman) in the absence of
splenomegaly; otherwise, red blood cell mass and plasma volume
determinations are mandatory if a JAK2V617F assay is positive
Negative Bcr-Abl FISH (peripheral blood) if a JAK2V617F assay is negative
If there is anemia, macrocytosis, or leukopenia, or evidence of extramedullary
hematopoiesis (ie, circulating nucleated erythrocytes, immature myelocytes, or
splenomegaly), a bone marrow examination (including flow cytometry and
cytogenetics) is mandatory regardless of JAK2V617F expression status
*Patients with MPD represent only a minority of patients with thrombocytosis in
general but constitute most of those with persistent thrombocytosis in the absence of a
definable cause.
Spivak JL, Silver RT. Blood. 2008;112:231..
Primary Myelofibrosis
• Also known as agnogenic myeloid metaplasia,
idiopathic myelofibrosis, myelofibrosis and myeloid
metaplasia, or primary osteomyelofibrosis
• Clonal stem cell disorder involving a pluripotent
hematopoietic stem cell resulting in disordered blood
cell production, marrow fibrosis, and extramedullary
hematopoiesis, most prominently involving the
spleen, with eventual bone marrow failure or
transformation to acute leukemia in some patients
Causes of Myelofibrosis
Malignant
Non-Malignant
Acute leukemia (lymphocytic,
myelogenous, megakaryocytic)
HIV infection
Chronic myelogenous leukemia
Renal osteodystrophy
Systemic lupus erythematosus
Tuberculosis
Vitamin D deficiency
Thorium dioxide exposure
Gray platelet syndrome
Thrombopoietin receptor
agonists
Hairy cell leukemia
Hodgkin disease
Primary myelofibrosis
Lymphoma
Multiple myeloma
Myelodysplasia
Metastatic carcinoma
Polycythemia vera
Systemic mastocytosis
Hyperparathyroidism
Diagnostic Criteria for Primary Myelofibrosis
Leukoerythroblastic blood picture
Increased marrow reticulin in the absence of an infiltrative or
granulomatous process
Splenomegaly
JAK2V617F assay (peripheral blood; expression establishes the
presence of an MPD but not its type; PV is always a consideration;
absence does not exclude an MPD)
Increased circulating CD34+ cells (> 15 x 106/L) and no increase in
marrow CD34+ cells by in situ immunohistochemistry
Characteristic cytogenetic abnormalities (peripheral blood:
del(13q), 9p, del(20q), del(12p), partial trisomy 1q, trisomy 8, and
trisomy 9)
Absence of Bcr-Abl, AML, or MDS cytogenetic abnormalities by
FISH (peripheral blood)
Spivak JL, Silver RT. Blood. 2008;112:231..
Survival in Polycythemia Vera
Survival curves of 396 patients with polycythemia vera compared
with life expectancy of the general population
Reprinted from Passamonti F, Rumi E, Pungolino E, et al. Life expectancy and prognostic
factors for survival in patients with polycythemia vera and essential thrombocythemia.
Am J Med. 2004;117(10):755-761, with permission from Elsevier.
The Consequences of Polycythemia Vera
Consequence
Cause
Thrombosis, systemic
hypertension, hemorrhage
Elevated red blood cell mass, decreased von
Willebrand factor multimers
Organomegaly, pulmonary
hypertension
Extramedullary hematopoiesis or elevated red
blood cell mass
Pruritus, acid-peptic disease
Erythromelalgia
Hyperuricemia, gout, renal
stones
Myelofibrosis
Acute leukemia
Inflammatory mediators
Thrombocytosis
Increased cell turnover
Reaction to the neoplastic clone
Therapy-induced or clonal evolution (“Richter
syndrome”)
The Challenges of Treating Polycythemia
Vera
• In a study of 1213 patients with PV, cancer-free survival and
survival analyses for death or major thrombosis were better
among patients who did not receive chemotherapy[a]
• In a prospective, controlled clinical trial of 292 patients with
PV, hydroxyurea did not prevent thrombosis or myelofibrosis[b]
• Hydroxyurea therapy was associated with a late (> 10 years)
risk for transformation to acute leukemia[b,c]
• In a study of 40 patients with PV, pegylated interferon alfa-1a
induced complete hematologic and molecular responses with
low toxicity[d]
a. GISP. Ann Intern Med. 1995;123:656.
b. Najean Y, et al. Blood. 1997;90:3370.
c. Thoennissen NH, et al. Blood. 2010;115:2882.
d. Kiladjian JJ, et al. Blood. 2008;112:3065.
The Complications of Polycythemia Vera
and Their Management
Complications
Erythrocytosis
Pruritus
Management
Phlebotomy; (new JAK2 inhibitors)
Antihistamines; (new JAK2 inhibitors); pegylated interferon;
psoralens and ultraviolet-A light ; hydroxyurea
Erythromelalgia;
ocular migraine
Aspirin; anagrelide; (new JAK2 inhibitors); pegylated interferon;
hydroxyurea
Thrombosis (arterial;
venous)
Phlebotomy; aspirin; coumadin; hydroxyurea (transient ischemic
attack only)
Thrombocytosis
(new JAK2 inhibitors); anagrelide; pegylated interferon;
hydroxyurea
Hemorrhage
Epsilon aminocaproic acid
Leukocytosis
(new JAK2 inhibitors); pegylated interferon; hydroxyurea
Hyperuricemia
Allopurinol (uric acid ~10 mg %)
Splenomegaly
(new JAK2 inhibitors); pegylated interferon; thalidomide;
hydroxyurea; imatinib; splenectomy
Effect of a JAK2 Inhibitor in 34 Patients
With Established PV (Phase 2 trial data)
• 97% achieved durable hematocrit control in the absence of
phlebotomy
• 59% achieved a durable reduction in splenomegaly of at least
50%
• 88% achieved a reduction in leukocytosis to ≤ 15 x 109/L
• 92% achieved a reduction in platelet count to ≤ 600 x 109/L
• 59% achieved a complete phenotypic remission
• 92% had durable relief from pruritus in 1 month
• The reduction in JAK2V617F allele burden was modest
• There were 3 grade 3 adverse events: 2 thrombocytopenia
and 1 neutropenia
• The nonresponder rate was 3%
Verstovsek S, et al. ASH 2010. Abstract 313.
Complications of Essential Thrombocytosis
Microvascular
ischemia
• migraine
• erythromelalgia
• transient ischemic attacks
Macrovascular
• stroke
thrombosis
• acute coronary syndrome
• peripheral arterial occlusion
• digital gangrene
• deep venous thrombosis
Hemorrhage due to acquired von Willebrand disease
Transformation to acute leukemia
Survival in Essential Thrombocytosis
Survival curves of 435 patients with essential thrombocythemia
compared with life expectancy of the general population
Reprinted from Passamonti F, Rumi E, Pungolino E, et al. Life expectancy and prognostic
factors for survival in patients with polycythemia vera and essential thrombocythemia.
Am J Med. 2004;117(10):755-761, with permission from Elsevier.
Treatment Is Not Always Required for
Patients With ET
• Thrombosis and hemorrhage are infrequent in
patients with low-risk ET and the thrombosis rate was
not different than normal[a,b]
• Thrombosis in patients with ET reaches a plateau after
9 years[a]
• Cytoreduction did not change the complication rate of
extreme thrombocytosis[c]
• The transformation of ET to high risk does not have an
impact on overall survival[a]
a. Alvarez-Laran A. et al. Blood. 2010;116:1205.
b. Ruggeri M, et al. Br J Haematol. 1998;103:772.
c. Tefferi A, et al. Blood. 2006;108:2493.
Management of Thrombocytosis in
Essential Thrombocytosis
• Asymptomatic thrombocytosis requires no therapy in the absence of a
thrombotic (prior thrombosis, tobacco use) or significant hemorrhagic
diathesis
• Platelet counts ≥ 1000 x 109/L can be associated with reduced von
Willebrand factor, high molecular-weight multimers, and ristocetin
cofactor activity
• Hemorrhage associated with thrombocytosis can be controlled with
epsilon aminocaproic acid
• Aspirin is the treatment of choice for erythromelalgia unless ristocetin
cofactor activity is reduced
• For platelet count reduction, particularly in patients under age 60,
anagrelide or interferon, if tolerated, are preferable to hydroxyurea. The
new JAK2 inhibitors may prove preferable to the above drugs
• It is not necessary to lower the platelet count to normal but only to a
level that alleviates symptoms
Effects of a JAK2 Inhibitor in 39 Patients With
Established Thrombocytosis (Phase 2 trial data)
• 49% normalized their platelet count within 2 weeks
• 82% maintained a platelet count ≤ 600 x 109/L for 9.8 months
• 93% with a platelet count ≥ 1000 x 109/L achieved a > 50%
reduction
• 75% had complete resolution of splenomegaly
• 49% had a complete phenotypic remission
• Reduction in the JAK2V617F allele burden was modest
• There were 2 grade 3 adverse events involving leukopenia
• The nonresponder rate was 8%
Verstovsek S, et al. ASH 2010. Abstract 313.
Complications of Primary Myelofibrosis
Anemia
• Hypoproliferative due to folate or iron deficiency,
inflammation, autoimmune hemolysis, hemodilution,
or impaired stem cell function
Thrombocytopenia
• Splenic sequestration, impaired stem cell function
Incapacitating splenomegaly and splenic infarction
Portal hypertension
Pulmonary hypertension
Organ compromise
• Obstructive uropathy
due to
• Intestinal obstruction
extramedullary
• Ascites
hematopoiesis
• Pleural effusions
• Hepatic failure
• Fibrous tumors
• Spinal or cranial compression
• Bone pain due to periostitis or increased
intramedullary vascularity
Bone marrow failure with pancytopenia
Acute leukemia
Survival in Primary Myelofibrosis
Risk Factors
Anemia: Hgb < 10 g/dL
Constitutional Symptoms
Peripheral Blasts > 1%
Low-Risk Score: 0-1 Factors
High-Risk Score: 2-3 Factors
Cervantes F, et al. Br J Haematol. 1998;102:684.
Management of Primary Myelofibrosis
• Low-risk patients under age 45 should be considered for marrow
transplantation if a matched sibling donor is available
• High-risk patients up to age 65 may benefit from reduced-intensity
conditioning marrow transplantation[a]
• Symptomatic anemia may respond to corticosteroids, recombinant
erythropoietin, folate, danazol, or low-dose thalidomide, or possibly
targeted JAK2 inhibition[b]
• Constitutional symptoms respond to targeted JAK2 inhibition[c]
• Splenomegaly may respond to targeted JAK2 inhibition, low-dose
interferon, low-dose thalidomide and prednisone, or hydroxyurea[c]
• Splenic irradiation is only palliative and temporary and is associated with
severe neutropenia and infection
• Splenectomy is only palliative and can lead to exuberant hepatic
extramedullary hematopoiesis or splanchnic vein thrombosis
a. Rondelli D, et al. Blood. 2005;105:4115.
b. Mesa RA, et al. Blood. 2003;101:2534.
c. Verstovsek S, et al. N Engl J Med. 2010;363:1117.
Effects of Nonselective JAK2 Inhibitors
Spleen Size
in PMF
Constitutional
Symptoms in PMF
PMF = primary myelofibrosis
Verstovsek S, Kantarjian H, Mesa RA, et al. Safety and efficacy of INCB018424, a JAK1 and
JAK2 inhibitor, in myelofibrosis. N Engl J Med. 2010;363(12):1117-1127. Copyright ©
2010 Massachusetts Medical Society. All rights reserved.
Summary
• The chronic MPDs — PV, ET, and PMF — are distinct disease entities that
share many clinical features (phenotypic mimicry) due to unregulated JAK2
signaling or a similar signaling abnormality
• Because these disorders differ with respect to their natural history and
survival, diagnosis must be accurate to ensure that therapy is appropriate
• Treatment of these 3 disorders should be tailored to fit their clinical
manifestations
• PV is the most common of the 3 MPDs because it is the ultimate expression
of the JAK2V617F mutation
• All chemotherapeutic agents are leukemogenic in the MPDs and should be
avoided whenever possible, which may now be possible with the new JAK2
inhibitors
• JAK2 inhibitors will be very useful for safely reducing splenomegaly,
controlling blood counts, and alleviating constitutional symptoms, but will
not eradicate these disorders
• Pegylated interferon or reduced-intensity conditioning bone marrow
transplantation offer the possibility of complete molecular remission