XV CONVEGNO NAZIONALE GRUPPO DI
STUDIO DIALISI PERITONEALE
BARI 18-20 MARZO 2010
LA BIOIMPEDENZA E’ UN UTILE STRUMENTO CLINICO ?
Paolo Lentini
Struttura Complessa di Nefrologia e Dialisi
Ospedale San Bassiano
Bassano Del Grappa
From PD gudelines (ISPD)
•
•
•
•
•
Biocompatible PD solutions - normal pH, low concentration of glucose
Insertion of PD catheter – 10 days-6 weeks before RRT
urea / creatinine clearance measured every 6 months
PET: 6 weeks after commencing treatment + annually
Avoid routine use of high glucose concentrations )use of icodextrin,
aminoacids instead)
• Preserve residual diuresis, obtain UF above
750 ml/day [hydration status]
• Peritonitis and exit-site infection rates, regular revision of technique
• Invasive procedures cover by ATB prophylaxis
• Topical ATB administration if needed (S.aureus, Ps. aeruginosa)
• Beware central obesity and malnutrition
ISPD GUIDELINES/RECOMMENDATIONS Perit Dial Int 2006; 26:520–522
I. CLINICAL PRACTICE GUIDELINES FOR PERITONEAL
DIALYSIS ADEQUACY
GUIDELINE 3: PRESERVATION OF RESIDUAL KIDNEY FUNCTION
Prospective randomized trials of dialysis adequacy and many observational
studies have confirmed a strong association between the presence of RKF and
reduction of mortality in patients on PD therapy.
It is important to monitor and preserve RKF. (A)
GUIDELINE 4. MAINTENANCE OF EUVOLEMIA
Volume overload is associated with CHF, left ventricular hypertrophy (LVH),
and hypertension; therefore, it is important to monitor ultrafiltration volume,
dry weight, sodium intake, and other clinical assessments of volume status.
CLINICAL PRACTICE GUIDELINES FOR PERITONEAL DIALYSIS NUTRITION
Guideline B.
• Assessment of nutritional status For PD patients should be
routinely assessed using a panel of measures.
• The frequency of using these measures has not been
verified, but a 6 monthly review is desirable.
• Serum albumin, prealbumin, creatinine and creatinine
index, dietary interviews and diaries, protein equivalent of
nitrogen appearance (nPNA), subjective global
Assessment (SGA), anthropometry and dual-energy X- ray
photon absorptiometry (DEXA) are all measures utilized to
assess nutritional status and their evidence for use will be
substantiated.
EBPG Nutrition Nephrol Dial Transplant (2005) 20 [Suppl 9]
Methods for Body Composition
Assessment
• Diluition Techniques – Reference method
–
2H, 3H, 18O,
NaBr;
• Dual Energy X-ray Absorptiometry (DEXA)- Reference method
• Computed Tomography and Magnetic Resonance Imaging
– Site Specific images - IAAT
•
Densitometry –
– Hydrostatic Weighing, BodPod
• Electrical Impedance Techniques
– BIA (single & multi- frequency)
– BIS – Cole-Cole Model
• Skinfolds & Anthropometric
• Body Mass or Weight
References Methods
• Dilution Techniques
• Deuterium (2H) exchanges with H2O –
reference method for Total Body Water
• NaBr (sodium-bromide) dilution doesn’t
cross cell membrane – ECF space
• Requires pre- and post- dilution specimen
(serum, urine) and mass spectrometer
• Dual Energy X-ray Absortiometry
(DXA)
•
•
•
•
•
X-ray
Measures Bone Mineral Content (BMC)
Bone Free Soft Tissue (BFST)
BMC + BFST = FFM
Distribution of Fat and Lean Tissue
PRINCIPLES OF BIA
The resistance (R) of an of homogeneous material of uniform
cross-sectional area is proportional to its length (L) and inversely
proportional to its cross sectional area (A).
The body offers two types of R to an electrical
current: capacitative R (Reactance), and resistive R (simply called
Resistance).
Reactance (Re or X): Capacitative R CELL MEMBRANES
Reactance (R): Extra and Intracellular FLUIDS
Impedance (Z): Relation between X and R
Phase Angle (PA): Lower phase angles: decreased cell integrity
A basic assumption of BIA is that the sum of the arm,
trunk and leg volumes can be modeled as a cylinder with uniform
conductivity.
CLASSIFICATION
• BIA: Bioelectrical Impedance Analysis
• SF-BIA: Single Frequency Bioelectrical Impedance
Analysis
• MF-BIA: Multi Frequency Bioelectrical Impedance
Analysis
• BIS: Bioelectrical Impedance Spectroscopy
• BIVA: Bioelectrical Impedance Vector Analysis
• W-BIA: Whole Body Bioelectrical Impedance Analysis
• S-BIA: Segmental Bioelectrical Impedance analysis
CLINICAL USE OF BIA IN PD
• BODY COMPOSITION ASSESSMENT
• MANAGEMENT OF EXTRACELLULAR
FLUID (DRY WEIGHT)
• ASSESSMENT OF NUTRITIONAL
STATUS
Nearly 2000 papers about BIA are found in English medical literature
1990-2010, 1200 being pubblished in the last 7 years.
MACHINES FOR BIOIMPEDANCE ANALYSIS
• Quantum II (RLJ System)
• SC-331 S (Tanita Corporation)
• ElectroFluidGraph (Akern s.r.l.)
• SFB7 (Impedimed Ltd.)
• Bioscan 916S (Maltron Ltd.
• Body Composition Monitor (Fresenius Medical Care)
CLINICAL USE OF BIA
• BODY COMPOSITION ASSESSMENT
FAT MASS
Mineral
Protein
FAT-FREE
MASS
Water
BODY COMPARTMENTS
• TBW: Total Body
Water
• ECW: Extracellular
Water
• ICW: Intracellular
Water
• BF: Body Fat
• FFM: Fat-free Mass
• FM: Fat Mass
CLINICAL USE OF BIA
• MANAGEMENT OF EXTRACELLULAR
FLUID (DRY WEIGHT)
Dry weight
“The lowest [post-dialysis] weight a patient can tolerate without
intradialytic symptoms and/or hypotension and in the absence of overt
fluid overload”
Henderson KI 17: 571-576; 1980
“ The post-dialysis weight at which the patient is and remains
normotensive until the next dialysis in spite of interdialytic
fluid retention and without antihypertensive medication”
Charra 1996
CONCEPT OF DRY WEIGHT
EXCESS FLUID WEIGHT
DRY WEIGHT
•Clinical assessment of dry weight
is a difficult task in PD patients by
the lack of treatment associated
signs indicative of dehydration as
may be observed in HD patients
such as intradialytic hypotension or
cramps.
•Useful monitoring tools for fluid
status estimation during HD like as
on line blood volume and blood
pressure measurement are not
availble for application in PD
patients
Physical examination should always be the basis for
assessment dry weight in dialysis patients.
However, as sometimes physical examination allows
no definite conclusion , several non-invasive methods
have been developed.
VOLUME
– Body Weight
– Blood Pressure
– Edema
– Diuresis
– Skin and Mucous hydration
– Hematocrit
– Electrolites Disorders
– Chest X-Ray
VOLUME EVALUATION
NO INVASIVE
INVASIVE
• U.S. Inferior vena
caval diameter
• Central Venous
Pressure
(CVP)
• Bio Impedance
Analysis (BIA)
• Pulmunary Artery
Occlusion
Pressure
(PAOP)
• Natriuretic Peptides
(ANP, BNP,CNP)
• Cardiac Output
( SVV, SVO2)
INFERIOR VENA CAVAL DIAMETER
Overhydration: VCD > 11, CI < 40%
Ideally measured 2hrs post dialysis
Limitations: Operator variability, heart failure
Timing of measurements is of pivotal importance for VCD, reference
value of 8mm/m2 obtained 2 h after dialysis.
Natriuretic peptides and the dialysis patient
BNP correlates well with cardiac function, and is a good
prognosticator for risk stratification
ANP is sensitive to volume changes during dialysis, but
changes in concentration do not predict achievement of
euvolemia.
Suresh et al. Seminars in Dialysis 2005
SF-BIA
SF-BIA, injecting 800 µA and 50 kHz alternating sinusoidal
current is passed between surface electrodes placed on hand
and foot.
At 50 kHz, the current passes through both intra and
extracellular fluid;
LIMITS
• SF-BIA permits to estimate TBW from equations derived
from healthy subjects;
• Fat-free mass is estimated by assuming TBW content is
73%, and fat is derived as weight minus FFM. Thus, both
of these are potentially unreliable in situations with
abnormal FFM hydration.
• Accuracy is not enough for clinical use due to the
individual variation in Body composition
MF-BIA and BIS
• Frequencies vary from 5 kHz – 1MHz
• In biological tissues lower frequency currents travel
preferentially in the extracellular space,whereas high
frequency currents traverse both ECV and ICV.
• Use of prediction equations - not independent of TBW
• Cole-Cole model is applying to calculate extracellular and
intracellular resistance
MF-BIA AND BIS
high
frequency
the
AtAtlow
frequency
(below
current
travels
through
30 kHz)
the current
both the
ECF and
travels
through
the ICF
ECF
Bioimpedance Spectroscopy (BIS)
Ri (Impedance Intracellular)
Determined mathematically by
parallel subtraction of Rinf and R0
BIS
Rinf
Scans from low (4 kHz) to high
(1000 kHz) frequencies 400-500
discrete data points
Impedance at infinite
KHz (Impedance TBW)
R0
Impedance at 0 kHz
(Impedance ECF)
Transformation
Key Points
ICF
(Litres)
Ri (ohm)
Transformation
Height
of the patient must be
14.2intracellular
L
Impedance
(Hanni mixture theory)
known to calculate volumes
TBW (Litres)
from the raw data (R0 and Ri).
If calculating Fat Mass in
36.4 L
addition to fluid volumes the
(14.2 + 22.2)
body weight of the patient
ECF
R0 (ohm)
(Litres)
must be known.
Impedance
22.2
extracellular
L
Transformation
(Hanni mixture theory)
Assumptions of the Hanni Mixture theory
Assumption 1
Body is made up of 5 cylinders
(2 arms, 2 legs and the
chest/abdomen)
Assumption 2
These are filled with fluid and
suspended cells of a
homogenous type and density
Assumption 3
The cylinders have a
homogenous conductive
properties (resistivities)
•
1.
2.
3.
4.
To assess abnormalities in body composition in
40 PD patients and in fluid status between
MF-BIA
Segmental BIA
Watson formula
Diluition methods (deuterium oxide [D02] for
TBW and Bromide Diluition [NaBr]for ECW
and DEXA for for body composition)
RESULTS
MF-BIA tended to underestimate TBW according to D2O
Whereas the Watson formula tended to overstimate TBW
according to D2O
• TBW: (D20 vs MF-BIA) 2.0 ± 3.9 L
• ECW: (NaBr vs MF-BIA) -2.8 ± 3.9 L
BIA techniques did not appear to have significant
advantages over the Watson formula to predicting TBW
MF-BIA AND BIS
Limits
• MF-BIA was unable to detect changes in the distribution of
fluid between extracellular and intracellular spaces in
OVERHYDRATED patients;
• BIS: Modeling for body cell mass derived from spherical
model (Cole-Cole Plot); muscle mass are non-spherical, but
rather cylindrical. This difference in geometry may account
for the understimation of R;
• Standard error by BIS for ECV measurement in healthy
subjects is> ±1 L and that of ICV is > ±1.5 L limiting their
clinical utility to dry weight determination;
BIVA
The BIVA approach developed by Piccoli
permits patient evaluation from the direct
measurement of the impedance vector and
does not depend on equations or models.
In BIVA, R and reactance (Xc),
standardized for height, are plotted as point
vectors in the R-Xc plane.
An individual vector can then be compared
with the reference 50%, 75%, and 95%
tolerance ellipses calculated in the healthy
population of the same gender and race (R
Xc graph method)
Cross-Sectional Study: 200 CAPD adults patients (149
without edema and 51 with edema). SF-BIA Rxc Graph
(BIVA) was performed and measured TBW compared
with:
1. 726 Healthy subjects
2. 1116 Hemodialysis patients
3. 50 Nephrotic patients
The mean impedance vector of CAPD patients without edema
was half way between the mean vectors of the healthy population
and the HD population before the hemodialysis session.
BIVA: Limits
An individual vector can be compared
with the reference 50%, 75%, and 95%
tolerance ellipses calculated in the healthy
population of the same gender and race
SEG-BIA
Segmental-BIA is performed by either placing two additional electrode on
wrist and foot on the opposite side, or by placing sensor electrodes on
wrist, shoulder (acromion), upper iliac spine and ankle.
The trunk of the body contributes only as 10% to whole bodyimpedance;
This implies three aspects :
(1)Changes of the impedance are closely related to changes of the FFM
(or muscle mass or body cell mass (BCM)) of the limbs;
(2) Changes of the FFM of the trunk are probably not adequately described
by whole body impedance measurements;
(3) Segmental BIA must be used to determine fluid shifts and fluid
distribution in some diseases (ascites, renal failure, surgery), and may
be helpful in providing information on fluid accumulation in the
pulmonary or abdominal region of the trunk (PD?)
Composition of the ESPEN Working Group; Clinical Nutrition (2004) 23, 1226–1243
AIM:Using Segmental BIA to determine the
characteristics of fluid shift of each body
segment in 13 CAPD patients before and after
PD solution exchange
Method: Seg-BIA Trunk, arms and legs 1 h
before and 1 and 2 hors later PD solution
exchange
RESULTS
ARMs
IMPEDANCE (ω)
ARMS: Increased 1 h after
drainage;
LEGS: Decrease after
exchange;
TRUNK: Increase 1 h after
drainage;
LEGs
TBW (L)
ARMS: - 0.25 L
LEGS: + 0.47 L
TRUNK: -0. 25 L
TRUNK
The change in body
weight significantly
correlated with total
net calculated water
volume change
(p = 0.009)
14 CAPD patients during standard exchange with
fluids of known conductivity.
Bioimpedance was continuously measured in the
arm, trunk, and leg and from wrist to ankle.
Volume changes were calculated using both
segmental BIA (SBIA) and wrist-to-ankle BIA
(WBIA) and were compared with volume changes
measured gravimetrically.
When 2.19 ± 0.48 L were removed from the
peritoneal cavity during draining, 95.2 ± 3.8%
of this volume was detected by SBIA compared
with 12.5 ± 24.3% detected by WBIA.
When 2.11 ± 0.20 L of fresh dialysate was
infused into the peritoneal cavity, 91.1 ± 19.6%
of this volume was detected by SFBIA
compared with only 8.86 ± 21.1% detected by
WBIA.
SEGMENTAL BIA LIMITS
• Segmental-BIA requires prior standardization,
particularly when different approaches and
different BIA devices are employed;
• Standardization of the type of electrodes used and
their placement;
• In literature we found very high relative errors
with segmental-BIA for arms and legs FFM: 13–
17% for arm FFM and 10–13% for leg FFM.
CLINICAL USE OF BIA
• ASSESSMENT OF NUTRITIONAL
STATUS
NUTRITIONAL STATUS
• MF-BIA: Body cell mass are derived from from DEXA in
healthy as well as TBW are derived from D2O diluition in
healthy:in conditions of abnormal fluid distribution can
affect resistance and the error must be significant for FFM
• SF-BIA and FFM: BIA measure primarly TBW when the
high correlations with FFM assume that the hydration
costant is stable at 73%.
In overhydrated patient the use of SF-BIA or MF-BIA or BIS
to estimate FFM for nutritional assessment may lead to
erroneous results
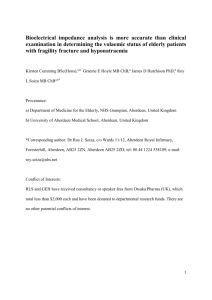
PHASE ANGLE
PhA has been correlated with the disease prognosis in HIVInfection, hemodialysis, peritoneal dialysis, chronic renal
failure and Liver cirrhosis patients: these study suggest that
PhA may be useful in determining increased risk of morbidity
and that PhA decreased with age
This study prospectively examined the relationship of
bioimpedance indexes to the nutrition status and
survival of 45 PD patients who were followed for
more than 1°year.
The cumulative observed survival of PD
patients with an enrollment phase angle
>6 degrees was significantly (p= 0.01)
Higher than that of patients with an
Enrollment phase angle <6 degrees.
The BIA indices reflect nutrition status
in PD patients, and may be useful in
Monitoring Nutrition
Fein PA, Advances in Peritoneal Dialysis, Vol. 18, 2002
OTHERS APPLICATIONS OF BIA
TO PD
• Outflow Failure
• Dialysis Adequacy (Mendley et al ): Kt/V urea in
pediatric PD patients utilizing TBW for volume
(by SF-BIA) and compared with deuterium
diluition.(mean difference 0.33± 1.44 L ns)
• Blood Pressure Control and fluid status in PD
(Wang et al): ECV higher in uncontrolled
hypertension
SEGMENTAL BIA IN PD
• Outflow failure, defined by the incomplete recovery of instilled
fluid, is observed frequently in PD patients. Kinking of the
catheter, malpositioning, omental occlusion and constipation are
commonly observed, but it is important to exclude dialysate
leakage as the underlying cause. The initial manifestations of
dialysate leakage may be subtle.
• Intra-abdominal fluid volume determined by segmental BIA could
aid differential diagnosis of outflow failure (catheter problem
versus leakage) and reduce the need for imaging studies.
BIA UNSOLVED PROBLEMS
• Limitations of BIA equations
• Limitations of Reference Methods
• Limitations with reference study population
(Ethins specificity differences)
• Limitations imposed by uremia and dialytic
process on BIA measurement
• Common errors in BIA application
LIMITATIONS OF BIA
EQUATIONS (1)
• Regression Functions (for SF-BIA): Based on
experimental data derived from healthy
population;
• Model that used equations based on the
knowledge of extra- and intracellular volume
space distribution (for MF-BIA and BIS) for
bicompartimental model;
• The trunk contributes only a small proportion to
whole body impedance;
TBW ERRORS
Composition of the ESPEN Working Group; Clinical Nutrition (2004) 23, 1226–1243
FAT-FREE MASS Errors
Composition of the ESPEN Working Group; Clinical Nutrition (2004) 23, 1226–1243
REFERENCE METHODS
Each of these reference methods has limitations and
makes assumptions that are not valid in all situations
• Isotope Diluition is not valid for multicompartment model
• DEXA limitations is that results by different
manufacturers do not agree.
• TBK is a reference method for body cell mass
(BCM) but is limited in the determination of FFM
because TBK content varies with sex and age.
STUDY POPULATON SUBJECTS
• Ethnic-specific equations for body composition
are justified because of differences in body build
among ethnic groups. Relative leg lengths, frame
size and body buildt are factors responsible for
ethnic differences in the body mass index (BMI);
• Failing to adjust for differences in FFM density in
ethnic groups may result in systematic biases 310%.
BIA MEASUREMENT
CONDITIONS (1)
• Subject must be measured for height and weight at the time
of BIA
• Body Position: Supine, arms separeted from trunk by about
30° and les separeted by about 45°
• Previous Exercise: No excercise from about 8 hours;
• Dietary Intake: Stop Food 2-4 hours before;
• Skin Temperature: Integrity, Clean with alcohol
• Electrode Position: Min. 5 cm of distance between
electrodes;
• Ethnic Group: Note Race, USE SPECIFIC EQUATION IF
AVAILABLE
• Time Measurement: For Hemodialysis: 20-30 minute after
session results show not difference against 2 hours after
session;
BIA MEASUREMENT CONDITIONS
(2)
• Severely malnourished (BMI<16 Kg/m²) or Obese (BMI>
34 Kg/m²) BIA results are affected by variable tissue
hydration and should be interpreted with caution
• Body Abnormalities: Amputation-Orthopedic prosthesis
,Atrophy, Hemiplegia,dystrophy (Duchenne, Cushing’s
syndrome etc), Pachydermia (May invalidated meausre for
high skin resistance;
• Special Conditions: Ascites with or without Liver Failure,
• Hemodialysis : No vascular access side;
• Peritoneal Dialysis: No difference between empty of full
abdomen, consider Seg-BIa
• Treatments: Electrolite infusions and diuretics can
interferes with BIA results
• Pacemaker-Defibrillator: No interference with
measurement
Limitations imposed by dialysis on
BIA measurement
• Underlying equations derived from non-uraemic
control groups.
• Fluids, Electrolyte and hematocrit: An increase in
Eletr or hematocrit concentrations will result in a
reduction in R
• Error of method vs fluid removal in HD and PD:
SEE for linear-regression for BIA equations is 2
L, the usual amount of ultrafiltrate removed ranges
from 1-4 L
• Arms and Legs contribute 90% of whole-body
impedance: abdomen fluids are under-estimated
respect to Seg-BIA
CONCLUSIONS
• Visible Edema: Hand-to foot SF-BIA is not valid
• Significantly altered hydration states (Diuretic, ascites,
liver and heart failure): the application of SF and MF-BIA
are not appropriate to assess ICW and ECW;
• HD/DP: MF-BIA and BIS do not appear accurate to
determine dialysis volume and intraperitoneal fluid
changes
• Segmental BIA may prove to be best to determining
abnormal hydration in trunk and ouflow failure: however
this method is has not yet been sufficiently standardized to
be used as a bedside technique
• BIVA method is able to detect altered tissue electric
property in ill subjects; Low PhA have been shown to be
of prognostic relevance in HD and PD patients
CONCLUSIONS
We have to use different tecniques for
different patients for different aims;
We need standardization of the current
Techniques and reference equations for
specials kidney related populations
(CKD, HD, PD).
GRAZIE