Tracking the Nottingham contribution to PD-PROBAND
advertisement
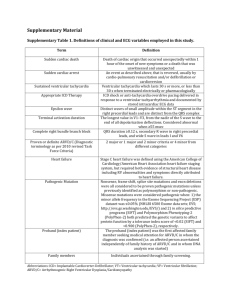
Tracking the East Midlands contribution to PD-PROBAND Nin Bajaj Clinical Director NPF International Centre of Excellence in PD, East Midlands Trent CLRN PD Research Champion PRoBAND: history Parkinson’s UK placed call for major biomarker study Joint scientific and clinical consortia formed PRoBaND was the clinical consortium to 2 of 3 studies Discovery Award went to Oxford group (£5m) Parkinson’s UK sought reactivation of PRoBaND PRoBAND: history Parkinson’s UK placed call for major biomarker study Joint scientific and clinical consortia formed PRoBaND was the clinical consortium to 2 of 3 studies Discovery Award went to Oxford group (£5m) Jan 2011 Apr 2012 Public launch Parkinson’s UK sought reactivation of PRoBaND PRoBaND: overview • Prospective clinical study of PD patients and relatives • DNA collected, tested, and stored • Serum collected and stored PRoBaND: recruitment of PD cases Around 2200 cases (PD diagnosed within last 3 years or <50 years) Study visits 6-monthly for 3 years (recent onset) Only 0 and 6 months for young onset Blood sample for DNA tests and biomarker analysis Clinical scoring: motor, non-motor, olfactory PRoBaND: sample size Patients Recent onset PD under 50 2000 Gene tests 100 + 1900 – Diagnosis 240 12 + 228 – PRoBaND: sample size Patients Recent onset PD under 50 2000 Gene tests 100 + 1900 – 150 600 750 Siblings Diagnosis 240 12 + 228 – PRoBaND: sample size Patients Recent onset PD under 50 2000 Gene tests 100 + 1900 – 150 600 750 Siblings Diagnosis 240 12 + 228 – 18 72 90 PRoBaND: recruitment of siblings Around 800 subjects (sibs of PD cases recruited to main study) Visit schedule: 0, 36 months Blood sample for DNA tests and biomarker analysis Health questionnaires and clinical examination PRoBaND: the detail • Clinician scoring • *Past, social and family history • UPDRS - clinician • Cognitive – MoCA, fluency • *Response to medication • Diagnostic evolution *Once during study • • • • • • • • • • Patient scoring UPDRS – patient *Smell – UPSIT Depression – HADS Sleep – ESS, RBD, PDSS Autonomic – SCOPA QoL – EQ5D, PDQ8 ICDs – QUIP NMS scoring Wearing-off Basic plan for Parkinson gene tests LRRK2 GBA Recent onset PD Diagnosis under 50 Parkin (PARK 2) PINK-1 (PARK 6) Basic plan for Parkinson gene tests LRRK2 GBA Recent onset PD Diagnosis under 50 Parkin (PARK 2) PINK-1 (PARK 6) Extend to new techniques eg. immunochip analysis Proteomics in Parkinson’s Disease- review of current work Nin Bajaj Nottingham Key Points • Most published studies in PD are CSF not plasma based • LP hard to justify in PD patients • Diagnosis in most PD is clinical (PDBBC) • DaTSCAN is available for clinically challenging patients although expensive, high sensitivity/specificity not possible in all centres (95%) and not known in pre-motor disease, not universally available, not possible for community screening, cannot track disease progression in trials Key Points • Current biomarkers are pg/ml but although sensitive, have poor specificity to distinguish IPD from normals • Using panel arrays is still in its infancy • A number of biomarker projects in PD have funding from MJF foundation Plasma Alpha-Syn • Plasma αsynuclein difficult as numerous sources including platelets, RBCs, skin cells, vascular cells • serum levels unlikely to be useful • widespread distribution of αsynuclein also has implications for CsF re traumatic tap • one small study found that the SNCA gene, upregulated in the skin fibroblasts of patients with PD, but not in controls or AD • Recent paper (Foulds et al FASEB 2011) found mean level of phospho-alpha-syn higher in PD than controls, although no difference in total alpha syn or oligo alph syn or oligophosphoalphasyn Plasma profiling • Plasma metabolomic profiling (liquid chromatography electrochemical array detection) identified several markers that were predictive of IPD, including low uric acid and high glutathione levels, in a sample of 25 controls and 66 patients Ttau or Ptau • CSF ttau and ptau increased in AD v DLB or controls • Use of CSF Ab42:t or ptau reliably distinguishes AD from DB with 90% accuracy • CSF Abeta42 lower in AD or DLB v PD or controls PSP v IPD • CSF p or t tau no different between PSP and PD • extended (55 kDa) and truncated (33 kDa) tau forms, proteolytic by-products of tau requiring immunoprecipitation, more time consuming and operatordependent than ELISA • Trunc tau:extended tau substantially reduced in patients with PsP compared with normal agematched controls. PSP v IPD • 85% accuracy distinguishing PsP from all other neurodegenerations • sensitivity of 96% and specificity of 85.7% were reported for comparing PsP with iPD or DlB • sensitivity of 90% and specificity 76.2% for PSP v CBD but single centre (Borroni, B. et al. Tau forms in CSF as a reliable biomarker for progressive supranuclear palsy. Neurology 71, 1796–1803 (2008).) CBD • In one study, CSF ttau significantly higher in patients with CBD v PSP-RS and controls (sensitivity of 81.5% and specificity of 80%- when ‘moderately severe’ cases analyzed separately, sensitivity of 92.3% and specificity of 100%) • Contradicted by a smaller study, in which CSF ttau and ptau similar levels in control, PSP and CBD MRI Imaging in PD • • • • Challenges Current technologies Nottingham contribution Proposed trial PaMIR: Parkinson MR Imaging Repository • MRI biomarker research in Parkinson’s is an emerging field with limited and often controversial findings • To overcome this we propose to build a large dedicated MRI imaging repository in early Parkinson’s to assess the diagnostic accuracy and predictive power of novel MRI biomarkers • Candidate MRI markers were selected from metaanalyses of published evidence and our own pilot and proof of concept studies • We plan to collect neuromelanin, iron, diffusion tensor and resting state functional MRI at 3T in 300 people with early Parkinson’s co-recruited from the Tracking Parkinson’s study PaMIR: Parkinson MR Imaging Repository • Control data will be included from 100 age matched healthy controls • 150 people with and 50 without the condition will be rescanned after 18 months to assess progression. • This will allow creation of unique virtual Parkinson’s Brain Bank, which will be the largest repository of advanced MRI linked to clinical, genetic and potentially proteomic phenotyping