Hypoglycaemia - CHSA Diabetes Service
advertisement
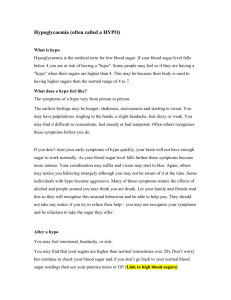
Hypoglycaemia Diabetes Outreach (June 2011) Hypoglycaemia Learning outcomes > Can state what hypoglycaemia is > Be able to assess who is at risk of hypoglycaemia > Be able to recognise a hypo event > Can state the treatment of a hypo in a health service and in the community > Is aware of the ways that hypo’s can be prevented. 2 What is hypoglycaemia? > In people with diabetes who are at risk, hypoglycaemia can cause signs and symptoms. > Hypoglycaemia is usually defined as a BGL less than 4mmol/L. > The BGL at which signs and symptoms occur can vary from person to person. 3 Features of hypoglycaemia Symptoms of hypoglycaemia occur as a response to adrenaline (pale skin, sweating, shakiness, palpitations, tingling especially around the lips, feeling of anxiety). Due to decreased glucose in the brain (hunger, confusion, behaviour changes & psychological reactions, seizures and coma). 4 Signs and symptoms Signs blood glucose level < 4.0mmol/L Symptomatic (sometimes) unconscious Symptoms: hunger / sweating faintness / dizziness trembling palpitations headache irritability / confusion unconsciousness 5 Causes of hypoglycaemia > > > > > > missing or delaying a meal or snack inadequate carbohydrate intake over-administration of insulin/OHA prolonged exercise excessive alcohol vomiting. 6 Who’s at risk? Consider > types of diabetes > age of the person > duration of diabetes > type of medication > hypo awareness > diabetes complications > weight > exercise > excessive alcohol intake. 7 Treatment of conscious person Step 1 BGL <4.0mmol/L give 15g fast acting carbohydrate (CHO) eg 90ml Lucozade, or 15g glucose tablets or equivalent. Step 2 Test BGL at 10 mins. If over 4 proceed to step 3, if under repeat step 1. 8 Treatment of conscious person Step 3 Give slow acting CHO eg 2 biscuits or 1 piece of fruit or 1 cup (250ml) of milk or equivalent or the person’s regular meal if available. Step 4 Ensure person receives and eats a normal meal (adequate CHO serves) when next due. 9 Unconscious hypoglycaemia > If the person is unable to safely swallow then glucagon needs to be administered either IM or SC. > People at significant risk of unconscious hypo need to receive education about glucagon. A caregiver or family member will require training. > In a hospital or health service, nurses can administer glucagon using a standing order. > If no response to glucagon 50% IV glucose will need to be ordered by MO. 10 Administration of: Glucagon (IM) is used when a person is unconscious. Given intramuscular (but can be given subcutaneous or intravenously). Requires approx 6-10 minutes for peak onset of action. Glucose (IV) given as 10ml of 50% glucose intravenously. 11 12 Diabetes Manual 2010 Follow up Follow-up post severe ‘hypo’: > reassess person 15-30mins post hypo > check BGL after 30mins from initial time if level is <4mmol/L repeat step 1 & 2 > may need IVT (5% Dextrose) > BGL 2-4 hourly for 12-24 hours (depending on severity and duration) > documentation of event. 13 ‘Hypo’ kit for health services A ‘hypo’ emergency kit can be assembled and placed in every ward or community health area and should contain at least the following: Quickly digested CHO: 1 bottle 50g Lucozade (90ml = 15g CHO) Slowly digested CHO: Biscuits. 14 ‘Hypo’ kit for health services 15 Hypo action plans in the community > All people at risk of hypo should have an action plan. > A hypo kit is central to this action plan. > Ask the person what foods they would like to keep in their hypo kit. > A hypo kit makes sure the person has planned for a hypo in various situations. 16 Case scenario Lucy is 70yrs old. She has had type 2 diabetes for 20yrs. She is on a reduced dose of Metformin, Daonil (sulphonylurea) and a basal insulin. Over the past 4 years her weight has dropped slightly from 63kgs to 57. She lives alone. 17 My ‘hypo’ plan BG ___________________________ Step 1 at home ___________________________ out / car ___________________________ Step 2 monitor BG – 10-15 min and repeat step 1 until BG over 4 or Step 3 ____________________________ at home ____________________________ out / car ____________________________ Step 4 monitor BG – 1-2 hour increasing gap time until happy no repeat hypo or ____________________________ NB ________________________________________ ___________ 18 Question > > > > Is Lucy at risk of hypoglycaemia? What makes her high risk? How would you address the risk factors? Use the hypo action plan on the next slide to assist with the discussion. 19 Summary > Important that nurses assess the persons knowledge and self care of hypoglycaemia. > People should have an action plan in place for hypoglycaemia. > All health services and hospitals should have a protocol in place for treatment of hypo and a hypo kit that is easily accessible in all patient care areas. 20 References > Cryer P E, Davis S N, and Shamoon H S (2003) Hypoglycemia in diabetes. Diabetes Care, 26(6): p1902-1912. > Diabetes Outreach (2009) Diabetes Manual, Section 4: Hospitalisation, Section 11: Unstable diabetes. > Diabetes Outreach (2011) Low blood glucose in type 2 diabetes (hypoglycaemia) factsheet. http://diabetesoutreach.org.au/consumer/defa ult.asp 21 22