PowerPoint - Q-CROC
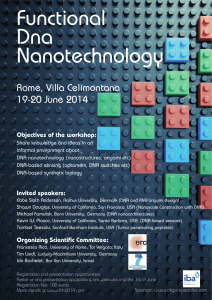
advertisement
DNA damage in cancer therapy Lawrence Panasci MD Department of Oncology & Experimental Medicine Segal Cancer Center-Lady Davis Institute Jewish General Hospital-McGill university Potential Conflict of Interest • Dr. Lawrence C. Panasci – None Advances in cancer survival 1.Two recent cytotoxic agents, taxanes and oxaliplatin 2. Herceptin, Rituximab, Gleevec and perhaps Sutent Repair of Specific DNA Lesions DNA DAMAGE Repair of DNA Strand Breaks DNA Repair in cancer and normal cells Cytotoxic anticancer drugs • DNA cross-linking agents, i.e. the platinum compounds(cis-platinum and oxaliplatin) and nitrogen mustards(chlorambucil) result in cytotoxic interstrand cross-links(ICLs) • Anthracyclines (adriamycin), etoposide and irinotecan result in potentially lethal double strand breaks (DSBs) Repair of interstrand cross-links(ICLs) and double strand breaks(DSBs) • Repair of DSBs and ICLs may occur via similar DNA repair pathways • An intermediate step in repair of ICLs may involve induction of DSBs • ICLs are produced by DNA cross-linking agents such as platinums and nitrogen mustards • DSBs are produced by ionizing radiation(IR) or agents such as etoposide and irinotecan DNA DSB -induced activation of checkpoint and repair pathways. Bolderson E et al. Clin Cancer Res 2009;15:6314 -6320 ©2009 by American Association for Cancer Research Rad-51 Directed DSB repair Non Homologous End Joining Repair Nitrogen Mustard (NM) Drug Resistance in chronic lymphocytic leukemia (CLL) (1)Lymphocytes from treated-resistant CLL patients have an enhanced capacity to remove DNA interstrand crosslinks formed by NMs such as chlorambucil as compared with those from untreated patients (2)The development of chlorambucil (CLB) resistance in CLL appears to be specifically associated with cross-resistance to other bifunctional alkylating agents, which produces interstrand cross-links (ICL) in DNA. (3)Thus, enhanced ICL-specific repair appears to be one of the primary mechanisms of NM resistance in CLL Nitrogen Mustard (NM) Drug Resistance in CLL (continued) (4)DNA ICL and certain double-strand breaks require information supplied by another chromosome or chromatid for error-free repair. (5)It is thought that ICL are removed from the DNA of mammalian cells by the combined actions of excision repair (NER) and recombination systems. (6)Our results suggest that the incision/excision step of ICL repair is not rate-limiting in CLBresistant lymphocytes but instead is associated with enhanced recombinational repair of ICL. Nitrogen Mustard (NM) Drug Resistance in CLL (continued) (7) It is possible that the repair of ICLs involves an intermediate step of DSB formation (8) Both homologous recombinational repair (HRR) and nonhomologous endjoining (NHEJ) are implicated in the repair of DSBs (9) Since CLL lymphocytes are largely nonproliferative and since NHEJ can repair DSBs in all phases of the cell cycle but HRR is more involved in S/G2 phases of the cell cycle, NHEJ is apt to be more prominent in CLL lymphocytes (10) NHEJ components include the Ku70/Ku80 heterodimer that is recruited to DSBs, followed by DNA-PKcs, XRCC4, and ligase IV to complete NHEJ. Nitrogen Mustard (NM) Drug Resistance in CLL(continued) (11)DNA-dependent protein kinase (DNA-PK) is a nuclear protein serine/threonine kinase comprised of 3 subunits; a large catalytic subunit of 460 KD, DNA-PKcs and a DNA binding subunit, the Ku autoantigen (a dimer of Ku70 and Ku86 proteins). (12)Mutations in the subunits result in doublestrand break repair defects, X-ray sensitivity, impaired V(D) J recombination and nitrogen mustard sensitivity. (13)The role of DNA-PK was investigated vis-à-vis nitrogen mustard drug resistance in CLL NHEJ in CLL NM drug resistance • KU80 protein levels and DNA-PK activity correlate directly with CLB drug resistance in-vitro in CLL lymphocytes • These results suggest that NHEJ may play a role in CLB drug resistance in CLL • In order to investigate this, we utilized relatively specific inhibitors of DNA-PK NU7026 is a specific DNA-PKi • Wortmannin, a nonspecific DNA-PK inhibitor, sensitizes CLL lymphocytes to chlorambucil. • Wortmannin is a noncompetitive, irreversible inhibitor of DNA-PK , whereas NU7026 (2-(morpholin-4-yl)benzo[h]chomen-4-one) is competitive inhibitor of the ATP site of DNA-PK • Although Wortmannin is primarily a PI 3-K inhibitor, being 90fold more active against PI 3-K than DNA-PK or ATM, NU7026 is more selective for DNA-PK with a 60-fold greater potency against this enzyme than PI 3-K and inactive against both ATM and ATR. Thus, in contrast to Wortmannin, NU7026 demonstrates excellent specificity for DNA-PK. NU7026 in CLL • (1-10uM)NU7026 synergistically(<1) sensitizes CLL lymphocytes to CLB in almost all(>15/19 samples). Similar sensitization occurs in the I83 CLL cell line. • This is associated with NU7026 inhibition of CLB-induced DNA-PK activity both in I83 cells and CLL lymphocytes( using FACS analysis) and NU7026 inhibition of repair of DSBs (using gH2AX ) NU7026 pharmacokinetics Following intravenous administration to mice at 5 mg kg, NU7026 undergoes rapid plasma clearance and this is largely attributed to extensive metabolism. Bioavailability following interperitoneal (i.p.) and p.o. administration at 20 mg kg(-1) was 20 and 15%, respectively. Investigation of NU7026 metabolism profiles in plasma and urine indicated that the compound undergoes multiple hydroxylations. NU7026 will have to be administered four times per day at 100 mg kg(-1) i.p. in order to obtain drug exposure required for radiosensitisation. Icos compounds • Icos corp made a series of IC compounds which are specific inhibitors of DNA-PK • These compounds also have problems with their pharmacokinetic parameters • These compounds were acquired by Luitpold corporation and they have modified these compounds to improve the pharmacokinetic parameters. • We have investigated the original IC compounds in CLL lymphocytes in colloboration with the Luitpold corporation. IC compounds compared to NU7026 • The IC compounds compare favorably with NU7026. • IC486241 appears to have the most favorable profile but all the IC compounds are active. • IC486241 sensitizes CLL lymphocytes to chlorambucil similar the results with Nu7026 • The Luitpold modification of the IC compounds should render them more useful clinically DNA-PK in colon cancer therapy • Irinotecan and oxaliplatin are major anticancer agents utilized in the treatment of metastatic colon cancer • We utilized two divergent colon cancer cell lines, the mismatch-repair deficient, p53 normal HCT-116 and the mismatch repair competent, dysfunctional p53 mutant HT-29 • Nu7026 and IC486241(ICC) specific DNA-PK inhibitors were utilized to test for synergy DNA-PK inhibitors in colon cancer • Modest reductions in IC50 values and a lack of synergy were observed with oxaliplatin in the presence of nontoxic concentrations of Nu7026 or IC486241 • In contrast, significant synergy was observed with SN38(activated irinotecan) in the presence of nontoxic concentrations of the inhibitors • This was associated with decreased activation of DNA-PK and greater DNA damage (comet assay) with presumably less DNA repair Homologous Recombinational Repair (HRR) in chlorambucil resistance in CLL • Since chlorambucil-induced ICLs are more rapidly repaired in resistant CLL lymphocytes, we also investigated the role of HRR • HRR can remove the ICLs in an error free fashion by utilizing non-damaged sister chromosones which are most readily available during DNA replication and cell division Mechanisms of drug resistance Panasci L et al. Clin Cancer Res 2001;7:454-461 ©2001 by American Association for Cancer Research CLB induces Rad51 Foci in primary CLL lymphocytes Christodoulopoulos G et al. Clin Cancer Res 1999;5:21782184 ©1999 by American Association for Cancer Research CLB-induced Foci correlates with CLB resistance Christodoulopoulos G et al. Clin Cancer Res 1999;5:21782184 ©1999 by American Association for Cancer Research c-abl phosphorylates Rad51 DNA DAMAGE BRCA1 c-Abl ATM Activation RAD51 c-Abl Activation BRCA1 Tyr 315 RAD51 RAD52 c-abl modulates Rad51-directed DNA Repair 1-c-Abl positively regulates Rad51-related Homologous Recombinational Repair 2-Homologous recombinational Repair is implicated in CLB drug sensitivity in CLL We investigate the effect of the c-abl inhibitor Imatinib/STI571/Gleevec in CLB cytotoxicity in CLL lymphocytes Determination of Drug Synergy Using the MTT Assay How we assess synergy CLB y = 109.53e 2 R = 0.9797 IC50=13.72M 120 100 80 80 % of Control 60 40 120 100 80 20 60 40 50 0 100 60 20 0 0 IC50= 2.8 M 40 20 0 20 40 0 60 0 STI571 (M) CLB (M) 5 10 CLB (M) IC50 CLB 5M STI571 120 IC50= 2.8 M 100 % of Control % of Control -0.0469x y = 106.63e-0.026x R2 = 0.9648 IC50=29.12M 100 CLB 5M STI571 % of Control 120 STI571 80 60 40 I= 20 0 0 10 I< 1 Synergy 20 30 CLB (M) 40 IC50 CLB IC50 CLB + [ STI571] IC50 STI571 50 I=1 Additive I> 1 Antagonism = 0.46 15 CLB induces phosphorylation of Ra51 Imatinib reduces CLB-induced Rad51 phosphorylation Mechanisms of imatinib cytotoxicity Chlorambucil Constitutive c-Abl activation of Lyn Fludarabine •Inhibition of transcription DNA damage Anti apoptotic signalling •Inhibition of DNA synthesis (cycling cells) Rad51-dependant DNA repair Survival APOPTOSIS c-abl kinase inhibition c-abl kinase Src kinase inhibition inhibition Dasatinib Gleevec Survival Mechanisms of imatinib cytotoxicity c-Abl inhibition sensitizes CLL lymphocytes to chlorambucil independently of the clinical status (untreated vs. treated ). The mechanisms involves increased apoptosis and decreased homologous recombinational repair. STI571 Chlorambucil C-abl activation C-Abl inhibition by STI571 (imatinib) decreases chlorambucil induced-RAD51 phosphorylation and Rad51 Foci Rad51phosphorylation Apoptosis c-Abl inhibition by STI571(gleevec) in the absence of DNA damage results in CLL lymphocytes apoptosis Rad51 Foci STI571 and chlorambucil cytotoxicity appear to be mediated by different mechanisms DNA repair STI571 is a promising agent to utilize with chlorambucil in the treatment of CLL patients Drug sensitization Phase I trial of imatinib and chlorambucil in previously treated CLL • : The three dose levels studied included imatinib at 300, 400, or 600 mg/day. Imatinib was given on days 1-10 and chlorambucil (8 mg/m2 daily) was given on days 3-7 of a 28-day cycle (up to 6 cycles). • Eleven patients participated in this study. Low grade gastrointestinal toxicities were observed in a dose-dependent manner. Forty-five percent of patients responded (2 unconfirmed CRs and 3 PRs). Two responding patients were fludarabine-refractory • in vitro IC50 of chlorambucil in the presence of 5 uM imatinib in CLL lymphocytes correlated with the decrease in lymphocyte counts on day 15. • Imatinib plasma concentrations achieved in patients were in the range of those effective in in vitro sensitization • The combination of chlorambucil and imatinib in patients with previously treated CLL was well tolerated and showed evidence of clinical efficacy. Future studies • DNA-PKcs detailed crystal structure determined ( Nature 2010 463:118-21)– better inhibitors? • We are designing combi-molecules with Dr Jean-Claude combining c-abl inhibitors and bifunctional alkylating agents • The first molecule incorporating imatinib and a chlorambucil-like molecule(ZRF4) has increased activity in-vitro against CLL lymphocytes than the individual components • Newer more potent c-abl inhibitors will be utilized to exploit this concept Acknowledgements • • • • • Lilian Amrein, PhD Research Associate Veronica Marignac, PhD Research Associate David Davidson, PhD postdoctoral fellow Jeremy Grenier Mcgill student Collaborators: Dr Raquel Aloyz & Dr Jean-Yves Masson Reference on NHEJ/HR/MRN Lamarche B FEBS letters 584:3682, 2010