Obstetric Anesthesia - UC San Diego Health Sciences
advertisement

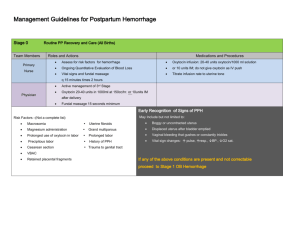
Complications in OB PACU Tom Archer, MD, MBA Director, OB Anesthesia UCSD Hillcrest August 16, 2012 OB PACU Complications • Patient S/P general anesthesia • Poor pain control • Post-partum hemorrhage • Preeclampsia– Dr. Kelly has already discussed • Separate talk on respiratory problems later. Patient S/P general anesthesia • We are not used to these patients! • Sleepy, disoriented, more pain, sore throat, nausea, anxious. • Potential airway problems – S/P intubation – Pregnant airway is swollen to start with. – Residual neuromuscular blocking agent Patient S/P general anesthesia • Hopefully anesthesiologist has given ample IV narcotic in OR. But is it long-acting (morphine or dilaudid)? Fentanyl will wear off quickly. • Antiemetics frequently used and helpful. • Ketorolac (Toradol) may be helpful (as in neuraxial anesthesia patients). Poor pain control • More common with GA. • Ask anesthesiologist if patient got IT or epidural morphine. • Ketorolac • Chronic pain patients may need a pain service consult. Ketorolac (Toradol) • Excellent NSAID analgesic. • Contraindicated in renal disease, GI ulcers, coagulopathy and NSAID allergy. • At UCSD we are not giving it at present in preeclampsia patients because of possible renal impairment. Ketorolac • Package insert says “contraindicated in breastfeeding mother” but American Academy of Pediatrics endorses its use in these patients. • Common dosage regimen is 30 mg q6h x 4 doses (not days!), then stop. Postpartum hemorrhage (PPH) • Vital sign changes: First to increase is RR, then HR, last to change (decrease) is BP! • Hemorrhage can be occult. • Neuraxial blocks also lower blood pressure. • Get anesthesia involved early. PPH in PACU • Diagnose PPH on clinical grounds. You don’t have to wait for labwork. • Start a second large-bore IV and draw labs from the IV catheter before hooking up the fluid. • Warm fluids early (often forgotten in the rush). Hypothermia exacerbates coagulopathy. PPH in PACU • Arterial line is often very helpful (BP measurement and repeated labwork). If you are going to get one ABG, consider an arterial line. • Be willing / able to go to OR early before the situation becomes dire. • GA often necessary in hemorrhage patient. Neuraxial may bottom-out the BP. California Pregnancy-related Mortality Review Composite Case Example: 24yo G2 P1 at 38 wks gestations induced for “tired of being pregnant”: • • • • • • • • • After 8hr active phase and 2 hr 2nd stage, had a NSVD of an 8lb 6oz infant. After placental delivery, she had an episode of atony that firmed with massage. A second episode responded to IM methergine and the physician went home (now 1am). The nurses called the physician 30 min later to report more bleeding and further methergine was ordered. 60min after the call, the physician performed a D&C with minimal return of tissue. More methergine was given. 45 min later a second D&C was performed, again with minimal returns. EBL now >2,000 ml. Delays in blood transfusion because of inability to find proper tubing. Anesthesia is delayed, but a second IV started for more crystaloid. VS now markedly abnormal, P=144, BP 80/30. One further methergine given and patient taken for a 3rd D&C. Now has gotten 2u PRBCs After D&C is complete, she had a cardiac arrest from hypovolemia /hypoxia and was taken to the ICU when she succumbed 3 hours later. CMQCC maternal hemorrhage 11 Doctor’s Company Review COMMUNICATION BREAKDOWNS Among Team Members… For example, • Obstetrician and anesthesiologist regarding efficacy of intervention(s) and need to escalate care or change strategy. • Operating room and blood bank concerning urgency of situation. • Among support personnel concerning delivery of products and location of specialized equipment (I.e rapid infusion devices or specialized kits) Doctors Company Reviews Maternal Arrests Cases (Reprinted with permission from The Doctors Company); APSF NEWSLETTER Summer 2007; page 28; Ann Lofsky, MD. 12 Avoid “delay and denial”. • DELAY. “Let’s check a ‘crit… we couldn’t get a blood sample for the lab… couldn’t find the right tubing…couldn’t find the form…couldn’t find the Attending…it was 3AM…” • DENIAL. “This can’t be happening.” “It will stop soon”. “Just give it time.” Don’t do this: • Get derailed by details or secondary issues: – Arterial line (if you can’t get it quickly) – Central line – ABG, checking base deficit – Checking hematocrit, coagulation studies • These things are important, but secondary to IV access and blood availability. Prioritize! Do this: • Function as a (respectful) team. Get help. Call OB and Anesthesia early. Start second IV. • Call Blood Bank early. Do they have a sample? • Be willing to act on clinical signs (pallor, hypotension, tachycardia, altered mentation, decreased urine output). Don’t have to wait for lab results!! Think ahead on 4 fronts simultaneously: • Resuscitation (IV access, blood availability) • Upcoming anesthesia needs and risks (airway, sympathectomy, etc.) • What is causing this problem? Can you help the OB make the Dx? • Logistics (getting to OR, tech support, etc.) What causes PPH: The 4 T’s • Tone (by far commonest cause of PPH)– 80% • Trauma (cervix, vagina– speculum exam with good light and anesthesia will be required. Also think ruptured uterus and pelvic hematoma (not visible on spec exam)– 15% • Tissue (retained membranes, placenta)– 4% • Thrombin (DIC)—1% UCSD OB hemorrhage protocol • Foster communication between OB, midwives, anesthesia, nursing and blood bank. • Rapidly obtain best blood products available for patient, given the available information. Guts of OBHP • Any attending can activate it. Tell charge nurse “I want to activate the OBHP.” • Call Blood Bank (BB). Give patient name and MRN, MD name and PID#. Explain what is going on. • Designate one person to communicate with BB • Designate one person to take paperwork to BB and blood from BB. Guts of OBHP • Charge nurse will give you “Request for Emergency Blood” form. • Does BB have patient blood sample? If not, patient will get type O, preferably Rh neg blood. • If yes, patient will get type specific blood, either cross-matched or uncrossmatched. Guts of OBHP • Transfuse 1:1:1, RBC:FFP:platelets • If you need to send a patient blood sample to the BB, try to make it 7 mL purple top. • If you can, get baseline: CBC (lavender top), fibrinogen, PT and PTT (blue top), wall clot (red top). Key technical issues • Early and adequate IV access. • Warm fluids and patient. • Early, clear communication with blood bank (one designated person). • Always think ahead. What will the next step be? Move along (progress) and think ahead! What will we need to do next? 24 24 Remember the 4 uterotonic drugs • Oxytocin -- IV • Methylergonovine (“Methergine”) -- IM • Carboprost (“Hemabate”) -- IM • Misoprostol (“Cytotec”) -- PR Other technical issues • Patient blood sample CAN be drawn from an IV. • Arterial line very helpful but don’t perseverate. IV access trumps art line. • A SECOND blood sample will be required if one is not already on file (“ABO recheck”). Other technical issues • Blood in closed cooler is OK for 4 hours. • “FFP” is no longer frozen. It is “thawed plasma”. • Patient blood sample is “good” for 3 days for use in T+S or T+C • Historical blood type is no good for transfusion. What happens to the patient blood sample in the Blood Bank? • “Hold specimen” (often incorrectly called “hold clot” or “type and hold”. Unclotted tube of blood is just held for possible later Type and Screen. • “Type and screen”– patient blood type and Rh is determined (“type”). Patient serum is checked for antibodies to wide variety of RBCs (“screen” takes 45 minutes). • “Type and cross”– patient serum is checked for antibodies against donor unit RBCs (5 minutes, usually done on computer if T+S is negative). Pictured above: L. Gioia, MD, A. Miller, RN, A. Hall, RN and other members of the L&D staff during a “Code Noelle” drill. Summary • Attempt to foresee likely hemorrhage cases (prolonged labor, infected or distended uterus, magnesium Rx, grand multiparity). • Make sure Blood Bank has blood sample. • Has BB done a T+S or T+C? • When hemorrhage occurs– CALL BB EARLY! Summary • Key technical issues are: – Adequate IV access (at least two big IVs) – Keep patient warm – Availability of blood – Swift Dx and Rx (requires safe anesthesia) – Consider going to OR early (conveys urgency and gravity of problem, provides good lighting, access to problem, anesthesia). Summary • Key organizational issues are: – Avoid “DENIAL and DELAY”. – Good communication between OB, anesthesia and nursing – Call BB early – Resource mobilization (extra help, techs, attendings, etc.) The End