CA-MRSA - Hkmacme.org
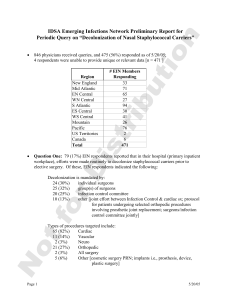
advertisement

Dr. Mona, Chiu Lai Shan, 趙麗珊 Specialist in Dermatology and Venereology 1. 2. 3. S. aureus skin infection Epidemiology and clinical characteristics of CA-MRSA Approach to CA-MRSA skin infection Colonize the anterior nares in one third of healthy population Colonize the skin of most atopic dermatitis patients (up to 100% in those with severe AD) Common pathogen for skin infection Notorious for secretion of various toxins and superantigens (TSST, enterotoxin) which can cause serious infection and promote inflammation Local Cellulitis Abscess Carbuncle Furuncle Impetigo Necrotizing fasciitis systemic Staphylococcus scalded skin syndrome Toxic shock syndrome Epidemiology -local prevalence -occupation -hobby -travel history Clinical features Laboratory -antibiotic resistance profile 1981-CA-MRSA outbreak was first described in United States in a group of intravenous drug users 1990s-multiple CA-MRSA outbreaks were documented among different states in the United States 1999-identify as a virulent pathogen after it was identified as the causative organism in the death of four previously healthy children in Minnesota and North Dakota 2004-CA-MRSA was referred as “ an emerging epidemic” PR Cohen. International Journal of Dermatology 2007. 46:i-11 Methicillin resistance is mediated by the methicllin resistance gene: mecA gene The gene is responsible for beta-lactam resistance by encoding the methicillinresistant penicillin binding protein 2a (PBP2a) which has a low affinity for beta-lactam type antibiotics The genetic elements that carries the mecA gene is the staphylococcal cassette chromosome (SCC) HA-MRSA infection is associated with SCCmec type I, II, III CA-MRSA infection is associated with SCCmec type IV and V which lacks other multidrug resistance genes CA-MRSA is more frequently associated with exotoxins than the HA-MRSA counterpart Panton-Valentine leukocidin (PVL) toxin is the most common toxin It is lethal to neutophils and is a potent dermonecrotic toxin. It is also associated with necrotizing pneumonitis HA-MRSA CA-MRSA Patient population Acquired after staying more then 48 hours in the hospital Community without exposure to the hospital environment Pre-disposing factors Surgery, intubation, catheter, dialysis, prior MRSA infection, long term care facility Members of military, IVDU, homosexual males, children, athletes, inmates, Pregnant women, chidren and infants Virulent factors SCCmec type I to III SCCmec type IV or V, PantonValentine leukocidin Clinical presentations Systemic infection such as UTI and pneumonia Most common soft tissue and skin infection Antibiotic resistance profile Resistant to most antibiotics except few (e.g.vancomycin, linezolid) Resistant to beta-lactam group of antibiotic but susceptible to quinolones and trimethoprim. Topical fusidic acid and mupirocin. Some are susceptible to clindamycin Large population based survey in the United States showed a 0.84% of overall MRSA colonization rate versus 31.6% of MSSA Worldwide, the overall MRSA colonization rate range from 0.26% to 9.2% The overall prevalence of MRSA is around 1.4% in our locale and most of them are associated with health-care exposure The prevalence is similar in the United Kingdom (1.5%) and <1% in Italy, Portugal and Canada The rate of MRSA colonization is higher in healthy school children in Asian countries: 5.1% in South Korea, 4.3% in Japan, and 1.9% in Taiwan There were significant differences in the prevalence of MRSA among distinct regions of China, with the highest prevalence, 76.9%, in east China, 52.3% in the southwest and about 60% in other regions The prevalence of MRSA in certain cities such as Shanghai, Beijing, and Guangzhou was high relative to other 32.7% of S. aureus isolated from pediatric patients was MRSA, which was about half that seen in adult patient The incidence of CA-MRSA in children with skin and soft tissue infections was 1.1–4% in Beijing Similar in other major provinces MRSA among patients presenting to the emergency department with purulent SSTI were studied over a 4-month period from November 2006 to February 2007. It involved the emergency departments in six regional hospitals estimated to provide service to half of the 6.6-million inhabitants in Hong Kong Wound swabs were obtained for culture from all patients who present with purulent SSTIs of less than 7 days duration A total of 298 patients aged 2 to 97 with purulent SSTIs were recruited S. aureus was isolated from 126 (42%) patients Among patients with purulent SSTIs, 10% (13/125) of all S aureus isolates was attributed to PVL-positive communityassociated MRSA MRSA was isolated from 5% (13/241) of abscesses, 13% (5/40) of infected wounds, and 17% (1/6) of purulent discharges associated with cellulitis In univariate analysis, Filipino ethnicity was significantly more likely than Chinese to be infected by PVL-positive communityassociated All other clinical and epidemiologic features were not predictive of PVL- positive community-associated MRSA Most common complain “spider bite” lesions Morphology: Papules Pustules Erythematous or crusted erosions Plaques Nodules Distribution Legs Knees Thighs Feet Buttock • • • • • • Abscess Cellulitis Folliculitis Furunculosis Impetigo Paronychia Severe infection: Necrotizing fasciitis Bullous erysipelas Staphylococcus scalded skin syndrome and staphylococcus toxic shock syndrome Purpura fulminans Ecthyma gangrenosum All are resistance to Beta-lactam group of antibiotics Most are susceptible to ciprofloxacin, rifampacin, cotrimoxazoles, vancomycin, mupirocin and fusidic acid Most are resistance to erythromycin Some are resistance to Clindamycin Resistance to older generation of fluoroquinolones is observed Resistance rates of 57.1–85.7% to macrolides, clindamycin, aminoglycosides, sulfamethoxazole-trimethroprim, quinolones, and tetracycline Resistance rate to rifampicin was 28.6% Y.-H. Xiao et al. Drug Resistance Updates 14 (2011) 236–250 Antibiotic susceptibilities of community-acquiredStaphylococcus aureus isolates recovered from children at Texas Children's Hospital from 1 August 2001 through 31 July 2004. Kaplan S L et al. Clin Infect Dis. 2005;40:1785-1791 © 2005 by the Infectious Diseases Society of America Chung HJ et al. Journal of Clinical Microbiology 2008. 46(3):991-995 - - Clues for CA-MRSA infection In area of high prevalence Highly susceptible groups Contact history ?more pus and discharge due to presence of PVL toxins Antibiotic susceptibility profile 1. 2. 3. 4. 5. 6. 7. 8. Thorough medical history and social history Clinical examination: abscess, cellulitis Risk evaluation: life threatening condition (necrotizing fasciitis) Appropriate culture before empirical antibiotic treatment Drainage of collections Review culture results and clinical response Report any confirmed case and contact tracing Follow up and decontimination Decolonization in infected persons is indicated in preventing recurrence and transmission of CA-MRSA Common decolonizing regime: 7.5%/10% povidine iodine soap, 4% chlorhexidinegluconate liquid detergent, triclosan preparations, mupirocin Active contact tracing and MRSA decolonisation with daily nasal mupirocin and chlorhexidine detergent for showers for 5 days are offered to all carrier is the current regime used in Hong Kong CA-MRSA is an emerging epidemics Skin and soft tissue infection is the most common site of CA-MRSA infection Prompt treatment is needed to prevent bacteremia which can lead to life threatening conditions such as necrotizing pneumonia Incision and drainage is the most effect treatment for abscesses The choice of empirical antibiotics depends on different localities as resistance profiles varies a lot at different countries