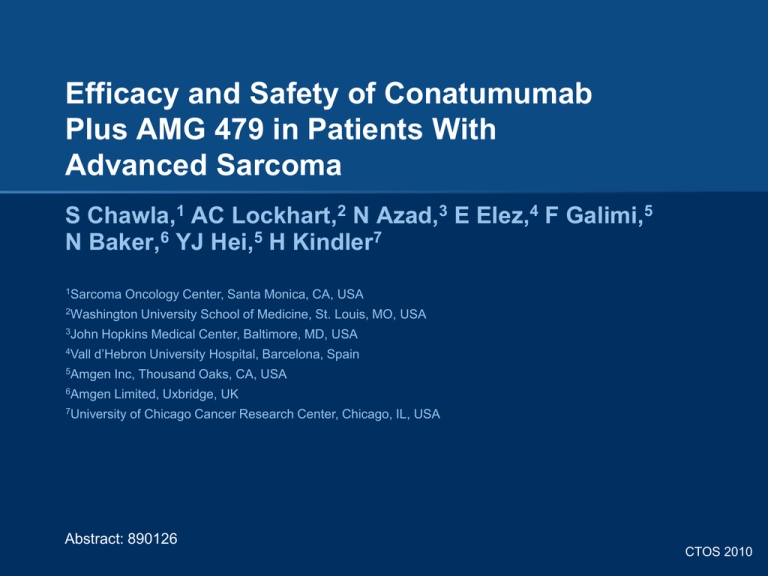
Efficacy and Safety of Conatumumab
Plus AMG 479 in Patients With
Advanced Sarcoma
S Chawla,1 AC Lockhart,2 N Azad,3 E Elez,4 F Galimi,5
N Baker,6 YJ Hei,5 H Kindler7
1Sarcoma
Oncology Center, Santa Monica, CA, USA
2Washington
3John
4Vall
University School of Medicine, St. Louis, MO, USA
Hopkins Medical Center, Baltimore, MD, USA
d’Hebron University Hospital, Barcelona, Spain
5Amgen
Inc, Thousand Oaks, CA, USA
6Amgen
Limited, Uxbridge, UK
7University
of Chicago Cancer Research Center, Chicago, IL, USA
Abstract: 890126
CTOS 2010
INTRODUCTION
AMG 479 Mechanism of Action
• AMG 479 is an investigational, fully human monoclonal antibody
against the type 1 insulin-like growth factor receptor (IGF1R)
– Binds to IGF1R and prevents binding of its ligands, IGF-1 and IGF-21
CTOS 2010
INTRODUCTION (continued)
Conatumumab Mechanism of Action
• Conatumumab is an investigational, fully human monoclonal antibody
against human death receptor 5 (DR5)
– Binds to DR5, activates caspases, and induces apoptosis2
CTOS 2010
INTRODUCTION (continued)
• IGF1R inhibition and DR5 stimulation inhibit the growth of sarcoma
cells3,4
• In preclinical models, activation of IGF1R can lead to resistance to
DR5-induced apoptosis5
• Combining AMG 479 with conatumumab may prevent DR5 agonistresistant cells from escaping apoptosis
• A multicenter, open-label, phase 1b/2 study was conducted to
investigate the efficacy and safety of conatumumab plus AMG 479 in
patients with advanced solid tumors (phase 1b) and advanced nonsmall cell lung cancer (NSCLC), colorectal cancer (CRC), pancreatic
cancer, ovarian cancer, or sarcoma (phase 2)
• Among 4 patients with soft tissue sarcoma in the phase 1b study, 1
had stable disease (SD) for 24 weeks and 1 had SD after > 1 year on
treatment6
• Here we present the results for sarcoma patients enrolled in the phase
2 study
CTOS 2010
PHASE 2 STUDY OBJECTIVE
• To estimate the efficacy of conatumumab in combination
with AMG 479 as measured by the objective response rate
(ORR)
CTOS 2010
METHODS
Phase 2 Study Schema
Planned N = 15 per cohort
Sarcoma
AMG 479 18 mg/kg
Conatumumab 15 mg/kg
KEY ELIGIBILITY
• Confirmed locally advanced or
metastatic disease
• Measureable disease
• ≥ 16 years old
• ECOG PS of 0 or 1
• Adequate organ function
• Informed consent
• No uncontrolled CNS disease
• No anti-cancer therapy ≤ 28
days before enrollment
• No prior treatment with DR
agonists nor IGF1R
antagonists
aIf
NSCLC (squamous)
AMG 479 18 mg/kg
Conatumumab 15 mg/kg
E
N
R
O
L
L
M
E
N
T
NSCLC (non-squamous)
AMG 479 18 mg/kg
Conatumumab 15 mg/kg
Pancreatic
AMG 479 18 mg/kg
Conatumumab 15 mg/kg
Ovarian
AMG 479 18 mg/kg
Conatumumab 15 mg/kg
Sarcoma
AMG 479 18 mg/kg
Conatumumab 15 mg/kg
eligible.
Two interim analyses of safety data were
conducted after at least 15 patients and
then 45 patients were enrolled and had
completed 1 cycle of treatment.
CRC
AMG 479 18 mg/kg
Conatumumab 15 mg/kg
Every 3 weeks for ≤ 24 months
C
O
N
T
I
N
U
A
T
I
O
N
O
F
T
R
E
A
T
M
E
N
T
L
O
N
G
T
E
R
M
F
O
L
L
O
W
U
P
CTOS 2010
METHODS (continued)
Study Design
• Multicenter, open-label, phase 1b/2 study of conatumumab in
combination with AMG 479
• In the phase 1 study, the planned maximum target dose of
conatumumab (15 mg/kg every 3 weeks) was determined to be safe
and well tolerated (as determined by the incidence of dose-limiting
toxicities)
• The phase 2 study was opened for enrollment after the maximum
target dose of conatumumab was determined
• Patients received AMG 479 (18 mg/kg) followed by conatumumab
(15 mg/kg) IV every 3 weeks for up to 24 months or until disease
progression, intolerable adverse event, death, withdrawal of consent,
or administrative decision
• Tumors were imaged by CT or MRI every 6 weeks for 6 months and
every 8 weeks thereafter
CTOS 2010
METHODS (continued)
Endpoints
• Primary: ORR
– Confirmed complete response (CR) plus partial response (PR) by
RECIST v1.0 per investigator review
• Secondary: time to response, duration of response,
progression-free survival, incidence of adverse events and
laboratory abnormalities, incidence of anti-conatumumab
or anti-AMG 479 antibody formation, and PK (Cmax and
Cmin for conatumumab and AMG 479)
CTOS 2010
RESULTS
Patient Disposition
n (%)
Patients enrolled
Sarcoma Patients All Patientsa
16
70
Patients who received conatumumab 15 (94)
and AMG 479
68 (97)
Patients who discontinued
conatumumab and AMG 479
12 (75)
50 (71)
Ineligibility determined
0 (0)
1 (1)
2 (13)b
4 (6)c 3 (4)d
Full consent withdrawn
0 (0)
3 (4)
Lost to follow-up
0 (0)
1 (1)
Death
0 (0)
1 (1)
Partial consent withdrawn
0 (0)
1 (1)
Other
0 (0)
1 (1)
10 (63)
38 (54)c 39 (56)d
Adverse event
Disease progression
• Median number
of infusions
per patient = 2
(range, 1 to 7)
aIncludes
sarcoma (n = 16), squamous NSCLC (n = 4), non-squamous NSCLC (n = 11), CRC (n = 16), pancreatic
cancer (n = 16), and ovarian cancer (n = 7). bDiscontinued AMG 479 and conatumumab, 1 due to grade 3
gastrointestinal hemorrhage (not attributed to study drugs); and 1 due to grade 3 constipation, somnolence, and
peripheral motor neuropathy (not attributed to study drugs). cDiscontinued conatumumab. dDiscontinued AMG 479.
CTOS 2010
RESULTS (continued)
Patient Demographics
Sarcoma
(N = 15)a
All Patients
(N = 68)a
Male
5 (33)
35 (51)
Female
10 (67)
33 (49)
14 (93)
58 (85)
Black or African American
0 (0)
5 (7)
Hispanic or Latino
1 (7)
2 (3)
Asian
0 (0)
3 (4)
Sex - n (%)
Race/ethnicity - n (%)
White or Caucasian
Age (years) at randomization
Median (range)
54.0 (29 to 65) 58.5 (29 to 83)
Age group at randomization - n (%)
aSafety
< 65 years
14 (93)
47 (69)
≥ 65 years
1 (7)
21 (31)
≥ 75 years
0 (0)
4 (6)
analysis set. Two patients, 1 with sarcoma and 1 with squamous NSCLC, did not receive study drugs.
CTOS 2010
RESULTS (continued)
Baseline Disease
n (%)
Sarcoma
(N = 15)
Bone sarcoma
Ewing
Fibrosarcoma
Osteosarcoma
3 (20)
1 (7)
1 (7)
1 (7)
Soft tissue sarcoma
Leiomyosarcoma
Synovial sarcoma
Myxoid liposarcoma
Low grade myofibroblastic sarcoma
Connective tissue sarcoma
Malignant peripheral nerve sheath sarcoma
Undifferentiated pleomorphic sarcoma
12 (80)
5 (33)
2 (13)
1 (7)
1 (7)
1 (7)
1 (7)
1 (7)
Disease stage at enrollment
Stage III
Stage IIIA
Stage IV
1 (7)
0 (0)
14 (93)
ECOG performance status at screening - n (%)
0
1
6 (40)
9 (60)
• Prior treatment
– Surgery, 14 (93%)
– Radiotherapy, 11 (73%)
– Chemotherapy, 15 (100%)
Safety analysis set.
CTOS 2010
RESULTS (continued)
Tumor Response
n (%)
Patients with measurable disease at baseline
Number of objective responders
Best overall response assessmenta
Confirmed CR
Confirmed PR
SD
Progressive disease
Sarcoma
(N = 15)
15
0 (0)
0 (0)
0 (0)
5 (33)
10 (67)
aA
best overall response of SD required a radiologically determined response of SD or better no earlier
than study day 35.
CTOS 2010
RESULTS
Prolonged SD
Tumor Type
Duration of SD
38-year-old
Hispanic female
Synovial sarcoma
46 weeks
Still on treatment
58-year-old
white female
Leiomyosarcoma
41 weeks
51-year-old
white male
Neurofibrosarcoma
18 weeks
• Two other patients had SD at the week-6 assessment
• All 5 SD patients had multiple lines of prior anticancer
therapy, which failed
CTOS 2010
RESULTS (continued)
Safety
n (%)
Sarcoma
(N = 15)
Patients reporting at least 1 AEa
Pyrexia
Back pain
Chills
Nausea
Fatigue
Vomiting
Abdominal pain upper
Rash
11 (73)
4 (27)
4 (27)
3 (20)
3 (20)
2 (13)
2 (13)
2 (13)
2 (13)
Grade 3 AEs
Abdominal pain upper
Constipation
Gastrointestinal hemorrhage
Peripheral motor neuropathy
Somnolence
3 (20)
1 (7)
1 (7)
1 (7)
1 (7)
1 (7)
Patients with conatumumab-or AMG 479-related AEs
8 (53)
• There were no grade
4 or grade 5 AEs
• There were no grade
≥ 3 conatumumab- or
AMG 479-related AEs
Safety analysis set.
aIn at least 2 patients. AE, adverse event.
CTOS 2010
CONCLUSIONS
• In this diverse and heavily pre-treated population of
sarcoma patients:
– Conatumumab plus AMG 479 was well tolerated
– Prolonged SD (18 to 46+ weeks) was observed in 3 patients
• Further study of this drug combination may be warranted
CTOS 2010
REFERENCES
1. Beltran PJ, et al. Mol Cancer Ther. 2009;8:1095-1105.
2. Kaplan-Lefko PJ, et al. Cancer Biol Ther. 2010;9:618-631.
3. Ashkenazi A and Herbst RS. J Clin Invest. 2008;118:1979-1990.
4. Olmos D, et al. Cancer J. 2010;16:183-94.
5. Amgen data on file.
6. Chawla SP, et al. J Clin Oncol. 2010;28:abstr 3102.
CTOS 2010
ACKNOWLEDGEMENTS
• This trial was sponsored by Amgen Inc., ClinicalTrials.gov ID:
NCT00819169
• Kathryn Boorer from Amgen Inc. provided writing assistance
CTOS 2010