Module 5a: Documenting Heart Failure
At the conclusion of this module, the learner will be able to:
1.
Differentiate between systolic and diastolic heart failure
2.
Describe three clinical indicators of acute heart failure
3.
Define acute cor pulmonale
Heart, due to impairment of structure or function, does not pump effectively
Because oxygenated blood is not effectively pumped forward into the circulation, tissues do not receive nutrients and oxygen
Fluid backs up within the circulatory system leading to peripheral and pulmonary edema
(“congestive heart failure”),
Most common cause is coronary artery disease
Documenting “CHF” is insufficient!
CMS guidelines require
acuity
and
specificity
.
Incomplete documentation of heart failure has a significant impact on severity of illness, risk of mortality, GLOS, and case mix index.
Incomplete documentation affects treatment modalities, core measures, and communication.
Incomplete documentation affects patient care.
Documenting NYHA classifications is
CMS
not
adequate documentation of heart failure for
Is it systolic, diastolic, or combined?
EF = % of blood volume pumped out with each stroke
Usually refers to left ventricle, but right ventricle EF may also be measured
Commonly diagnosed by ECHOcardiogram, but may also be measured during stress test or cardiac catheterization
Ejection fraction is a key clue as to type of heart failure
Ejection fraction < ~ 50%
Result of impaired inotropic state – heart can’t empty
Causes include dilated cardiomyopathy, myocardial infarction
Treated with ACE-inhibitors or ARBs – core measures; Digoxin, judicious use of βblocker
Core measure HF-3: pts w/LV systolic dysfunction (EF < 40%) prescribed ARB or
ACE-i
Ejection fraction > ~ 50 %
1/3 of patients with symptomatic heart failure have “normal” EF
Risk increases with age
Result of impairment in heart’s ability to relax – heart can’t fill
May see elevated filling pressures “stiff ventricle”
Causes include restrictive and hypertrophic cardiomyopathy, ischemia, HTN, senile cardiac amyloid, constrictive pericarditis, myocardial ischemia
Treatment differs from systolic HF – β-blockade
It is possible to have elements of both systolic and diastolic heart failure
Physician should not write, “both,” or
“combined,” because the coders can’t code from that
Physician needs to specify, “systolic and diastolic”
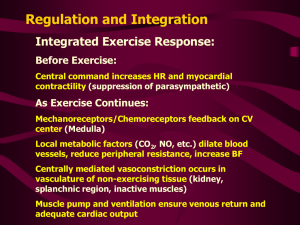
Is it acute, chronic, or acute on chronic?
Usually – but not always – systolic
Develops suddenly without prior history
May have sudden reduction in cardiac output
May be hypotensive
May not show peripheral edema
Can be documented as “acute” or
“decompensated” heart failure
Develops slowly
May be seen in patients with dilated cardiomyopathy, valvular heart disease
Often has normal blood pressure but with peripheral edema
Patients coming from home with heart failure medications – if you continue those meds, are you treating a chronic condition?
Patient has pre-existing chronic condition that worsens
Can be documented either as “acute on chronic” or “exacerbation”
Check the BNP – is it elevated?
Check the ECHO results – what is the EF? How does the cardiologist describe LV function?
What are the pt’s clinical signs/symptoms?
◦ Dyspnea, hypoxia
◦ Rales/rhonchi
◦ Peripheral edema
◦ JVD
◦ S3 gallop
How is the heart failure being treated?
◦ IV diuresis usually means an acute condition!
◦ No change in home HF meds usually means chronic
SI/IS for heart failure
Need documentation of diagnosis, physical assessment to support diagnosis, documented evidence of cardiopulmonary instability, treatment per core measures
(unless contraindicated), evaluation of LV systolic function, assessment of oxygenation and treatment with supplemental oxygen, use of cardiac monitoring
Heart failure can be monitored and treated in an observation status – not an automatic IP
Severity of illness & geometric length of stay
“CHF” does nothing to increase relative weight and CMI
Acute heart failure, documented as systolic, diastolic, or systolic & diastolic, is a major co-morbidity that increases relative weight and CMI
Two patients with the same presentation and same treatment, documented differently, can have dramatically different relative weights,
CMI, and geometric lengths of stay
Patient admitted with atrial fibrillation, develops signs of acute heart failure, EF is
60%
◦ Physician documents AF, CHF
DRG 310, GLOS 2.0 days, RW 0.5608
◦ Physician documents AF, acute diastolic heart failure
DRG 308, GLOS 4.0 days, RW 1.2283
Patient admitted with intracranial hemorrhage, has been taking Lisinopril for previously diagnosed heart failure, meds are continued and patient placed on telemetry.
ECHO done in June showed EF of 30%
◦ Physician documents ICH, hx systolic dysfunction
DRG 66, GLOS 2.6 days, SOI 1, RW 0.8105
◦ Physician documents ICH, chronic systolic heart failure
DRG 65, GLOS 3.8 days, SOI 2, RW 1.8555
Patient admitted with CAD, hx systolic HF, undergoes CABG; postoperatively cannot handle fluid resuscitation, requires extensive diuresis and increased oxygen requirement, spends extra 2 days in the hospital
◦ Physician documents CAD, fluid overload
DRG 236, GLOS 6.0 days, RW 3.7720
◦ Physician documents CAD, systolic HF exacerbation
DRG 235, GLOS 9.3 days, RW 5.9063
Getting acuity and specificity into the medical record
Dr. Jones:
“CHF” is documented in the medical record.
The record indicates moderate dyspnea, bilateral rales and rhonchi. BNP is 9400. ECHO shows ejection fraction of 35%. Orders for oxygen, PO Lisinopril and IV
Bumex. CMS requires acuity and specificity in documentation of heart failure. To establish the most accurate severity of illness of your patient, please specify the type (systolic, diastolic, or systolic & diastolic), and acuity (acute, chronic, or acute on chronic) of heart failure you are treating. For continuity of the record, please document in the progress notes and continue through to the discharge summary.
Type of right-sided heart failure
Acute cor pulmonale = acute lung disease
(e.g., PE, ARDS, COPD exacerbation) causing acute right sided heart failure
Chronic cor pulmonale = right sided heart failure resulting from pulmonary hypertension, chronic lung disease, or pulmonary valve stenosis
◦ Right ventricle dilates from chronic ischemia and hypertension of the arteries in the lungs
◦ Ventricle unable to pump against the hypertension
Acute onset of dyspnea
JVD
Hypotension
Hypoxia
Tachycardia
Shock
S3/S4 on inspiration
Fatigue
Exertional dyspnea
Ascites
Hepatomegaly
Dependent edema
Cardiomegaly
Syncope
Acute Chronic
CXR: RV and pulmonary artery enlargement
EKG: RV hypertrophy (R axis deviation, QR wave in V
1
, dominant R wave in V
1 patient due to realignment of the heart to V
3
)
◦ Both CXR and EKG results may be skewed in COPD
ECHO: evaluate LV and RV function, likely to see RV thickening and increased PA pressures
◦ Often limited by lung disease
Right heart catheterization
Cor Pulmonale, Merck Manual for Healthcare Professionals
Be aware of combination codes in ICD-10.
ICD-9
415.0 acute cor pulmonale
ICD-10
I26.01 septic pulmonary embolism with acute cor pulmonale
415.12 septic pulmonary embolism
Not coded as heart failure. There is no code in heart failure DRGs for right sided heart failure.
As PDx, cor pulmonale goes to DRG 316, other circulatory system diagnoses.
As SDx, acute cor pulmonale is a major comorbidity.
Can occur due to many causes
When found in patient with heart failure, is considered integral to disease and is not coded EXCEPT
◦ Physician can state that the pleural effusion is clinically significant, apart from the heart failure, or is not due to the heart failure (look for evidence of different etiology for the pleural effusion)
◦ If treatment of pleural effusion is not the same as that for heart failure (e.g., performing a thoracentesis—not routine tx for HF!), then the pleural effusion can also be coded
1.
Mrs. Gonzales is admitted with shortness of breath, rales in the bases; CXR indicates bilateral effusions, BNP is 12,400, EF is 28%; IV Lasix is ordered. The physician documents CHF with pleural effusion. Your most likely action is: a.
Code pleural effusion as PDx and query for acute systolic HF as SDx b.
Query for acute systolic HF as PDx and do not code the pleural effusion c.
Query for acute systolic HF as PDx and query for transudative pleural effusion as SDx d.
Code CHF as PDx and query whether the pleural effusion is related to the CHF
2.
On day 2, Mrs. Gonzales’s pulmonologist decides to perform a thoracentesis of the pleural effusion. Your most likely action is to: a.
Code the pleural effusion as PDx because that is the focus of the care b.
Not code the pleural effusion because it is inherent in heart failure c.
Code the pleural effusion as SDx because the treatment is outside the scope of heart failure d.
Query for acute respiratory failure due to the thoracentesis.
3.
A good way to remember the difference between systolic and diastolic heart failure is: a.
Systolic means the heart can’t fill; diastolic means the heart can’t pump b.
Systolic means the left ventricle is preserved; diastolic means the right ventricle is preserved c.
Systolic means the heart failure is acute; diastolic means the heart failure is chronic d.
Systolic means the heart can’t pump; diastolic means the heart can’t fill
4.
Acute cor pulmonale: a.
Is usually caused by an acute lung injury or disease b.
Is usually caused by acute systolic heart failure c.
Is best diagnosed by a left heart catheterization d.
Is never found in patients with chronic lung disease