Hypernatremic Dehydration
advertisement

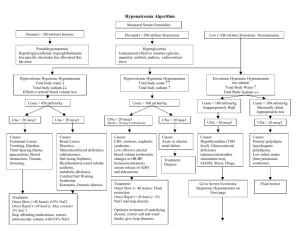
Hypernatremic Dehydration Mary Palomaki November 8, 2010 Definition • Serum sodium level greater than 145 mEq/L • Deficit of water • Causes: – pure water loss (diabetes insipidus) – Hypotonic fluid loss (vomit/diarrhea) – Hypertonic sodium gain (wrong formula preparation) Diabetes Insipidus • Central or Nephrogenic • Hypernatremia develops when patient does not have access to free water or is unable to drink sufficient water – Immaturity – Neurologic impairment – emesis Adipsia • Absence of thirst • Primary adipsia is rare • Secondary adipsia from damage to hypothalamus – Trauma – Tumor – Hydrocephalus – Histiocytosis Osmotic Diuresis • Glucose, mannitol, or urea • Water losses exceed sodium losses • Polyuric phase of acute tubular necrosis – Osmotic diuresis from high levels of urea – Tubular dysfunction causing inability to concentrate urine Breastfeeding Hypernatremia • • • • • Occurs in infants 1-3 weeks old First born children Poor mother-infant interaction Limited human milk production Sodium content in human milk remains high • 40 cases have been described: mean serum sodium was 181 mEq/L Clinical Manifestations • Children in initial phase of hypernatremic dehydration tend to show fewer physical exam findings of dehydration than those with isotonic or hypotonic – Intracellular water shifts to extracellular space – Child can then maintain intravascular volume • Maintain BP and urine output longer • • • • • Skin feels “doughy” Muscle weakness High-pitched cry Insomnia Lethargy Hypernatremia and the Brain • Water shifts from inside brain cells to extracellular space • Brain cells decrease in size • Total brain volume decreases • Intracerebral blood vessels can tear – Shearing forces – Bridging veins can rupture as brain pulled away from meninges/skull • • • • Hemorrhage Seizures Encephalopathy Paralysis Thrombotic Complications • • • • Stroke Dural sinus thrombosis Peripheral thrombosis Renal vein thrombosis Idiogenic Osmoles • If dehydration develops slowly, brain develops idiogenic osmoles • These intracellular osmoles help to preserve intracellular water content • Slow correction of hypernatremia is crucial – If extracellular fluid osmolarity is decreased too rapidly, water shifts intracellularly causing brain edema Treatment • Goal: decrease serum sodium by 12-15 mEq/L/24 hours (0.5-0.6 mEq/L/hr) • Frequent monitoring of serum sodium to ensure rate of correction is not too fast • First priority is restoration of intravascular volume Treatment: Emergency Phase • Restore intravascular volume – 10-20 mL/kg of isotonic IV fluid (LR or NS) – LR: 130 mEq/L sodium – NS: 154 mEq/L sodium • In severe dehydration (sodium greater than 175 mEq/L): – Don’t give NS or LR, as these fluids are hypotonic to patient – Make IV fluids with sodium concentration 10-15 mEq/L less than serum sodium (so fluid is isotonic to patient) Treatment: Rehydration Phase • Calculate maintenance IV fluids • Calculate amount of free water to be replaced over the next 24 hours • Assume 60-70% body weight is water (higher in infants vs. older children) • Free water deficit is: • (L) = 0.7 x wt (Kg) [1-current sodium/desired sodium] • In mild-moderate dehydration free water deficit will be replaced over 48h Treatment: Rehydration Phase • In mild-moderate dehydration (initial serum sodium < 175 mEq/L), • IV fluid of choice is: • D5 1/4 NS Treatment: Rehydration Phase • In severe dehydration (initial serum sodium is >175 mEq/L), • IV fluid of choice is similar to IV fluids in emergency phase • Make IV fluids with sodium content 10-15 mEq/L less than serum sodium • Mix 3% (513mEq/L) with D5NS • Frequent monitoring of serum sodium and adjustment of sodium in fluids What if…. • Correction occurs too rapidly? – Brain Edema – Administer 3% NS to quickly reverse edema • Patient has hypernatremia secondary to sodium administration – The change is usually rapid-no time for idiogenic osmoles to accumulate – Can correct rapidly • Peritoneal dialysis • Administration D5W (no sodium) and loop diuretics References • Androgue HJ, Madias NE. Hypernatremia. N Engl J Med 2000;342:1493-1499 • Nelson Textbook of Pediatrics. 18th ed. PP 273-275. • Schwaderer, A and Schwartz, G. Treating hypernatremic dehydration. Peds in Rev 2005;26:148-150