Acute Upper GI Bleed:

Acute Upper GI Bleed:
Case 1
64/C/M presented to the A&E with c/o
SOBOE, giddiness and lethargy.
He gives a history of passing out black tarry stools yesterday.
He has been taking diclofenac sodium regularly due to bilateral knee pains.
He has also drinking alcohol regularly, i.e. 2 large bottle of beers daily.
How important are the colour of his stools?
What are the possible causes of his GI bleed?
What other physical signs are helpful to determine the cause of GI bleed?
Physical examination
The patient was found to be drowsy, with
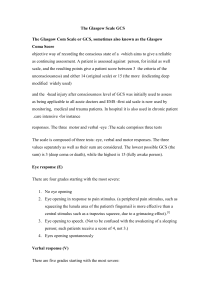
M5V3E3 (GCS 11/15)
BP was 95/70 mm Hg
HR 110 bpm
Peripheries was cold and clammy
Pulse was feeble
SpO2 95%
What is the causes of the low GCS?
What is the significance of the vital signs recorded?
You find that he has 8 spider naevis, absence of axillary hair and gross ascites.
He has a flapping tremor.
He also has multiple bruising over the extensor surfaces of his arms.
What could be the other cause of his low
GCS?
State the stages of hepatic encephalopathy.
Suddenly, he develops haemataemesis.
Do you insert a Ryle’s tube? State your reasons for doing so.
You check the vital signs again :
– BP 84/50 mm Hg
–
–
HR 150 bpm
GCS M3V2E1 (6/15)
– SpO2 89%
Why has the vital signs worsened?
Why has he become more hypoxic?
What do you do now?
List down your approach to stabilizing this patient.
Investigation results
TWC 13.5
Hb 6.0
MCV 80
MCH 30
Plt 500
Explain the results above.
Would you expect hypochromic microcytic anemia?
APTT 40
PT 15
INR 1.8
What are the possible causes?
What other tests to order to elucidate the cause?
Urea 28
Creat 140
Na 130
K 3.7
Explain the results above.
TP 60, alb 23
ALT 878
ALP 30
Explain the results.
RBS 3.0
Why?
What blood products do you want to give and why?
What is the target Hb in this patient?
List all the problems / diagnosis of this patient.
What is the definitive treatment of this patient?
Are there any drugs which helps reduce bleeding?
Are antibiotics needed in this patient?
What is the follow up care for this patient?
Case 2
60 year old man presents with 1 week history of malaena and shortness of breath?
On examination he his pale and cachexic.
Hb 9.0g/dL MCV 60 MCH28
PR showed malaena, examination of the abdomen was unremarkable.
BP 120/80 mm Hg
HR 99 bpm
What could be the possible causes of his
UGIB?
What investigations would you send?
Would you transfuse him with blood?
What are the indications for blood transfusion?
How fast would you transfuse the blood?
Do you need to give IV Frusemide as well?
OGDS showed a Forrest IIc ulcer.
What does this mean?
How can the ulcer be treated endoscopically?
What drugs should the patient be given?
Patient asks you what are the risks for
OGDS. What do you say?