Interventional Radiologists
advertisement

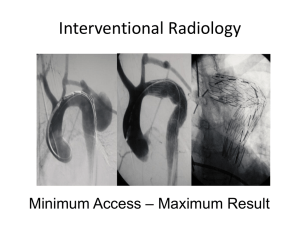
Interventional RadiologistsWhere will they go next? Dr Simon Travis MB ChB FRCR Vascular/Interventional Radiologist Nottingham University Hospitals What is an Interventional Radiologist? Global Statement Defining Interventional Radiology J Vasc Interv Radiol 2010; 21:1147–1149 1. Expertise in diagnostic imaging and radiation safety. 2. Expertise in image-guided minimally invasive procedures and techniques as applied to multiple diseases and organs. 3. Expertise in the evaluation and management of patients suitable for the image-guided interventions included in the scope of IR practice. 4. Continual invention and innovation of new techniques, devices, and procedures. History • 1964 Angioplasty • 1966 Embolization therapy to treat tumors and spinal cord vascular malformations by blocking the blood flow • 1967 The Judkins technique of coronary angiography, the technique still most widely used around the world today • 1967 Closure of the patent ductus arteriosis, a heart defect in newborns of a vascular opening between the pulmonary artery and the aorta • 1967 Selective vasoconstriction infusions for hemorrhage, now commonly used for bleeding ulcers, GI bleeding and arterial bleeding • 1969 The catheter-delivered stenting technique and prototype stent • 1960-74 Tools for interventions such as heparinized guidewires, contrast injector, disposable catheter needles and seethrough film changer • 1970’s Percutaneous removal of common bile duct stones • 1970’s Occlusive coils • 1972 Selective arterial embolization for GI bleeding, which was adapted to treat massive bleeding in other arteries in the body and to block blood supply to tumors • 1973 Embolization for pelvic trauma • 1974 Selective arterial thrombolysis for arterial occlusions, now used to treat blood clots, stroke, DVT, etc. • 1974 Transhepatic embolization for variceal bleeding • 1977-78 Embolization technique for pulmonary arteriovenous malformations and varicoceles • 1977-83 Bland- and chemo-embolization for treatment of hepatocellular cancer and disseminated liver metastases • 1980 Cryoablation to freeze liver tumors • 1980 Development of special tools and devices for biliary manipulation • 1980’s Biliary stents to allow bile to flow from the liver saving patients from biliary bypass surgery • 1981 Embolization technique for spleen trauma • 1982 TIPS (transjugular intrahepatic portosystemic shunt) to improve blood flow in damaged livers from conditions such as cirrhosis and hepatitis C • 1982 Dilators for interventional urology, percutaneous removal of kidney stones • 1983 The balloon-expandable stent (peripheral) used today • 1985 Self-expanding stents • 1990 Percutaneous extraction of gallbladder stones • 1990 Radiofrequency ablation (RFA) technique for liver tumors • 1990’s Treatment of bone and kidney tumors by embolization • 1990’s RFA for soft tissue tumors, i.e., bone, breast, kidney, lung and liver cancer • 1991 Abdominal aortic stent grafts • 1994 The balloon-expandable coronary stent used today • 1997 Intra-arterial delivery of tumor-killing viruses and gene therapy vectors to the liver • 1999 Percutaneous delivery of pancreatic islet cells to the liver for transplantation to treat diabetes • 1999 Developed the endovenous laser ablation procedure to treat varicose veins and venous disease Why Interventional Radiology • • • • • • Shorter Hospital Stays Money Saving Reduction in Transfusion Requirements Better QoL for patients Faster Recovery High Intensity Localised treatments What’s Our Role in Chronic Care? Vascular • Treatment of Ischaemic limbs • Diabetic foot ulcers • Management of Aneurysms of the Aorta and Visceral vessels • Vascular Access Management for Renal Replacement Therapy • Varicose Vein Ablation • Renal Artery Disease • AVM management Oncology • Vascular Access (ports and lines) • Image Guided Biopsy • Tumour Ablation – – – – RF Cryo Microwave Focused U/S • Tumour Embolisation with Chemotherapy • SVC Stenting for SVCO • Portal Vein Embolisation Prior to Hepatic Resection Gastrointestinal • Percutaneous Bile Duct Management • Colonic Stenting as a Bridge to Surgery (CREST trial) • Oesophageal Stenting • Gastrostomy Insertion • TIPSS for Ascites Control in Hepatic Cirrhosis Other Conditions • Uterine Fibroid Embolisation for Symptom Relief • Vertebroplasty for Pain Relief • Tunnelled Pleural and Ascitic Drains What’s Our Role in Acute Medical Care? • Control of Haemorrhage – Uterine Postpartum (Health Commission report on Northwick Park) – Acute Aneurysm Rupture – Acute Aortic Dissection – Post Traumatic Vascular and Visceral Injury – GI Haemorrhage • Acutely Ischaemic Limbs • DVT and PE management • Emergency Venous Access in Dialysis Patients What’s New? • Renal Artery Denervation for Difficult to Control Hypertension • Prostate Embolisation • Desolving Stents Renal Artery Denervation • Transarterial Catheter directed RF Ablation of Renal Sympathetic Nerves • Good results from proof of principal cohort study (45 patients with drug resistant hypertension) Prostate Embolisation for BPH • Injection of micro particles (100-200 micron) into the prostatic arteries to shrink the organ • Promising results in animal and human studies • Day case procedure with the potential for a return towards normal micturition with out medication (better QoL and cost saving) How Will We Affect Health Care in The Future • Save Money – Reduced Bed stays – Reduced Transfusion Requirements – More Rapid Patient Recovery – More Rapid Return to Normal Life/Work • Improve QoL for Patients • More Procedures by the month • Better Cancer Outcomes Interventional Radiology • Has been recognised as a distinct subspeciality by the Royal Colleges • We now have our own training program • We have our own syllabus • 3 years of Radiology Training followed by 3 years of Interventional Training Finally Train Patients to do Their Own Procedures?