Wheezing in Children
advertisement
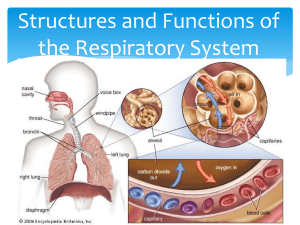
Wheezing in Children Mona Massoud, MD Emory University School of Medicine Family Medicine Residency 9/22/11 Introduction Common presenting symptom of respiratory disease in children Could benign and self limiting or presenting symptom of significant respiratory disease Common problems presented to PCP Incidence 25-30% of infants will have one episode of wheezing. By six years of age approximately half of children will have had at least one episode of wheezing Overview Wheezing: Continuous coarse whistling sound produced by oscillation of narrowed or compressed respiratory airway. Inspiratory or expiratory/ High or low pitched. Crackles (rales): Popping sound created when air is forced through respiratory passages. Stridor: high-pitched harsh sound heard during inspiration, due to obstruction of upper airway. Wheezing type in childhood Transient wheezer: One episode or few episodes of wheezing. No further episodes beyond 6 years. Non-atopic wheezer: Wheeze during viral infections and continue to have recurrent airway obstruction during early school years. IgE associated wheeze/asthma: Start to have symptoms later in life which continues into adulthood. Wheezing Type in Childhood Why do Children tend to wheeze more than Adults? Children have smaller airway passages, therefore higher resistance Less chest compliance Elastic tissue recoil is lower than adults and fewer collateral airways-prone to obstruction and atelectasis Differential Diagnosis Acute Asthma Bronchitis Bronchiolitis Laryngeotracheobronchitis (Croup) Bacterial Tracheitis FB aspiration Esophageal FB Chronic or Recurrent Causes Asthma GERD Retained foreign body Cystic Fibrosis Recurrent Aspiration Primary ciliary dyskinesia ILD Immunodeficiency Structural Causes: Tracheo-bronchomalacia Vascular rings Tracheal web Cystic lesions/lymphadenopathy/mediastinal masses Asthma Affects approximately 5 million children in US Chronic and reversible inflammatory disorder that produces airway hyper-responsiveness, airway inflammation and airflow limitation. Immediate and delayed inflammatory response Classification of Asthma Asthma Control assessment Bronchiolitis Children less than 2 yo, usually 3-6 m Viruses-RSV (most common), adenovirus, influenza or parainfluenza Fall and winter months Begins as mild URI which can progress to increase respiratory distress Rx: Supportive therapy Ribavirin in extremely ill children Croup vs Epiglottitis Approach to a wheezing child Clinical History: Wheeze description from parents Snoring, snoring, rattling or gargling noises Patient age at onset of wheeze Distinguishes congenital vs non-congenital Course: acute vs gradual Acute onset- FB aspiration Cont’d Q’s Pattern of wheezing? Episodic: asthma Persistent: congenital Response to bronchodilators? Improvement: Asthma Is Wheezing associated with multiple respiratory illnesses? Cystic fibrosis and Immunodeficiency diseases Cont’d Q’s Wheeze associated with feeding? GERD Wheeze associated with cough? GERD, asthma, allergies Change in position? Worsening or improvement Tracheomalacia Family hx of asthma? Features that favors diagnosis of Asthma Intermittent episodes of asthma Presence of a trigger URI Allergens Exercise Seasonal variation Family hx of asthma and/or atopy Response to bronchodilators Clinical features that suggest a diagnosis other than asthma: Hx of wheezing since birth or neonatal respiratory problems. Hx of choking associated with SOB and coughing. Symptoms that change with position. Poor weight gain and recurrent infections. Hx of progressive dyspnea, tachypnea, exercise intolerance. Poor response to broncholdilators. Physical Examination Vital signs including Sa02 % Inspection: Respiratory distress/ tachypnea/ cyanosis Retractions or structural abnormalities (increased AP diameter, pectus excavatum, scoliosis) HENT: allergic shiners/nasal polyps Skin: eczema Cont’d PE Palpation: chest wall asymmetry with expansion, tracheal deviation or supratracheal lymphadenopathy Percussion: difference in vocal resonance and define position of diaphragm Auscultation: Location of wheeze Character of wheeze Other breath sounds associated with wheeze Cardiac: presence of murmur or gallops Diagnostic Evaluation CXR: AP and lateral views Children with new onset wheezing of undetermined etiology Chronic persistent wheezing not responding to treatment Lateral decubitus views: FB aspiration Chest radiography is not performed with every asthma exacerbation unless there is a specific indication CXR findings: Hyperinflation: Generalized: suggests diffuse air trapping Asthma/ Cystic fibrosis/ Primary ciliary dyskinesia Localized hyperinflation: Structural abnormalities/ FB aspiration Other findings: atelectasis, bronchiectasis, mediastinal masses, enlarged LN’s, cardiomegaly, enlarged pulmonary vessels or pulmonary edema. Status Asthmaticus Croup (Steeple Sign): FB aspiration FB occludes middle lobe bronchus Atelectasis of Rt middle lobe Hyperinflation of upper and lower lobes Other radiological studies: Chest CT scan: Mediastinal masses or LN’s Vascular anomalies Bronchiectasis Barium Swallow: GERD TEF Vascular rings Swallowing dysfunction Vascular ring TEF Pulmonary Function Tests (PFT’s) Airway obstruction assessment PFT’s with inspiratory and expiratory flow- volume loops is is important in determining the degree, location of airway obstruction in addition to response to bronchodilators. Response to Treatment Trial of inhaled bronchodilators Improvement: reversible airway disease Partial or negative response: asthma or other causes Combination of inhaled CST +bronchodilators: if asthma is suspected in a patient with chronic or persistent symptoms Bronchodilator response Other Investigations Sweat Chloride Test: Cystic fibrosis screening in children with chronic lung problems, failure to thrive and diarrhea Immunoglobulin levels: Screen for immunodeficiencies. Rapid antigen testing, viral cultures, sputum gram stain and culture. PPD in suspected cases. http://www.youtube.com/watch?v=VA9C_aC H7F0 http://www.youtube.com/watch?v=EMKxnyPs 7K8&feature=related http://www.youtube.com/watch?v=Qbn1Zw5C TbA&feature=related References http://www.aafp.org http://www.uptodate.com/contents http://emedicine.medscape.com http://www.essentialevidenceplus.com http://www.acaai.org/patients/resources/asthma/Docu ments/AZnhlbiGuidelines http://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0001 970/ http://www.medcyclopaedia.com/library/radiology http://pediatrics.aappublications.org/content/123/3/e5 19.long