Aeromedical Evacuation
advertisement
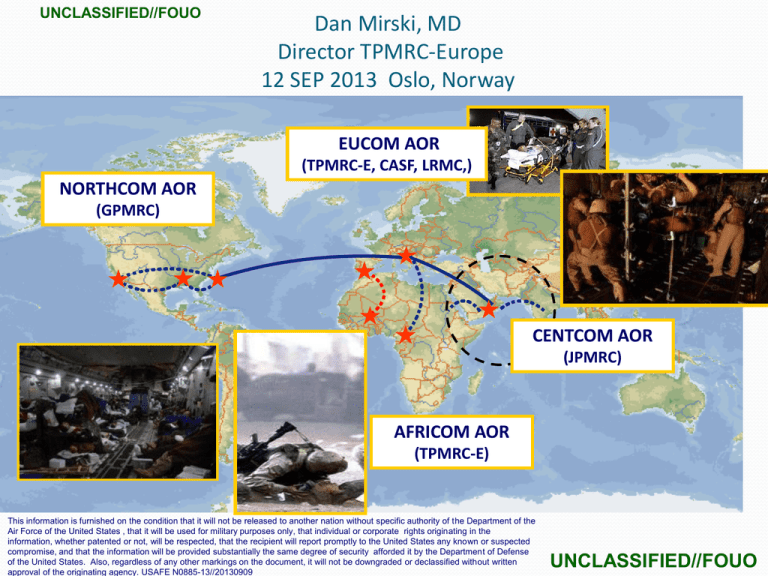
UNCLASSIFIED//FOUO Dan Mirski, MD Director TPMRC-Europe 12 SEP 2013 Oslo, Norway EUCOM AOR (TPMRC-E, CASF, LRMC,) NORTHCOM AOR (GPMRC) CENTCOM AOR (JPMRC) AFRICOM AOR (TPMRC-E) This information is furnished on the condition that it will not be released to another nation without specific authority of the Department of the Air Force of the United States , that it will be used for military purposes only, that individual or corporate rights originating in the information, whether patented or not, will be respected, that the recipient will report promptly to the United States any known or suspected compromise, and that the information will be provided substantially the same degree of security afforded it by the Department of Defense of the United States. Also, regardless of any other markings on the document, it will not be downgraded or declassified without written approval of the originating agency. USAFE N0885-13//20130909 UNCLASSIFIED//FOUO UNCLASSIFIED//FOUO Outline USAF Flight Surgeon Overview of US System Aeromedical Evacuation (AE) Patient Tracking: TRAC2ES Medical Lessons Learned UNCLASSIFIED//FOUO UNCLASSIFIED//FOUO Dan Mirski, MD, MPH Emergency Medicine Aerospace Medicine LtCol, US Air Force, Chief Flight Surgeon Director, TPMRC-Europe UNCLASSIFIED//FOUO Enroute Care UNCLASSIFIED//FOUO Level of Care GOAL: Maintain Equal Or Greater Level Of Care During Intra/Inter-Theater Air Evacuation CSH, EMEDS, EMF Forward Surgical teams BAS Wounded Self Aid & Buddy Care First Responder Definitive Care Theater Hospitals Forward Resuscitative Continuous Increase in Level of Care Provided Time UNCLASSIFIED//FOUO UNCLASSIFIED//FOUO Aeromedical Evacuation (AE) Overview CASEVAC, MEDEVAC, Aeromedical Evacuation (AE) Role 1-4: Installation Capabilities 3 = Life-saving med/surg/psych care) Urgent, Priority(24h), Routine (72h) AE crew = 2 RNs, 3 techs CCAT = 1 MD, 1 RN, 1 RT C17, C21, KC135, C130 “Stressors of Flight” Patient Categories 1-5 EMR: TRAC2ES UNCLASSIFIED//FOUO UNCLASSIFIED//FOUO PM Route Current Route from Point of Injury to Definitive Capability CASEVAC or MEDEVAC MEDEVAC or INTRATHEATER AE First Responder Role 1 INTERTHEATER AE Forward Resuscitative Capability Role 2 Theater Hospitalization Capability (CSH, EMEDS, EMF) Role 3 SURGICAL CAPABILITY PUSHED FAR FORWARD UNCLASSIFIED//FOUO Definitive Capability Role 4 UNCLASSIFIED//FOUO 10/2001 – 8/12/13 BI= 14,875 NBI= 46,346 BI NBI 1600 1400 1200 1000 800 600 400 200 UNCLASSIFIED//FOUO Oct-12 Oct-11 Oct-10 Oct-09 Oct-08 Oct-07 Oct-06 Oct-05 Oct-04 Oct-03 Oct-02 Oct-01 0 UNCLASSIFIED//FOUO DoD Patient Movement System UNCLASSIFIED//FOUO UNCLASSIFIED//FOUO 2 TRAC ES TRANSCOM Regulating Command/Control Evacuation System UNCLASSIFIED//FOUO UNCLASSIFIED//FOUO DoD Patient Movement System TRANSCOM RegulatingTRAC2ES Command/Control Evacuation System (TRAC2ES) Web-based/Consolidated Server Automates Patient Regulating Network for In-Transit Visibility of patient movement Patient Movement Requirements Center Originating Hospital UNCLASSIFIED//FOUO Patient Movement Requirements Center Destination Hospital UNCLASSIFIED//FOUO DoD Patient Movement System Military Medical Treatment Facilities (MTF)s Submit Patient Movement Requests (PMRs) Coordinate arrival/departure of patients Patient Movement Requirements Center CENTCOM: Joint PMRC, Al Udeid, Qatar NORTH/SOUTHCOM: Global PMRC, Scott AFB, Illinois PACOM: Theater PMRC, Hickam AFB, Hawaii EUCOM: Theater PMRC, Ramstein AB, Germany UNCLASSIFIED//FOUO UNCLASSIFIED//FOUO PMRC Areas of Responsibility USNORTHCOM Validate/Coordinate/Communicate patient movement to/from/within geographic Area of Responsibility UNCLASSIFIED//FOUO UNCLASSIFIED//FOUO DoD Patient Movement System Air Mobility Division (AMD), AE Control Team (AECT) Interface with airlifters for AE movement USAFE for intra-theater movement Tanker Airlift Control Center (TACC) for inter-theater lift Aeromedical Evacuation Squadrons Provide in-flight medical or specialty care 2 flight nurses, 3 medical technicians UNCLASSIFIED//FOUO UNCLASSIFIED//FOUO TRAC2ES Patient Movement Request (PMR) Referring MTF/Hospital: Submit Patient Movement Request (PMR) Reception MTF: Patient arrives at destination facility UNCLASSIFIED//FOUO PMRC: Validate PMR, Coordinate airlift, Communicate mission itinerary AECT/TACC: Task airlift/aircrews AE Crews: Execute mission UNCLASSIFIED//FOUO TRAC2ES Patient Movement Request (PMR) Clinical Data Medical Specialty/Diagnosis Patient History/Medications/Labs Patient Demographics Patient Name/Nationality/ID# Rank/Age/Gender Precedence (URGENT, PRIORITY, ROUTINE) UNCLASSIFIED//FOUO UNCLASSIFIED//FOUO TRAC2ES Mission Planning/Execution Referring MTF/Hospital: Submit Patient Movement Request (PMR) Reception MTF: Patient arrives at destination facility UNCLASSIFIED//FOUO PMRC: Validate PMR, Coordinate airlift, Communicate mission itinerary AECT/TACC: Task airlift/aircrews AE Crews: Execute mission UNCLASSIFIED//FOUO TRAC2ES Mission Planning/Execution AE Control Team/ Tanker Airlift Control Center Identify aircraft Task AE crew members Task specialty support Notify PMRC when mission information is complete UNCLASSIFIED//FOUO UNCLASSIFIED//FOUO TRAC2ES Mission Planning/Execution Referring MTF: Submit Patient Movement Request (PMR) Reception MTF: Patient arrives at destination facility UNCLASSIFIED//FOUO PMRC: Validate PMR, Coordinate airlift, Communicate mission itinerary AECT/TACC: Task airlift/aircrews AE Crews: Execute mission UNCLASSIFIED//FOUO TRAC2ES 24-Hour Report Referring MTF: Submit Patient Movement Request (PMR) Reception MTF: Patient arrives at destination facility UNCLASSIFIED//FOUO PMRC: Validate PMR, Coordinate airlift, Communicate mission itinerary AECT/TACC: Task airlift/aircrews AE Crews: Execute mission UNCLASSIFIED//FOUO TRAC2ES 24-hr Report UNCLASSIFIED//FOUO Destination Medical Treatment Facilities Visibility for in-bound… Missions Itineraries Patient loads Plan patient reception/care UNCLASSIFIED//FOUO Global Patient Movement A Team Effort USNORTHCOM UNCLASSIFIED//FOUO UNCLASSIFIED//FOUO From the last 10 years of Patient Movement UNCLASSIFIED//FOUO UNCLASSIFIED//FOUO Medical Advancements & Lessons Learned 1. 2. 3. 4. 5. 6. 7. 8. 9. Resuscitation with blood products LIFO Blood Usage Damage Control Surgery Burn Management Ventilatory Control with Decreased Tidal Volume Massive Blood Transfusion Triggers Epidurals & Nerve Blocks Tourniquets No Steroids in Blunt Spinal / Head Trauma UNCLASSIFIED//FOUO UNCLASSIFIED//FOUO Blood Component Therapy Prior typical "resuscitation protocol" = lots of LR or NS then 1-2 units of blood (3:1) This practice contributed to the lethal triad of coagulopathy, hypothermia & acidosis Now, high suspicion patient is bleeding = proceed directly to blood products. Repine TB, Perkins JG, Kauvar DS, Blackborne L. The use of fresh whole blood in massive transfusion. J Trauma. 2006;60:S59-S69. 2. Spinella PC, Perkins JG, Grathwohl JG, Beekley AC, Holcomb JG. Warm fresh whole blood is independently associated with improved survival for patients with combat-related traumatic injuries. J Trauma. 2009;66:S69S76. 1. UNCLASSIFIED//FOUO UNCLASSIFIED//FOUO Blood Tx: LIFO New blood over old blood Previously, the oldest blood in the theater was given first for transfusions should be used before it goes bad. Fresh blood has been shown to be superior complications of transfusion with "older" units of PRBCs "storage lesion": increase pro-inflammatory factors, acidosis, increased free hemoglobin, and decreased RBC deformability, 2,3 DPG & ATP The people most likely to suffer the consequences of complications of "older" units of blood are those requiring a higher dose In patients requiring massive transfusion , effort made to transfuse fresh units of PRBCs Preferably < 14 days old, but the freshest available nonetheless Now, LAST IN, FIRST OUT (LIFO) Blood Policy Donation to availability in theater averaging 7 days 1. Spinella PC, Perkins JG, et al. Warm fresh whole blood is independently associated with improved survival for patients with combat-related traumatic injuries. J Trauma. 2009;66:S69-76. UNCLASSIFIED//FOUO UNCLASSIFIED//FOUO Damage Control Surgery We now transport patients with “unfinished surgeries” - open abdomens bleeding stopped via clamping and/or packing. They are moved to higher levels for more definitive care Further damage control surgeries done “Final” closure surgery Eastridge BJ, Mabry RL, Seguin P, Cantrell J, Tops T, Uribe P, Mallett O, Zubko T, Oetjen-Gerdes L, Rasmussen T, Butler FK, Kotwal RS, Holcomb JB, Wade C, Champion H, Lawnick M, Moores L and Blackbourne LH. Death on the battlefield (2001-2011): Implications for the future of combat casualty care. J Trauma. 2012;73:S431-S437, UNCLASSIFIED//FOUO UNCLASSIFIED//FOUO Burn Management Rule of 10's and 6 ml/kg/%BSA burned in thermal injury burn management Basically, now we don’t pour in the fluid. Start with an initial amount Then adjust it up or down up to 25% per hour (not more!) Result = far less incidents of abdominal compartment syndrome CCATT transported patients with burns up to 98% and they have survived. 1. Ennis JL, Chung KK, Renz EM, Barillo DJ, Albrecht MC, Jones JA, Blackbourne LH, Cancio LC, Eastridge BJ, Flaherty SF, Dorlac WC, Kelleher KS, Wade CE, Wolf SE, Jenkins DH, Holcomb JB. Joint Theater Trauma System implementation of burn resuscitation guidelines improves outcomes in severely burned military casualties. J Trauma. 2008;64(2):S146-51; discussion 151-2. 2. Markell KW, Renz EM, White CE, Albrecht ME, Blackbourne LH, Park MS, Barillo DA, Chung KK, Kozar RA, Minei JP, Cohn SM, Herndon DN, Cancio LC, Holcomb JB,Wolf SE. Abdominal complications after severe burns. J Am Coll Surg. 2009;208(5):940-7; discussion 947-9. UNCLASSIFIED//FOUO UNCLASSIFIED//FOUO Vents: Decreased TV Lung protective strategies in ARDS / ICU / Difficult to Ventilate pts Tidal Volume: 4-6 cc/Kg Not 10-12 cc/Kg, as prior Ideal BW Increase PEEP and/or FiO2 Essentially ARDSNet Used very often by US CCATT UNCLASSIFIED//FOUO UNCLASSIFIED//FOUO Other Advances 7. Massive transfusion triggers Higher quantities of blood up front McLaughlin DF, Niles SE, Salinas J, et al. A predictive model for massive transfusion in combat casualty patients. J Trauma.2008;64:S57-63. 6. PCA, Epidural and nerve blocks We fly these all the time now Waiver x 10yrs, Official since 2012 Mepivacaine 250 vs 400ml IV bags Katz J, Cohen L, Schmid R, et al. Postoperative Morphine Use and hyperalgesia are Reduced by Preoperative but not Intraoperative Epidural Anagesia: Implications for Preemptive Analgesia and the Prevention of Central Sensitization. Anesthesiology. 2003;98:1449-1460. UNCLASSIFIED//FOUO UNCLASSIFIED//FOUO Lessons Learned (con’t) 8. Re-emergence of tourniquets 9. No steroids in blunt spinal cord or TBI No proven benefit Worsen outcomes in patients with severe head injury Frequent associated open or contaminated wounds of battle casualties further complicate steroid administration UNCLASSIFIED//FOUO Questions Mirski@hotmail.com UNCLASSIFIED//FOUO “VALIDATE…COORDINATE…COMMUNICATE” UNCLASSIFIED//FOUO