Anatomy of the Female Pelvis
Gareth Davies
Pelvis
Male vs Female
Male = Deep Greater Pelvis, Narrow pelvic inlet, small pelvic outlet, Narrow
Subpubic angle (<70 degrees)
Female = Shallow Greater Pelvis, Wide pelvic inlet, large pelvic outlet, wide
Subpubic angle (>80 degrees)
Pelvic Inlet
(a) Gynaecoid—normal.
(b) Symmetrically contracted pelvis
small woman with symmetrical shape.
(c) Android — masculine pelvis.
(d) Platypelloid — shortened in the
anteroposterior diameter, increased in
the transverse diameter (the ‘nonrachitic flat pelvis’).
(e)The Rachitic flat pelvis - rickets
(f) Anthropoid— lengthened
anteroposterior and a shortened
transverse diameter.
(g) Asymmetrical - scoliosis,
longstanding hip disease (e.g.
congenital dislocation), poliomyelitis,
pelvic fracture, Naegele pelvis
Joints
• Sacroiliac
– Anterior –> Synovial
– Posterior --> Syndesmosis
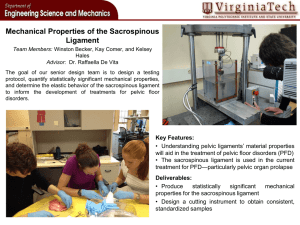
Ligaments
• Anterior, Interosseous, Posterior
Sacroiliac ligaments
• Pubic Symphysis
– Secondary Cartilaginous joint
Sacrospinous, Sacrotuberous
ligaments
Urogenital and Anal Triangles
Urogenital Triangle
Anal Triangle
Ischio-anal
fossae
Infection passes easily from one side to
the other
Can be due to boils or abrasions of the
perianal skin, from lesions within the
rectum and anal canal, from pelvic
infection
bursting through levator ani or, rarely, via
the bloodstream.
External
Genitalia
Deep Perineal Pouch
Injury to Pelvic
Floor During
Childbirth
• Can cause tearing of pubococcygeus
• Pubococcygeus encircles and
supports – urethra, vagina, anal
canal.
• Alteration of position of neck of
bladder and urethra – may lead to
urinary stress incontinence
• Episiotomy
Female Urethra
• Approx 4cm long
• Musculature surrounding the internal urethral
orifice is not organised into an internal
sphincter
• More easily distensible than male urethra
(increased elastic tissue) means catheters are
more easily placed.
• Paraurethral glands (homologue of the
prostate)
Pelvic Viscera
Ligaments
Infection – Peritonitis
Salpingitis
Round Ligament of uterus
Ovarian Ligament
Suspensory Ligament of Ovary
Broad Ligament
- Mesometrium
- Mesovarium
- Mesosalpinx
Transverse cervical (Mackenrodt) ligament provides main passive
support to uterus
Dynamic support provided by perineal muscles
Together help to prevent prolapse
The most important single practical relationship in this region is that of the ureter to the
supravaginal cervix. At this point, the ureter lies just above the level of the lateral fornix,
below the uterine vessels as these pass across within the broad ligament. In performing a
hysterectomy, the ureter may be accidentally divided in clamping the uterine vessels,
especially when the pelvic anatomy has been distorted by a previous operation, a mass of
fibroids, infection or malignant infiltration.
the ureter lies 12 mm lateral to the supravaginal cervix.
When can ureteric calculi be palpated?
Blood supply to the ureter
In abdomen – From Medial side
In Pelvis – From lateral Side
Innervation of the Perineum
Innervation of the
perineum:
Pudendal nerve
Innervation of the anterior
part of the mons pubis
provided by ilioinguinal
and genitofemoral nerves
from the lumbar plexus –
anterior labial nerves
Pelvic Pain Line
• the pelvic pain line corresponds to the inferior
limit of the peritoneum (in the GIT it occurs
midway along the sigmoid colon)
• Superior structures travel via sympathetic
afferents
• Inferior travels via parasympathetic