Chapter 37 Management of Patients With Gastric and Duodenal
advertisement
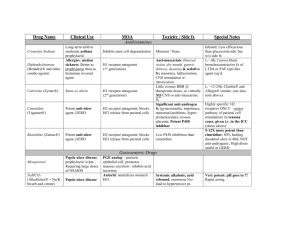
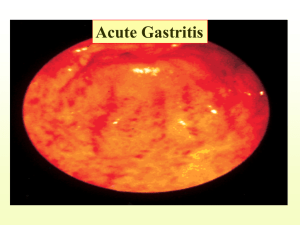
Management of Patients With Gastric and Duodenal Disorders Gastritis • Inflammation of the stomach • A common GI problem • Acute: rapid onset of symptoms usually caused by dietary indiscretion. Other causes include medications, alcohol, bile reflux, and radiation therapy. Ingestion of strong acid or alkali may cause serious complications. • Chronic: prolonged inflammation due to benign or malignant ulcers of the stomach or by Helicobacter pylori. May also be associated with some autoimmune diseases, dietary factors, medications, alcohol, smoking, or chronic reflux of pancreatic secretions or bile. Erosive Gastritis Manifestations of Gastritis • Acute: abdominal discomfort, headache, lassitude, nausea, vomiting, hiccuping. • Chronic: epigastric discomfort, anorexia, heartburn after eating, belching, sour taste in the mouth, nausea and vomiting, intolerance of some foods. May have vitamin deficiency due to malabsorption of B12. • May be associated with achlorhydria, hypochlorhydria, or hyperchloryhydria. • Diagnosis is usually by UGI X-ray or endoscopy and biopsy. Medical Management of Gastritis • Acute – Refrain form alcohol and food until symptoms subside – If due to strong acid or alkali treatment to neutralize the agent, avoid emetics and lavage due to danger of perforation and damage to esophagus – Supportive therapy • Chronic – Modify diet, promote rest, reduce stress, avoid alcohol and NSAIDs – Pharmacologic therapy (See Table 37-1) Peptic Ulcer • Erosion of a mucous membrane forms an excavation in the stomach, pylorus, duodenum, or esophagus • Associated with infection of H. pylori • Risk factors include excessive secretion of stomach acid, dietary factors, chronic use of NSAIDs, alcohol, smoking, and familial tendency. • Manifestations include a dull gnawing pain or burning in the mid-epigastrium; heartburn and vomiting may occur • Treatment includes medications, lifestyle changes, and occasionally surgery (See Tables 37-1 and 37-3) Deep Peptic Ulcer Surgical Procedures for Peptic Ulcers Nursing Process: The Care of the Patient with Gastritis—Assessment • History including presenting signs and symptoms • Dietary history and dietary associations with symptoms • 72 hour diet; diary may be helpful • Abdominal assessment Nursing Process: The Care of the Patient with Gastritis—Diagnoses • • • • • Anxiety Imbalanced nutrition Risk for fluid volume imbalance Deficient knowledge Acute pain Nursing Process: The Care of the Patient with Gastritis—Planning • Major goals may include reduced anxiety, avoidance of irritating foods, adequate intake of nutrients, maintenance of fluid balance, increased awareness of dietary management, and relief of pain. Interventions • Reduce anxiety; use calm approach and explain all procedures and treatments. • Promote optimal nutrition; for acute gastritis, the patient should take no food or fluids by mouth. Introduce clear liquids and solid foods as prescribed. Evaluate and report symptoms. Discourage caffeinated beverages, alcohol, cigarette smoking. Refer for alcohol counseling and smoking cessation. • Promote fluid balance; monitor I&O, for signs of dehydration, electrolyte imbalance, and hemorrhage. • Measures to relieve pain: diet and medications. • See Chart 37-1. Nursing Process: The Care of the Patient with Peptic Ulcer—Assessment • Assess pain and methods used to relieve pain • Dietary intake and 72 hour diet diary • Lifestyle and habits such as cigarette and alcohol use • Medications; include use of NSAIDs • Sign and symptoms of anemia or bleeding • Abdominal assessment Nursing Process: The Care of the Patient with Peptic Ulcer—Diagnoses • • • • Acute pain Anxiety Imbalanced nutrition Deficient knowledge Collaborative Problems/Potential Complications • • • • Hemorrhage Perforation Penetration Pyloric obstruction (gastric outlet obstruction) Nursing Process: The Care of the Patient with Peptic Ulcer—Planning • Major goals for the patient may include relief of pain, reduced anxiety, maintenance of nutritional requirements, knowledge about the management and prevention of ulcer recurrence, and absence of complications. Anxiety • • • • • Assess anxiety Calm manner Explain all procedures and treatments Help identify stressors Explain various coping and relaxation methods such as biofeedback, hypnosis, and behavior modification Patient Teaching • • • • Medication teaching Dietary restrictions Lifestyle changes See Chart 37-2 Management of Potential Complications • Management of hemorrhage – Assess for evidence of bleeding, hematemesis or melena, and symptoms of shock/impending shock and anemia. – Treatment includes IV fluids, NG, and saline or water lavage; oxygen, treatment of potential shock including monitoring of VS and UO; may require endoscopic coagulation or surgical intervention. • Pyloric obstruction – Symptoms include nausea and vomiting, constipation, epigastric fullness, anorexia, and (later) weight loss. – Insert NG tube to decompress the stomach, provide IV fluids and electrolytes. Balloon dilation or surgery may be required. Management of Potential Complications • Management of perforation or penetration – Signs include severe upper abdominal pain that may be referred to the shoulder, vomiting and collapse, tender board-like abdomen, and symptoms of shock/impending shock. – Patient requires immediate surgery.