PN 124 Day 5, Venous and Pressure ulcers

Integumentary System, PN 124
Causes
- chronic deep vein insufficiency
- delay of venous blood returning to the central circulation
-severe varicose veins, burns, trauma, sickle cell anemia, diabetes, neurogenic disorders and heredity
-Dry/rough looking skin
-Hard to the touch
-Loss of body hair
-Ulcers begin as small, tender, inflamed
-Edema around the ulcer
-Occasional purulent drainage
-Slow to heal
Subjective Data
-Severity of ulcer pain
-worse with the leg dependent
-itching
-duration
-measures to treat the ulcer
Objective Data-
-Size
-location
-appearance
-Color
-both in a dependent and elevated position
-Wound drainage
-color and consistency
-edema
-Surrounding skin appearance
-erythema, induration
Limb elevation
-encourages return of venous blood to the general circulation
-increases arterial blood flow
-to general circulation and lower extremities
-decreased edema.
Compression dressings
-Unna Boot
Infection Control
-aseptic technique with dressing changes
-monitor for signs of infection
-cellulitis
Antibiotics-
-topical (Silvadine cream)
-oral or IV
Debridement
-Removal of necrotic tissue
- Mechanical
-wet to dry dressings
-Chemical
- Enzyme (Santyl, Elase)
-Surgical
-used only if mechanical and chemical means were ineffective
-removal via scalpel of necrotic tissue
Dressings
-Compression
-Unna boot, Ace bandages, TED socks
Pain Management
-Elevate legs, analgesics, topical anesthetics
Nutrition
-Protein, Vitamin A, Vitamin c, Zinc
(Bedsores/decubitus ulcers)
Causes
-Pressure on the skin
-collapse of capillaries
-ischemia/redness-1 hour
-tissue necrosis-after 2 hours
-boney prominences
-
Shearing
-Force exerted against the skin
-movement or repositioning
-Stretches and tears the blood vessels,
-reducing blood flow
-necrosis develops
Friction
_the force of 2 surfaces moving across on
another
_the rubbing of skin against the sheets
_removes superficial skin
_increases the risk of skin breakdown
Moisture
- incontinence urine and feces
-wound drainage
-perspiration
Stage I
- Non-blanchable erythema of intact skin
Stage II Pressure ulcer
-Partial thickness skin loss
-epidermis, dermis or both.
-Ulcer is superficial
-abrasion, blister or shallow crater
Stage III Ulcer
-Full thickness skin loss
-damage or necrosis to the subcutaneous tissue.
-May extend down to, but not through the underlying fascia.
-Deep crater with/without undermining of the adjacent tissue.
Stage IV Ulcer
-Full thickness skin loss
-extensive bone destruction, tissue necrosis, or damage to muscle, bone, or supporting structures
-Undermining and sinus tracts
Surrounding skin
-intact edges
-erosion
-maceration
-erythema
-edema
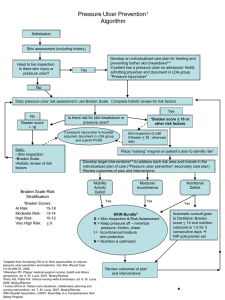
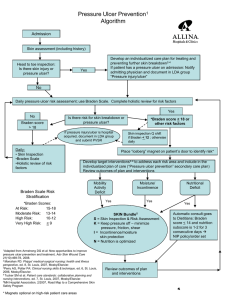
Braden Assessment Tool
Norton Pressure Ulcer Scale
Norton Assessment Tool
Risk factors for pressure ulcers
1. Impaired mobility
-bedbound
-wheelchair bound
-dependent on positioning
2. Moisture
-incontinent of urine and/or feces,
-perspiration
-wound drainage
3. Nutritionally compromised
-underweight
-obese
-poor nutritional status
-poor food/fluid intake
-secondary to poor appetite
-dysphasia
-limited ability to feed themselves.
4. Disease Process
-diabetes
-anemia
-atherosclerosis,
-edema
5. Vitamin and Mineral Deficiencies
-vitamin A, C, E, Zinc
Identify the at-risk patient
-elderly
-impaired mobility
-poor nutritional status
-altered level of consciousness
Pressure relieve
-written repositioning/ turning schedule
-30 degree position when side lying
-pillows and foam wedges
-turn sheet to reposition or lift patient in the bed
-encourage patients in wheelchairs to shift their weight every 15 minutes
Cleansing of the skin
-inspect the skin daily
-mild cleanser for bathing
-avoid massaging skin over a boney prominence
-moisturizer on the skin
-protective barrier ointment for incontinent patients
-clean the skin at the time of incontinence.
Pressure relieving mattress and cushions
-Egg carton mattress
-Geomatt mattress
-foam overlay mattress
-comparatively inexpensive
-Air overlay mattress
-placed over the hospital bed mattress
-weight redistribution
-Clinitron Bed
-mattress filled with small glass sand particles,
-moisture flows through the mattress
KCI/Kin Air Bed
-mattress of air-inflated pillows divided into sections
-pressure can be adjusted in each of the sections according to the client’s needs
-air flow form the mattress to eliminate moisture.
PREVENTION!!!
-most important aspect to be taught to client’s and their caregivers!!
1. Turning, positioning and shifting
-every 2-3 hours- even during the night.
2. Observe skin daily
3. Diet adequate in protein, vitamins, calories and good fluid intake.
4. Notify the health care provider for any changes in the skin.
-After a pressure ulcer has appeared
-Reinforce aggressive turning, positioning and pressure relief.
-Home Health RN
-assess the wound
-instruct the client and/or caregiver
-wound care
-signs of healing vs. deterioration
-homebound clients