Demystifying the Fellowship Examination
advertisement
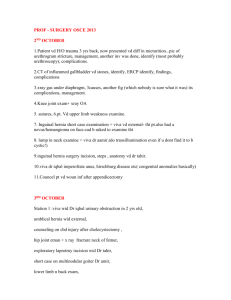
Demystifying the Fellowship Examination Tom Wilson Senior Examiner – General Surgery GSA Trainees’ Dinner 2013 Structure of the Examination • The exams are held twice a year with the Writtens a month before the Vivas in May and September. • May exams are in Wellington & Melbourne (odd years) and Auckland & Brisbane (even years). • September exams are in Adelaide (odd years) and Sydney (even years). Structure of the Examination • The Pathophysiology Critical Care and Clinical Reasoning Viva and the Operative Viva are usually on a Friday. • The 2 Clinical Vivas are on the Saturday. • The Anatomy Viva is usually on the Sunday. The Content of the Exams • Details of the Curriculum are available on the GSA web site www.generalsurgeons.com.au/e ducation-andtraining/curriculum The 7 exam segments 1. Written 1 – 25 spot questions 2. Written 2 – 8 short answer questions 3. Pathophysiology, Critical care and Clinical reasoning (PCC) viva – 2 scenarios, 4 mini-scenarios 4. Operative viva – 1 scenario, 5 mini-scenarios 5. Clinical 1 viva – 2 long cases 6. Clinical 2 viva – 6 short cases 7. Anatomy viva – 5 images, 5 Wet specimens Written 1 - Spots • 25 questions in 2 hours • Typically a clinical photo or image with 2-4 short questions about diagnosis, investigation & management • < 5 mins per question • Note form or dot point answers are appropriate • Clarity, precision and legibility are important Written 1 example A 58-year-old woman presents with fever, abdominal pain and jaundice. This is the image from her ERCP. 1. Describe the findings. 2. What is the diagnosis and outline your management of this problem? 3. What are the specific complications of ERCP? Written 2 – short answers • 8 questions in 2 hours • Greater detail expected. Usually 1 anatomy question • 15 mins per question • Either written, note form or dot point answers are appropriate • Clarity, precision and legibility are important Written 2 example A 65 year old man presents with 4 months of progressive dysphagia and recent weight loss. The provisional diagnosis is oesophageal cancer. • Outline the key points in establishing the diagnosis (including clinical features and investigations), staging and treatment options for this man. Pathophysiology, Critical Care & Clinical Reasoning (PCC) • 40 minute viva • 2 x 10 minute scenarios – 1 acute care (trauma, sepsis etc) – 1 complex clinical reasoning • 4 x 5 minute “mini-scenarios” • Example ……. This abnormality was seen in the stomach in a patient who being investigated for chronic anaemia. • What is the likely pathology? • What are the important features to document on endoscopy? • How would you investigate this further? • What management would you recommend? Operative • • • • 30 minute viva 1 x 10 minute scenario 5 x 4 minute “mini-scenarios” Example ……. This patient presented with acute large bowel obstruction. This is a limited rectal contrast study. • What is the diagnosis? • If you are unable to decompress this at sigmoidoscopy, describe the principles of your surgical approach. Clinical 1 – long cases • 40 minute viva • 2 long clinical cases – 20 minutes each • About 10 minutes for history, examination & presentation • 10 minutes for case discussion – discuss investigations & imaging, management What to expect? • These are likely to be chronic illness type patients • They can be complex problems • Be polite, respectful and professional • Treat the encounter as a patient consultation Clinical 2 – short cases • 40 minute viva • 6 short clinical cases (i.e., 6-7 minutes each) • This exam particularly assesses clinical interaction and elicitation of clinical signs What to expect? • These patients will usually have common clinical signs • The range of problems is predictable – hernias, abdominal signs, skin lesions, head/neck masses, breast lumps, vascular signs • It is important to show skilled and practiced examination technique • Be polite, respectful and professional Anatomy • • • • 25 minute viva 5 anatomy images 5 regions of anatomy on Wet specimens The range of anatomy is “General Surgery” – head & neck, axilla/breast, GI tract, diaphragm, abdominal cavity & contents, pelvis, inguinoscrotal & femoral regions, etc • Example ……. Use to scroll through images First image Last image The marking system • Each of the 7 exam segments are equally weighted • The segments are marked according to the “Close Marking System” – – – – 9.5 = excellent pass 9 = pass 8.5 = borderline fail 8 = fail • If you pass all exam segments you will pass the exam • If you fail 1 or 2 exam segments, you can still pass the exam if your performance overall is considered satisfactory! • If you fail > 2 exam segments, you are unlikely to pass The “Expanded Close Marking System” • Each of the 7 exam segments has defined “Marking Points” that the examiners use to score the candidate’s performance • Each of the “Marking Points” in each segment are scored according to the “Close Marking System” (i.e., 9.5, 9, 8.5, 8) • Each candidate is examined by a pair of examiners in each segment • Although the examiners score their “Marking Points” independently, they must reach a “Consensus grade” for the candidate in each exam segment The “Expanded Close Marking System” Segment Written 1 Written 2 PCC Operative Clinical 1 Clinical 2 Anatomy Content 25 questions 8 questions Scenario x 2 Mini-scenario x 4 Scenario Mini-scenario x 5 2 x long cases 6 x short cases 5 images 5 Wets Ex 1 25 8 2x3 4 3 5 2x4 6x2 5 5 Ex 2 25 8 2x3 4 3 5 2x4 6x2 5 5 TOTAL MPs 50 16 20 16 16 24 20 The marking system • At the completion of the exams, the Specialty Court meets to consider all the results – Candidates whose total score is ≥ 63 (7 x 9) will pass – Candidates whose total score is ≤ 61.5 will fail – Candidates whose total score is between 61.5 and 63 are discussed in detail and may still pass An example of information assessed by the Specialty Court The results • Candidates who pass do not receive feedback about details of how well they performed (or how close they may have been to failing!) • Candidates who fail do receive feedback about which segments of the exam they failed, but do not receive detail about specific questions or topics that were not satisfactory • The feedback is usually of a more general nature referring to “lack of knowledge”, “inappropriate management choices”, “poor examination technique” etc Coping with the examination • The Fellowship examination is a tough test • It is expensive and stressful • Make sure you come to it well prepared, both mentally & physically. Preparing for the exam • Study with your colleagues • Practice written questions • Treat the face-to-face vivas like an interaction with colleagues rather than an interrogation by the examiners • See the clinical vivas like ward or outpatient clinical encounters • Be polite and professional with the patients Don’t be intimidated • Remember the examiners were candidates once. • They understand what you are going through! • Most of the time you will know more than the examiner does! • How you apply that knowledge is important! • We are trying to pass you, not fail you!