Developing Safety Programmes in Regional Hospitals
advertisement
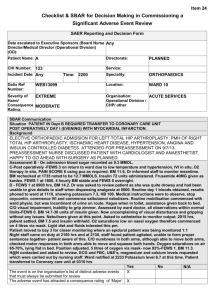
Developing Safety Programmes in Regional Hospitals PSC & PIPSQC Paediatric Patient Safety Day Birmingham, May 20th 2013 Dr. John FitzSimons HSE Ireland Dr. Santanu Maity Royal Free Hospital, London At the end of this session you will be able to…. • Discuss some of the unique features of paediatric patient safety • Understand the challenges when developing paediatric patient safety in a regional centre • Plan strategically for paediatric patient safety • Describe some proven safety solutions and know how to implement them What is patient safety? “The avoidance, prevention and amelioration of adverse outcomes or injuries stemming from the process of healthcare” Charles Vincent A Story… Organisational Accident Model Organisation & Culture Contributory factors Environment factors Management decisions & Organisational processes Care delivery problems Unsafe acts Team factors Errors Staff factors Task factors Violations Patient factors Latent failures Defences & Barriers Active failures Harm Errors of Omission “On average, children received 46.5% of the overall indicated care” Error & Harm Non-preventable Error Harm Preventable Group Discussion 1 What makes paediatric patient safety different? Patient Factors Unique Features of Paediatric Care Difference (4 D’s) Development - Physical Safety implication - Psychological e.g. age weight changes, changes in pharmacokinetics, Increased susceptibility to infection - Emotional Communication, consent Dependence (on adults) Wrong details, various people giving meds etc Consent Different disease epidemiology Rare diseases – rare treatments Demographics Poverty, language barriers System Factors System Factors Adult setting Paediatric setting Team Interchangeable (e.g. hospital at night) Specific Tasks Routine Adapted around patient Tools & Technology Standardised. Designed for adults Patient specific. Adapted from adults Work environment Designed for adults Built for medicine past Often share adult resources, labs, radiology Organisation Larger Smaller. High profile NPSA Safety incident reports (Children Vs Adults) Problem Medication Children 19% Adults 9% Treatment/procedure problem Device problem 14% 7% 6% 3% Consent issue 7% 4% Patient accident 13% 41% Safety Solutions “We cannot change the human condition, but we can change the conditions under which humans work” James Reason Group Discussion 2 What are the challenges for paediatric patient safety in a regional setting? Some Challenges for Paediatric Patient Safety in Regional Settings • Small units, fewer staff • Paediatrics usually left until “we get it right elsewhere” • Many services are shared: - A&E, OPD, Theatre - Surgery & Anaesthetics (and their trainees) - Diagnostics (Laboratory & radiology) - Allied professionals - Pharmacy • Most research comes from children’s hospitals Group Discussion 3 What would a safe paediatric service look like in your hospital? Harm Free Paediatrics 1. No, or the very least, pain or distress. 2. No unnecessary investigations or admissions or treatments. 3. No tissue injury - extravasation, pressure or other. 4. No hospital acquired infections. 5. No medication or fluids injuries. 6. Recognise sepsis or other life threatening events as early as possible and institute the right treatment. 7. Safeguarding with safe care Make Space for Improvement “Here is Edward Bear, coming downstairs now, bump, bump, bump, on the back of his head. It is, as far as he knows, the only way of coming downstairs, but sometimes he feels that there really is another way, if only he could stop bumping for a moment and think of it.” Winne the Pooh A.A. Milne Dr. John Fitzsimons First Steps • Will, Ideas, Execution • Have an aim – SMART • Have a strategy – driver diagrams • Have an improvement method - Model for Improvement SMART Aim Specific Measurable Achievable Realistic Time bound Aim – “Improve hand hygiene” SMART Aim Specific Measurable Achievable Realistic Time bound Aim – “Improve hand hygiene for all staff on the children’s ward to over 90% of cleaning opportunities by the end of June 2013” Driver Diagram Aim Primary Drivers (Processes, rules of conduct, structure) Secondary Drivers (Components & activities leading to 1º drivers) Driver Diagram Primary Drivers (Processes, rules of conduct, structure) Crispy Skin Secondary Drivers (Components & activities leading to 1º drivers) Basting Seasoning Heat Moist meat Brining Slow & low cooking flavoursome Organic chicken Herbs Components – Chestnuts, bread Volume Perfect Stuffing Great Gravy Stock Wine flavourings Good Presentation Dressing Plates The Perfect Roast Chicken Driver Diagram Primary Drivers (Processes, rules of conduct, structure) Communication Medication harm Improve safety on children’s wards Early detection & rescue of sick child Parental involvement Measure harm & learn from serious events Heathcare assoc infections Management & leadership Secondary Drivers (Components & activities leading to 1º drivers) Handover (SBAR & Critical language) Photo boards Proformas for admission Prescribing criteria Standardised medication guidelines Situation awareness (PEWS) Safety briefings Improve rescue – Simulation, debriefing, RRT Transparency On safety committee/team Ability to effect change Become a learning organisation Institute GTT SUI team Rapid reviews Debriefings Formal response to all/selected incidence forms Improve hand hygiene Surgical site infections Safety a the top of the agenda Safety culture Clear information on safety and harm Walkabouts Aim Measures Changes Execution The Improvement Guide, API The PDSA Cycle for Learning and Improvement What change can we make that will result in an improvement ? Act • What changes are to be made? • Next cycle? Study • Complete the analysis of the data •Compare data to predictions •Summarize what was learned Plan • Objective • Questions and predictions (why) • Plan to carry out the cycle (who, what, where, when) • Plan for data collection Do • Carry out the plan • Document problems and unexpected observations • Begin analysis of the data Repeated Use of the Cycle Changes That Result in Improvement A P S D A P S D Hunches Theories Ideas Group Discussion 4 How might you achieve Harm Free Paediatrics where you work? A few ideas we’ve tried… • Situation awareness • Communication • Bundles • Bring consultants to the front 24/7 PEWS Background • CEMACH report “Why Children Die” found preventable factors in 26% of reviewed cases • Centres with PICU and rapid response teams have used PEWS to trigger the team. • No accepted model “Brighton” PEWS PEWS: 24 PDSA Cycles in 9 Months K RFH PEWS • Scores on 7 parameters • Set actions according to score 0-1 Continue observations 2 Nurse in charge review 3 Above plus SHO review 4 Above plus inform registrar 5-7 Registrar review +/- Crash call SBAR Situation Background Assessment Recommendations SBAR • Situation – One sentence description of problem • Background – Details that give information • Assessment – What you think about the problem • Recommendation – What you think needs to be done SBAR Modifications • iSBAR – identification of yourself, your location and your patient. • SBAR with a Readback – After handover give a readback of highlights SBAR Notes • 11 Essential components of a hospital note 1. Patient ID 2. Date 3. Time 4. Context 5. Situation 6. Background 7. Assessment 8. Recommendation 9. Signature 10. Print Name 11. Medical Council Number Improvement Process • • • • Education Prompts Measurement and feedback Twice a week, up to 10 charts if available - Individual (out of 11) - Bundle (11 out of 11) • Changes - More education - Individual feedback - Consultant ownership Use data to drive Change % Compliance SBAR Notes 100% 90% 80% 70% 60% 50% 40% 30% 20% 10% 0% Education and visual reminders Named consultant Bundle Re-education and individual feedback Wk 1 Wk 2 Wk 3 Wk 4 Wk 5 Wk 6 Wk 7 Wk8/ Dr. A Wk 9/ Wk 10/ Wk 11 / Wk 12/ Dr B Dr C Dr D Dr E 20-Apr 27-Apr 05-May 09-May 18-May 25-May 30-May 03-Jun 07-Jun 17-Jun 22-Jun 29-Jun Weeks 25/10/2012 Items Dr. John Fitzsimons - Presentation to National Clinical Leads “To err is human, to cover up is unforgivable, and to fail to learn is inexcusable.” Sir Liam Donaldson Questions welcome