Emergency_Procedures
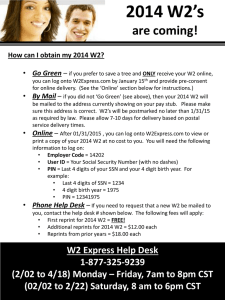
advertisement

Emergency Procedures The Surgical Technologist’s Responsibilities During Emergencies in the O.R. Setting. Blood Loss Blood loss is monitored intra-operatively to aid in determining the need for the patient to receive a blood transfusion Suction canisters have measurements on them so that an estimated blood loss (EBL) can be determined The surgical technologist should keep close track of the amount of irrigation fluid being used This information is used to calculate the amount of blood the patient has lost The irrigation used is subtracted from the total amount in the canister and this gives a more accurate amount of blood loss In some cases the circulator may weigh the sponges that have been removed from the sterile field to give another blood loss estimate This method is rarely used and would be calculated by the circulator Average blood loss can be estimated for a saturated lap sponge at 100ml per lap Saturated laps should be squeezed out into a bowl or over the suction tip and fluid suctioned into the cell saver if one is available or off table suction canister Blood Replacement When blood loss is to great to be controlled by intra-operative hemostatic control alone, blood replacement therapies are in order, but blood loss must still be controlled Blood replacement involves the administration of whole blood or blood components such as plasma, packed red blood cells, or platelets via an IV This is used to increase the circulating blood volume, to increase the number of red blood cells, and to provide plasma and platelet clotting factors that have been depleted during surgery as a result of blood loss Blood Products Blood product may be either homologous (donated by another person) or autologous (donated previously by the patient and stored for surgical use) Autotransfusion is the use of the patients own blood, which has been processed for reinfusion Cell Savers used intraoperatively are another method employed in major surgeries where a large amount of blood loss is anticipated Cell savers suction like a traditional suction, anticoagulate the blood (Heparin drip employed as part of suction tubing), filter the blood being suctioned into a reservoir, and it is readministered to the patient at the anesthesia person’s or surgeon’s discretion Cell Saver Contraindications Cell savers should not have the following fluids suctioned into the reservoir as the solutions are damaging to red blood cells: Bacitracin (lyses cells) and topical hemostatic agents such as Thrombin (coagulates cells) Or deadly to the patient if infused intravenously into their system: Amniotic fluid, presence of malignant cells, fecal material present from a perforated bowel, presence of infection Hemolytic Transfusion Reactions If blood is not properly matched prior to transfusion a hemolytic transfusion reaction or hemolytic anemia, may develop This may result from Rh incompatibility from mismatched blood transfusions Severe hemolytic reactions can be fatal and must be treated immediately The Conscious Patient May exhibit fatigue and complain of lack of energy The patient may experience rapid pulse, shortness of breath, and pounding of the heart The skin may appear jaundiced and pallor may be exhibited, especially in the palms of the hands Pallor- an unnatural paleness or absence of color in the skin The Patient Under General Anesthesia Will not show these signs, and the only signs noted may be a generalized diffuse loss of blood and a lowered blood oxygen saturation level due to the inability of the red blood cells to carry oxygen If a hemolytic transfusion reaction is suspected, The transfusion should be immediately stopped and a blood sample sent to the blood bank to rule out a mismatch Appropriate drug therapies will be started by anesthesia persons Cardiopulmonary Resuscitation Every healthcare professional should be familiar with the technique of CPR, that is, manually providing chest compressions and ventilations to patients in cardiac arrest in an effort to provide oxygenated blood to the brain and vital organs As a CST you will certify in CPR every year or two ABC’s of CPR Airway- open and free of foreign bodies Breathing- artificial breathing is done until natural breathing is restored Circulation- chest compressions are given in place of natural pulse (80 to 100 beats per minute for adult) Cardiac Arrest in the O.R. The primary responsibility of the CST is to protect the sterile field The CST should remain sterile and should keep the tables and the operative area sterile The surgical wound should be packed & covered with a sterile drape It is also the CST’s responsibility to keep track of all instruments, sponges, & needles Pay careful attention to the needs of the surgeon When CPR must be performed through the sterile field, sterile team members should perform whatever procedures are necessary (e.g., open chest heart massage) Sterility may become secondary to lifesaving procedures Malignant Hyperthermia (MH) Is a life threatening, acute pharmacogenetic disorder, that occurs during or after anesthesia Characterized by a rapid increase in body temperature, unexplained tachycardia, unstable blood pressure, muscle rigidity, tachypnea, & cyanosis Body temperature may rise to over 46C or 114F MH Is usually triggered by an anesthetic gas such as Halothane, Enflurane, or Isoflurane It may also may be triggered by a muscle relaxant such as Succinylcholine (Anectine) Succinlycholine (“succs” for short) short is the only depolarizing muscle relaxant in use today The rapid increase in body temperature is due to an increase in the metabolic state, caused by an inherited defect in the muscles of the skeletal system of some patients MH The most obvious sign to the CST will be total body rigidity Treatment of MH At the first sign of masseter spasm, or jaw muscle tightness, the anesthesia provider will stop the administration of triggering anesthetic agents & deepen the anesthesia using opioids, barbiturates, or propofol Every hospital has its own protocol for dealing with the crisis The CST should be familiar with the protocol in order to anticipate emergency needs of the surgeon MH In the case of a sudden, intense, & unanticipated attack, the surgery may need to be stopped as soon as possible Treatment includes packing the patient in ice, circulating ice water through a nasogastric tube, & irrigating the open abdominal wound with chilled irrigation fluids MH treatment DANTROLENE is the drug of choice in treating the hypermetabolism Steroids & diuretics may also be administered Ventilation will be adjusted to compensate for the increased end tidal CO2 100% oxygen will be administered Since surgery may need to be stopped as soon as possible in order to focus attention on dealing with the MH crisis, the CST must be prepared to anticipate the needs of the surgeon for quick closure and/ or actions within the sterile field to assist in cooling the patient Emergency medical services In the emergency department of the hospital, nurses triage, or sort and classify patients in order of need for immediate medical attention Emergency physicians then assess which patients may be treated in the E.R. or on the medical wards of the hospital and which need emergency surgery Indications of emergency situations The CST is frequently called on to work in emergency surgery situations or to react appropriately when the elective surgery becomes an emergency The CST must be able to anticipate emergency situations & to prepare for them in advance This skill comes with experience The entry level CST Should be able to recognize an emergency situation when it occurs Indicators such as - rapidly dropping blood pressure, cardiac dysrhythmia, & any vital signs out of normal range provide the surgical team with information about impending emergent situations Some emergencies occur suddenly, with little or no warning, such as rapid hemorrhaging (hypovolemia) It is important that the entire surgical team react in a calm & quick fashion Prior to surgery, the surgeon or anesthesia provider should be notified immediately if any of these indicators occur Indicators of emergency situations Difficulty breathing Chest pain Changes in skin color or temperature Changes in vital signs Open bleeding wounds or visible punctures not indicated on the patients chart Inability to move an extremity Misshapen / misaligned body part Disorientation or confusion The surgeon and anesthesia provider will assess the situation & will provide instruction on how the team should proceed Objectives & priorities in emergency situations The objective of emergency care & emergency & trauma surgery is to preserve life, to prevent further deterioration of the patient’s condition, and to provide whatever care necessary to restore the patient to his or her previous lifestyle Most commonly seen emergencies in the O.R. Syncope- sudden loss of consciousness Convulsions/ seizures- disturbances of nervous system function resulting from abnormal electrical activity of the brain The primary duty of the surgical team, including the CST, is to protect the patient from injury Anaphylactic reactions- An exaggerated allergic reaction to a substance or protein Substances most likely to cause a reaction are drugs such as local anesthetics, codeine, antibiotics, animal derived drugs such as insulin, contrast media & in some cases the latex found in surgical gloves & foley catheters A patient suffering a reaction generally first shows only mild inflammatory symptoms such as itching, swelling, & in some cases, difficulty breathing As the reaction progresses, the patient experiences further difficulty breathing due to bronchospasm & laryngeal edema During an anaphylactic reaction, the surgical team must maintain the airway and provide supplemental oxygen or the patient may die of respiratory failure The symptoms of vascular collapse must also be treated to prevent death from cardiovascular failure EPI Epinephrine is the first line drug in the treatment of a severe anaphylactic reaction Epi causes bronchodilation, therby reducing laryngeal spasm It also raises heart rate and raises blood pressure Because an anaphylactic reaction occurs so quickly & can so often lead to death, it is important that it be avoided altogether by identifying patient allergies Allergy information must be available to the entire surgical team This lowers the risk of provoking an anaphylactic reaction Allergies should be marked on the chart & on patients ID bracelet Any history of previous reactions should be noted in the chart Impending cardiac arrest Warning signs a CST should be able to recognize in order to anticipate emergent needs Chest pain(in awake pt.) Unstable blood pressure Tachycardia Cardiac dysrhythmia Respiratory changes Hypovolemia Laryngospasm (anesthesia having difficulty ventilating the patient) Remember: The primary responsibility of the STSR in any emergency is to: MAINTAIN THE STERILE FIELD