Adult Health Nursing II
Block 7.0
Topic: Respiratory Nursing, part 1
Module: 4.1
RESPIRATORY PROBLEMS
Nursing Care &
Considerations of the Client
With Respiratory Conditions
ASSESSMENT
*Obstructive Sleep Apnea (OSA)
*Head & Neck CA
*Tracheostomy and Laryngectomy
Tubes
Pharmacology:
Provigil
Heparin
Protamine sulfate
Warfarin (Coumadin)
Vitamin K
Alteplase (Activase)
Codeine
*Lung Cancer
*Pulmonary Edema
*Pulmonary Embolism
*Chest Trauma
*Problems of the Pleura
*Chest Tubes
*Acute Respiratory Failure
*ARDS
*Mechanical Ventilation
Block 7.0
Module 4.1
Nursing
Intervention
&
Evaluation
Learning Outcomes
1. Relate the pathophysiology, risk factors,
diagnostics, and interventions for the client with
obstructive sleep apnea (OSA).
2. Examine the risk factors, clinical manifestations,
interventions, and nursing responsibilities for the
patient with head and neck cancer.
3. Compare and contrast the indications of and the
nursing care responsibilities for the client with a
tracheostomy tube versus a laryngectomy tube.
Block 7.0
Module 4.1
Learning Outcomes
4. Relate the risk factors, clinical manifestations,
interventions, and nursing responsibilities for the
client with lung cancer.
5. Examine the risk factors, clinical manifestations,
diagnostics, interventions, and nursing
responsibilities for the client with pulmonary
embolism.
6. Compare and contrast the use of heparin and
coumadin in patients with deep vein thrombosis
(DVT) and pulmonary embolus (PE).
Block 7.0
Module 4.1
Learning Outcomes
7. Identify risk factors and compare and contrast
clinical manifestations, interventions, and nursing
responsibilities for the client with acute respiratory
failure (ARF) versus acute respiratory distress
syndrome (ARDS).
8. Explain pathophysiology and possible complications
of pulmonary contusion.
9. Explain the pathophysiology, assessment and
interventions for the client with flail chest.
Block 7.0
Module 4.1
Learning Outcomes
10. Compare and contrast the pathophysiology and
interventions for pleural effusion and pleurisy.
11. Relate the pathophysiology, clinical manifestations,
and interventions for the client with pneumothorax,
hemothorax, and tension pneumothorax.
12. Prioritize nursing care for the client with a chest tube.
13. Prioritize nursing care for the client on mechanical
ventilation.
Block 7.0
Module 4.1
Learning Outcomes: Pharmacology
Provigil
Heparin
Protamine sulfate
Warfarin (Coumadin)
Vitamin K
Alteplase (Activase)
Codeine
Block 7.0
Module 4.1
Key Terms
Tracheotomy
Tracheostomy tube
Laryngectomy tube
Invasive mechanical ventilation
Non-invasive positive pressure
ventilation
Block 7.0
Module 4.1
Block 7.0
Module 4.1
Obstructive Sleep Apnea (OSA)
Breathing disruption during sleep lasting >10 seconds
& occurring at least 5x/hr
Most common cause: upper airway obstruction by soft
palate or tongue
Risk factors: Obesity w/BMI (body mass index) >30,
neck circumference >17 in, large uvula, smoking,
enlarged tonsils & adenoids
BMI = (metric) wt/ht2
BMI = (non-metric) wt / ht2 x 702
Block 7.0
Module 4.1
Obstructive Sleep Apnea (OSA)
Repeated cycles of apnea disrupt deep sleep which is
needed for maximum rest
S/sx: Excessive daytime sleepiness, snoring, inability
to concentrate, headache, irritability, waking up tired,
personality changes, frequent nocturnal awakening
Pts may not be aware they have OSA; often family will
be first to observe
Dx: PSG (polysomnography) sleep study
Block 7.0
Module 4.1
Polysomnography (sleep study)
Measures
depth & type
of sleep,
respiratory
effort, O2 sat,
& muscle
movement.
Block 7.0
Module 4.1
Interventions for OSA
Pharmacology:
Provigil used for narcolepsy
(uncontrolled daytime sleep) & OSA by
promoting daytime wakefulness does
not treat the cause of OSA.
Surgical management:
– Adnoidectomy and/or uvulectomy
– Uvulopalatopharyngoplasty (UPP) -remodeling of entire posterior oropharynx
Block 7.0
Module 4.1
Interventions for OSA
Nonsurgical management:
– Weight loss or change in sleeping position
– Non-invasive positive pressure ventilation
to hold open the upper airways:
• BiPAP (bilevel positive airway pressure)
• APAP (autotitrating positive airway pressure)
• CPAP (nasal continuous positive airway pressure)
• May also be used for: Acute/chronic respiratory failure,
acute pulmonary edema, acute exacerbations of COPD,
chronic heart failure
Block 7.0
Module 4.1
Noninvasive Positive-Pressure Ventilation
(BiPAP, APAP, or CPAP)
Technique uses positive pressure to keep alveoli open
and improve gas exchange without airway intubation.
Improves tidal volume & prevents collapse of the
alveoli.
May deliver oxygen or just use room air
Nasal mask or full face mask delivery system for either
BiPAP, APAP, or CPAP
RT should set up & handle these.
Block 7.0
Module 4.1
Nursing Responsibilities
Check that patient’s face mask fits properly.
Assess his face for signs of pressure.
Patient may experience anxiety/dyspnea due to
mask.
Reassure patient; stay with him for 30 minutes after
starting
Watch for gastric distention that could lead to
aspiration.
Block 7.0
Module 4.1
BiPAP & CPAP Masks
Block 7.0
Module 4.1
Head and Neck Cancer
Head & neck cancer is curable when treated
early.
> 80% are squamous cell carcinomas
Head and neck cancers can disrupt breathing,
eating, facial appearance, self-image, speech, and
communication.
Physiological & psychosocial effects can be
devastating for the patient & family even when
treated successfully.
Block 7.0
Module 4.1
Risk Factors for Head & Neck CA
2 major risk factors:
Prolonged use of alcohol
History of heavy smoking (smoke or
smokeless)
– Calculate pt’s smoking history in packyears (# of packs per day X # of years
smoked). Example: 2 packs/day X 25 yr =
50 pack-years.
Block 7.0
Module 4.1
Oral & Laryngeal Cancers
4% of all cancer diagnoses
Mucosal cancer lesions may be:
– White, patchy lesions (leukoplakia)
– Red, velvety patches (erythroplasia)
Metastasize (spread) to local areas (lymph nodes, muscle,
bone) or distant sites (lungs, liver)
Degree of malignancy:
– Early: lesions are well differentiated
– More advanced: lesions are moderately differentiated
– Late: lesions are poorly differentiated
Block 7.0
Module 4.1
SIGNS OF ORAL CANCER
Leukoplakia
Erythroplasia
Block 7.0
Module 4.1
Started using spit tobacco at
age 13
Was diagnosed with oral
cancer at age 17
Has been through 35 painful
surgeries
Parts of his neck and tongue
were removed
Block 7.0 Module 4.1
S/Sx of Oral & Laryngeal Cancer
Pain
Lump in mouth,
neck or throat
Dysphagia
Mouth sore that
does not heal in 2
weeks
Hoarseness
(painless)
Block 7.0
Persistent or
recurrent sore
throat
Color changes in
mouth
Persistent,
unexplained oral
bleeding
Anorexia & wt loss
Module 4.1
Interventions for Oral & Laryngeal Cancer
Radiation therapy
Chemotherapy
Surgical Intervention:
…goal is to remove the tumor, maintain airway
patency & provide for optimal cosmetic appearance
– Radical neck dissection
– Partial or total laryngectomy
Block 7.0
Module 4.1
Radical Neck Dissection
w/Closure
Block 7.0
Oral Cancer from
Smokeless Tobacco
Module 4.1
Laryngeal Cancer
Comprises 2% of all cancers
Hoarseness may occur because of tumor
bulk and inability of the vocal cords to come
together for normal phonation.
Cancer of true vocal cords is slow growing
d/t decreased lymphatic supply. Elsewhere
in larynx, abundant lymph tissue ensures
cancer spreads rapidly w/mets to deep neck
lymph nodes.
Block 7.0
Module 4.1
Block 7.0
Module 4.1
LARYNX
The larynx has 3
main parts:
1. Top part is
supraglottis
2. Glottis &
vocal cords
in middle
3. Subglottis at
bottom &
connects to
windpipe
Block 7.0
Module 4.1
Assessment & Diagnostics
History & physical (H&P)
Laryngoscopy or panendoscopy with
biopsy
TNM (Tumor-Node-Metastasis) System:
– Used for staging & classification
– Determines treatment modalities
CT, MRI, PET scan
Block 7.0
Module 4.1
Surgical Management
Partial laryngectomy w/wo radical neck
dissection on involved side tracheostomy &
tracheostomy tube placed to protect airway &
is usually temporary stoma is not sutured
open
Total laryngectomy requires permanent
tracheal stoma & laryngectomy tube to
maintain airway stoma is sutured open
– Results in permanent loss of the voice
– Stoma opening is pt’s ONLY airway
– No risk for aspiration of food & fluids into lungs
since esophagus & trachea are separated
Block 7.0 Module 4.1
– No voice, but normal
swallowing
Tracheostomy
Tracheotomy is the surgical incision
into the trachea for the purpose of
establishing an airway.
Tracheostomy is the stoma, or opening,
that results from the procedure of a
tracheotomy.
Tracheostomy may be temporary or
permanent
Block 7.0
Module 4.1
Incision for Trach (Tracheotomy)
Block 7.0
Module 4.1
Block 7.0
Module 4.1
Postoperative Care
#1 priority post-op is airway maintenance & ventilation.
Monitor airway patency, vital signs, hemodynamic status
(increased BP, decreased AHR), comfort level.
Assess for complications:
– Respiratory distress & hypoxia AEB confusion, restlessness, irritation,
agitation, tachypnea, use of accessory muscles & decreased SaO2 (pulse ox)
– Hemorrhage: apply direct pressure & summon help
– Infection: increased temp & pulse, purulent drainage w/odor, increased
redness & tenderness
– Wound breakdown common d/t poor nutrition, smoking history, ETOH abuse,
wound contamination & previous radiation therapy.
Block 7.0
Module 4.1
Carotid Artery Rupture
Extensive surgical wounds in neck area can
put carotid artery at risk for rupture.
– If leak is suspected, call Rapid Response Team
– DO NOT apply pressure could cause immediate rupture
– If rupture occurs, apply constant, direct pressure over site & secure airway
– Transport patient to OR for resection
– Do not leave patient.
– Patient at high risk for stroke & death.
– To prevent, keep wound dressing wet
Block 7.0
Module 4.1
Other Possible Complications
Assess for:
– Pneumothorax – air in pleural space
– Subcutaneous emphysema – crepitus
air leak into neck, chest & face tissues if
skin is puffy w/crackling sensation, call
physician immediately
– Bleeding
– Infection
Block 7.0
Module 4.1
Subcutaneous Emphysema
Block 7.0
Module 4.1
Maintaining a Patent Airway
Semi-Fowler’s or high Fowler’s position
Tracheostomy tube (usually temporary) if partial laryngectomy
done. Stoma NOT sutured open.
Laryngectomy tube (patient’s only airway) if total laryngectomy
done. Stoma IS sutured open. Care same as trach tube.
Removed 3-6 wks post-op when stoma (surgical opening into
trachea) is healed.
Turn, cough and deep breath
Increased mucus secretions -- suction
Humidification (nebulizer) to decrease cough, mucus production,
crusting at site
Stoma care: combined wound & airway care
Block 7.0
Module 4.1
Maintaining a Patent Airway (cont’d)
Possible complications for tracheostomy
tubes:
– Tube obstruction from secretions or tube displacement
– Tracheostomy tube dislodgment: accidental decannulation.
Tube dislodgment in 1st 72h post placement is emergency
ventilate patient w/face mask & ambu bag. Call for help.
Always have duplicate trach tube, obturator & trach insertion
tray at bedside at all times. If >72 hr post-op, use obturator to
open site & place new trach tube.
Block 7.0
Module 4.1
Temporary Tracheostomy –
Tracheostomy Tube
Opening is not sutured open
A tracheostomy tube must always be in place to prevent closure of
the opening
Placed for partial laryngectomy & mechanical ventilation
temporary airway only pt can still breath through mouth & nose
Has inner & outer cannula inner cannula may be disposable or
reusable
Outer cannula may be cuffed or not
Outer cannula may be fenestrated allows pt to speak when
capped & inner cannula removed
Block 7.0
Module 4.1
Trach Tube, Inner Cannula, Obturator
Block 7.0
Module 4.1
Permanent Tracheostomy –
Laryngectomy Tube
Placed after total laryngectomy pt’s only airway for life
trachea no longer part of oral airway
Opening is sutured open laryngectomy tube can be taken in
& out immediately for cleaning or replacement
Prevents shrinkage of stoma until it heals in 3-6 weeks
After open stoma heals, opening is permanent & laryngectomy
tube not needed
Not cuffed & has outer cannula only
Block 7.0
Module 4.1
Total laryngectomy
requires permanent tracheal
stoma & laryngectomy tube to
maintain airway stoma is
sutured open
•Results in permanent loss of
the voice
•Stoma opening is pt’s ONLY
airway
•No risk for aspiration of food &
fluids into lungs since esophagus &
trachea are separated
•No voice, but normal swallowing
Block 7.0
Module 4.1
Laryngectomy Tube & Permanent
Stoma
Block 7.0
Module 4.1
Trach Suctioning and Care
Suctioning maintains a patent airway and promotes
gas exchange.
Assess need for suctioning from the client who
cannot cough adequately.
-----Trach suctioning (hospital) is strict sterile technique
Always secure tracheostomy tube in place to prevent
accidental decannulation
See Craven’s Fundamentals of Nursing,
pp. 866-873
Block 7.0
Module 4.1
Complications of Trach Suctioning
Suctioning can cause:
– Hypoxia (see causes to follow)
– Tissue (mucosal) trauma (see slide)
– Infection strict sterile technique never use
oral suction equipment to suction an artificial
airway
– Vagal stimulation results in severe bradycardia
& dysrhythmias stop suctioning immediately &
oxygenate pt
– Cardiac dysrhythmias from hypoxia caused by
suctioning stop suctioning & oxygenate pt
– See Chart 30-3, p. 584, for Best Practice
Block 7.0
Module 4.1
Causes of Hypoxia with Trach
Suctioning
Ineffective oxygenation before, during, and after suctioning
oxygenate before, during, & after w/100% O2
Use of a catheter that is too large for the artificial airway
standard size is 12 or 14 Fr
Prolonged suctioning time never longer than 10-15 sec.
Excessive suction pressure 80-120 mm/Hg
Too frequent suctioning limit 3 passes
Block 7.0
Module 4.1
Prevention of Tissue Damage
Do not apply suction during insertion.
Cuff pressure can cause mucosal ischemia
use minimal leak technique.
Check cuff pressure often (<25cm H2O)
Prevent tube friction and movement
secure to keep tube mid-line
Block 7.0
Module 4.1
Block 7.0
Module 4.1
Air Warming and Humidification
The tracheostomy tube bypasses the
nose and mouth, which normally
humidify, warm, and filter the air.
Air must be humidified use
humidifier bottle at wall O2 setup
Block 7.0
Module 4.1
Stoma Care
Apply shield over the tracheostomy
tube or laryngectomy stoma when
bathing to prevent water from entering
the airway.
Apply protective stoma cover or guard
to protect the stoma during the day.
Block 7.0
Module 4.1
Stoma Covers
Block 7.0
Module 4.1
Weaning from a Temporary Trach Tube
Weaning is a gradual decrease in the tube size and
ultimate removal of the tube.
Cuff is deflated as soon as the client can manage
secretions and does not need assisted ventilation.
Trach tube is capped as patient tolerates;
supplemental O2 by nasal cannula may be needed.
Block 7.0
Module 4.1
Pain Management for Laryngeal
Cancer
Opioids used with caution since they depress
respirations (morphine, codeine, hydromorphone,
hydrocodone, oxycodone, fentanyl, methadone,
propoxyphene)
Acetaminophen alone
Nonsteroidal anti-inflammatory drugs
(NSAIDS)
Elavil (amitriptyline) for nerve-root pain
Block 7.0
Module 4.1
Nutrition with Tracheostomy Tube
May not be allowed to eat for 10-14 days
Alternative sources of nutrition:
– Nasogastric (NG) tube feeding
– Gastrostomy (G-tube) feeding
– Jejunostomy (J-tube) feeding
– Parenteral nutrition (TPN/PPN)) until the GI
tract recovers from the effects of
anesthesia
No risk of aspiration after total laryngectomy
because the airway and esophagus are
completely separated
Block 7.0
Module 4.1
Risk for Aspiration w/Tube Feedings
If not a total laryngectomy, pt is at risk
Swallow study
Enteral or tube feedings aspiration
precautions
–
–
–
–
Semi-Fowler’s / high Flowler’s position
Strict adherence to tube feeding regimen
No bolus feeding at night
Check residual feeding every 4-6 hr for
continuous feeding; prior to each can of feeding if
bolus feeding
Block 7.0
Module 4.1
Nutrition with Tracheostomy Tube
When po, start with thickened liquids & advance as tolerated
May have diminished sense of smell & taste
Swallowing can be a major problem for the client with a
tracheostomy tube in place.
If balloon is inflated, it can interfere with the passage of food
through the esophagus.
High Fowler’s or semi-Fowler’s position for eating. Elevate
head of bed for at least 30 minutes after client eats to prevent
regurgatation & aspiration.
Block 7.0
Module 4.1
Speech and Communication with
Tracheostomy Tube
Patient with tracheostomy tube can speak with
a cuffless tube, fenestrated tube, or cuffed
fenestrated tube that is capped or covered.
Patient with laryngectomy cannot speak pt
has had total laryngectomy
Client can write.
Ask “yes” or “no” questions.
One-way speaking valve that fits over the tube & replaces the
need for finger occlusion can be used to assist with speech
(Passy-Muir valve).
Block 7.0
Module 4.1
Passy-Muir Valve
Block 7.0
Module 4.1
Speech Rehabilitation with Total
Laryngectomy
Patient with total laryngectomy can no
longer speak.
Alternatives:
Writing or using a picture board
Artificial larynx
Esophageal speech: sound produced by “burping”
the air swallowed or injected into the esophageal
pharynx and shaping the words in the mouth
Mechanical devices (electrolarynges)
Block 7.0
Module 4.1
Reducing Anxiety & Depression
Multidisciplinary team conference w/pt & family: RN, physician,
RT, ST, SW, dietitian, & home health RN
Fear & anxiety r/t cancer dx, possible loss of voice, possible
disfigurement
Visit by other laryngectomy pt usually helpful
Antianxiety drugs such as Valium (diazepam) administered with
caution because of possibility of respiratory depression
Block 7.0
Module 4.1
Promoting Positive Body Image &
Self-Esteem
Disfiguring surgery & loss of voice is a threat to pt’s body image
& self-esteem
Use positive approach
Help client & family set realistic goals
Involve pt & family in self-care ASAP
Ease client into more normal social environment after
hospitalization
Advise loose-fitting, high-collar shirts or sweaters, scarves,
jewelry, or cosmetics to cover the laryngectomy stoma
Block 7.0
Module 4.1
Patient Education for Tracheostomy
Tube & Stoma Care
Tracheostomy/laryngectomy tube & stoma care clean not
sterile technique in home setting
Instruct proper suctioning technique
Need to increase humidity in home with humidifier & nebulizer
if needed
Air-conditioned air may be too cool, too dry
Apply shield over the tracheostomy tube or laryngectomy
stoma when bathing to prevent water from entering the airway.
Don’t swim!!
Apply protective stoma cover or guard to protect the stoma
during the day.
Good oral hygiene w/frequent brushing
Medical alert bracelet
Block 7.0
Module 4.1
Lung Cancer
Cause: chronic tissue irritation or
inflammation d/t repeated exposure to
inhaled substances (cigarette smoke,
occupational or environmental agents)
80-90% linked to cigarette smoking
(includes 2nd-hand smoke)
Block 7.0
Module 4.1
Lung Cancer
Leading cause of cancer deaths in both men & women
accounting for 28% of all cancer deaths (>165,000
deaths/year)
5-year survival (after diagnosis) rate only 14%
Slow growing – takes 8-10 yr to reach 1cm, smallest
detectable lesion on an x-ray
Low survival rate d/t dx at a late state when metastasis
(spread) has already occurred
Metastasize by (1) direct extension; (2) thru the blood
(hematogenous); & invading lymph glands & vessels.
Block 7.0
Module 4.1
Block 7.0
Module 4.1
Signs & Symptoms of Lung Cancer
Insidious, often nonspecific, appearing late in disease
process
#1 sx: dry, persistent cough or change to chronic,
productive cough
Hemoptysis (coughing up blood)
Recurrent lung infections w/chills, fever
Dyspnea; painful breathing; wheezing
Weight loss, fatigue
Block 7.0
Module 4.1
Diagnostic & Lab Tests
Chest x-ray, chest CT
Sputum cytology
Bronchoscopy / mediastinoscopy w /
biopsy
Needle biopsy
MRI
PET scan to detect metastasis
CEA (carcinoembryonic antigen titer)
Block 7.0
Module 4.1
Medical Management
May include combination of surgery, chemo,
& radiation therapies
Chemotherapy may provide pain relief but
does not usually cure
– Useful in rx of mets to brain, spine, pericardium
– Side effects: N/V, alopecia (hair loss), anemia,
immunosuppression, mouth sores thrombocytopenia
(decreased platelets)
Radiation therapy may cure, relieve sx,
reduce size of tumor
Block 7.0
Module 4.1
Surgical Management
Preferred tx, esp. if non-small cell CA & no mets
Lobectomy – resection of entire lobe
Pneumonectomy – resection of entire lung
Segmentectomy – resection of bronchus, pulmonary
artery & vein, & portion of involved lung segment
Wedge resection – removal of peripheral portion of
small, local areas
Block 7.0
Module 4.1
Block 7.0
Module 4.1
Interventions for Palliation
Oxygen therapy
Drug therapy
Radiation therapy
Laser therapy
Thoracentesis and pleurodesis
Dyspnea management
Pain management
Hospice & end-of-life issues
Block 7.0
Module 4.1
Nursing Responsibilities
Manage pain, n/v, dyspnea, fatigue
Drugs for sx relief
Oxygen
Ways to reduce fatigue
Psychological support for pt & family
– Identify community resources
– Help family deal with poor prognosis
– End-of-life treatment options (hospice, home health)
Block 7.0
Module 4.1
Pulmonary Edema
Pulmonary edema is swelling and fluid accumulation in
the lungs. The extra fluid and swelling drown the
patient by impairing healthy gas exchange with the
7.0 cause
Module 4.1 respiratory failure.
circulating blood andBlock
can
Treatment for
Block 7.0
Module 4.1
Pulmonary Embolism (PE)
Clot enters bloodstream & lodges in pulmonary vessels.
Blood clot is most common, but may also be fat, air, amniotic fluid,
tumor tissue.
Obstructs pulmonary blood flow, leading to decreased systemic
oxygenation, pulmonary tissue hypoxia & potential death.
90-95% of PE arise from DVTs (deep vein thrombosis) in the leg.
10% mortality rate; many die within 1st hour
Block 7.0
Module 4.1
Pulmonary Embolus (PE)
Block 7.0
Module 4.1
Block 7.0
Module 4.1
Block 7.0
Module 4.1
Risk Factors for PE
DVT #1 90-95%
Prolonged immobility (lying or sitting)
Central venous catheters, including PICCs
Surgery (orthopedic, pelvic, abdominal, recent
pregnancy/childbirth)
Obesity
Advanced age
Hypercoagulability (anemia, estrogen therapy, birth
control pills, smoking)
History of thromboembolism
Block 7.0
Module 4.1
S/Sx of PE
Symptoms (subjective):
Dyspnea, sudden
onset
Sharp, inspiratory
chest pain
Apprehension,
restlessness
Feeling of impending
doom
Block 7.0
Signs (objective):
Tachypnea, gasping
Crackles, diminished
breath sounds
Cough, hemoptysis
Tachycardia
Hypotension
Fever, low grade
Decreased SaO2
Module 4.1
Diagnostic & Lab Tests
Spiral CT most often used to dx PE
ABGs – indicate hypoxemia, hypocapnia initially (respiratory
alkalosis) later will have hypercarbia w/respiratory acidosis
mixed w/metabolic acidosis d/t lactic acid buildup
Venous U/S to determine presence of DVT to support PE dx
Pulmonary angiogram is most specific test but not usually
done d/t risk
Block 7.0
Module 4.1
Pharmacology for PE
Heparin (an anticoagulant) is initial treatment of
choice
– Keeps embolus from enlarging & prevents formation of new clots.
Does not dissolve clot. Pt’s own body dissolves the clot.
– High risk for bleeding.
– Monitor lab: therapeutic range for PTT/aPTT is 1.5-2 x baseline
(baseline usually 25-39 sec) (see sample heparin protocol sheet)
(see Chart 34-5, p. 682)
– Antidote for heparin overdose: protamine sulfate IV
– Avoid antiplatelet drugs like aspirin & Plavix increases risk of
bleeding
Block 7.0
Module 4.1
Pharmacology for PE
Warfarin (Coumadin) (an anticoagulant) is
started on day 3 of heparin therapy long
half-life (3-5 days)
– Pt continues on both heparin & warfarin until INR 2-3, then
heparin d/c’d.
– Monitor lab: Therapeutic range for INR: 2-3
– Antidote for coumadin overdose: Vit. K SQ or IV
– Avoid aspirin & acetaminaphen (increases risk for bleeding)
– Avoid foods high in Vit K (green, leafy vegetables decrease
effects of warfarin)
Block 7.0
Module 4.1
Pharmacology for PE
Streptokinase (a thrombolytic/fibrinolytic
drug) – used in massive PE with shock &/or
hypotension to dissolve clot. HIGH risk for
bleeding. Bleeding is most common side
effect.
Other anticoagulants – LMWH (low molecular
weight heparin) – Lovenox SQ 1mg/kg
Pain meds, antianxiety meds
Block 7.0
Module 4.1
Interventions for PE
O2
Monitor q1-2 hr & prn:
– Vital signs
– Respiratory status (lung sounds, crackles,
cyanosis, increased dyspnea)
– C/V status (dysrhythmias, edema)
Surgery
-- Embolectomy if clot is very large & if
fibrinolytic therapy contraindicated (hx of
cerebral or GI bleed)
-- Inferior vena cava filter (Greenfield filter)
placement in high risk patients, esp. if
7.0 Module 4.1
anticoagulants areBlockcontraindicated
Block 7.0
Module 4.1
Block 7.0
Module 4.1
Nursing Interventions for PE
Bedrest (24-48 hr) in semi-Fowler’s position
Turn, cough & deep breath
O2: monitor ABGs, SaO2 , nebulizer rx, incentive spirometer
Monitor q1-2h & prn: vital signs, respiratory status (lung sounds,
crackles, cyanosis, increased dyspnea), & C/V status (edema,
dysthythmias, chest pain)
Assess for internal & external bleeding
Assess for +Homans’ sign (unreliable)
Assess for s/sx of obvious &/or occult bleeding (easy bruising,
blood in stools/urine/emesis)
See Chart 34-6, p. 683
Block 7.0
Module 4.1
Homan’s Sign
Forced plantar flexion of the ankle may elicit
pain response in leg. Unreliable do not use.
Block 7.0
Module 4.1
Health Promotion & Prevention of PE
Stop smoking esp. if on birth control pills
Reduce weight, increase physical activity
Anticoagulants for pts w/atrial fib
Anticoagulants & compression stockings for post-op & other atrisk pts
Ambulate pt ASAP post-op
If traveling or sitting for long periods, get up frequently & drink
plenty of fluids.
Refrain from massaging leg muscles.
Avoid tight garters, girdles, belts
Prevent pressure under the popliteal space (don’t put pillows
under pt’s knees)
Block 7.0 Module 4.1
Patient Education for Anticoagulants
Prevent bleeding from anticoagulants
– Use electric razor
– Avoid sharps
– Soft bristle toothbrush
– No OTC meds w/o MD’s permission
– Avoid laxatives, may affect Vit K
absorption
– Report dark, tarry stools
– Wear ID or carry med card
Block 7.0
Module 4.1
Chest Trauma
About 25% of civilian traumatic deaths result
from chest injuries
Blunt chest trauma: sudden pressure to chest
wall. Most common:
– Steering wheel or seatbelt in MVA
– Fall
– Bicycle crash
Penetrating trauma: foreign object
penetrates chest wall. Most common:
– Stabbing
– Gunshot wounds
Block 7.0
Module 4.1
Assessment & Diagnostics for Chest
Trauma
Assess for patent airway
Assess for bleeding, open wounds
Assess rate, depth, symmetry of resp
Assess for stridor (late sign), cyanosis,
trauma to mouth, face, neck
Assess VS & neuro status
CXR, CT, CBC, lytes, ABGs, SaO2, EKG
Totally undress pt so nothing is missed
Block 7.0
Module 4.1
Pulmonary Contusion
Most common chest injury in U.S.
Often results from rapid deceleration in MVA
Respiratory failure develops over time rather than immediately
Damage to lung tissues resulting in hemorrhage & localized
edema decreased lung movement & gas exchange
May not be initially evident (even on CXR), may not develop
until 1-2 days post injury
S/sx: dyspnea, hemoptysis, hypoxia
Rx: O2 support, analgesics (opioids), ATBs, may need
mechanical vent if ARDS
Block 7.0
Module 4.1
Rib Fractures
Rib fractures 2nd most common chest injury, usually
d/t blunt trauma
Uncomplicated rib fx heal spontaneously
S/sx: severe chest pain resulting in compromised
respirations; possible crepitus if rib punctures lung
Main focus: pain control so pt’s respirations will not
be compromised
Avoid analgesics that cause respiratory depression
Block 7.0
Module 4.1
Flail Chest
Caused by multiple rib fractures resulting in instability of chest
wall with paradoxical breathing – portion of lung under injured
chest wall moves in on inspiration & out on expiration
Usually unilateral
Results in severe respiratory distress w/decreased gas
exchange & ability to cough
High mortality (40%), esp. in older pts
S/sx: pain, dyspnea, cyanosis, SOB, tachycardia, hypotension,
anxiety
Block 7.0
Module 4.1
Flail Chest
Block 7.0
Module 4.1
Interventions for Flail Chest
Maintain patent airway
Agitation, irrational, combative
behavior may indicate decreased O2 to
the brain
Maintain fluid volume
Maintain chest wall integrity
Stabilized w/positive-pressure
ventilation
Block 7.0
Module 4.1
Interventions for Flail Chest
Humidified O2
Analgesics (opioids)
Turn, cough, deep breath
May need mechanical vent if shock or
respiratory failure occurs
Monitor: ABGs, VS, fluid & electrolyte
balance for hypovolemia or shock
Block 7.0
Module 4.1
Problems of the Pleural Space
Lies between the parietal pleura (membrane lining the
chest cavity) and the visceral pleura (surrounds the
lungs)
Holds about 50 ml of lubricating fluid
Creates a negative pressure that keeps the lungs
expanded
Excess fluid or air accumulation in the pleural space
limits lung expansion and leads to respiratory distress
Block 7.0
Module 4.1
Pleural Space
Block 7.0
Module 4.1
PROBLEMS OF THE PLEURA
Pneumothorax: air in pleural space
Hemothorax: blood in pleural space
Pleural effusion: fluid in pleural space
Pulmonary Empyema: pus in pleural
space
Pleurisy: inflammation of the pleura
Block 7.0
Module 4.1
Pneumothorax &/or Hemothorax
Pneumothorax: Air enters pleural space
Hemothorax: Blood enters pleural space
Prevents lung expansion & exchange of O2 & CO2.
Causes the lung to collapse
Severity depends on amount of lung that is collapsed
Block 7.0
Module 4.1
Pneumothorax &/or Hemothorax
Block 7.0
Module 4.1
S/sx of Pneumothorax/Hemothorax
Sudden onset of pleuritic pain
Tachypnea, dyspnea
Anxiety, apprehension
Reduced or absent breath sounds on affected side
Hypotension, tachycardia
Crepitus (subcutaneous emphysema)
Block 7.0
Module 4.1
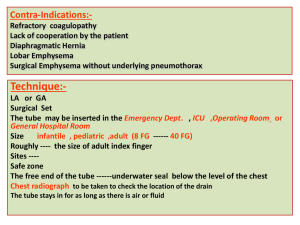
Causes for Pneumo/Hemothorax
Open pneumothorax: sharp chest wound (stab or
gunshot wound, surgical thoracotomy,
thoracentesis, chest tube placement, lung biopsy)
Closed pneumothorax: no external wound
– Interstitial lung disease (cancer, TB)
– ARDS
– Mechanical ventilation
Block 7.0
Module 4.1
Block 7.0
Module 4.1
Interventions for
Pneumo/Hemothorax
Goal: evacuation of air &/or blood from pleural space
Oxygen therapy
Pain management
Thoracentesis
Chest tube to water seal and/or suction
Patient with hemothorax may need open thoracotomy for
massive (>1500 mL) &/or persistent bleed (>200 mL over 3 hours)
Monitor: VS, respiratory status, blood loss, chest tubes
Block 7.0
Module 4.1
PLEURODESIS
Procedure that causes the pleura around the lung to
stick together and prevents the buildup of fluid in the
pleural space.
This procedure is done in cases of severe recurrent
pleural effusion (fluid around the lungs), as from
cancer, to prevent the reaccumulation of fluid.
In pleurodesis, an irritant (such as sterile talc powder)
is instilled inside the space between the pleura in order
to create inflammation which tacks the two pleura
together.
This procedure obliterates the space between the
pleura and prevents re-accumulation of fluid.
Block 7.0
Module 4.1
Pleurodesis
Block 7.0
Module 4.1
Tension Pneumothorax
Collapse of lung d/t air entering the pleural
space on inspiration, but does not leave on
expiration heart, great vessels & thorax in
mediastinum shifts to unaffected side
Pressure in lung decreases venous return
leading to decreased filling of the heart &
decreased cardiac output.
Develops rapidly, quickly fatal if not detected
& treated
Block 7.0
Module 4.1
Block 7.0
Module 4.1
Tension Pneumothorax
Emergency situation
mediastinal shift
to the unaffected
side twists the heart
& great vessels.
Assess the trachea
for midline position.
Block 7.0
Module 4.1
S/sx of Tension Pneumothorax
Asymmetry of thorax w/absence of
breath sounds on affected side
Tracheal deviation or mediastinal shift
to unaffected side
Respiratory distress, cyanosis, anxiety
Dx: CXR, ABGs w/resp alkalosis
Interventions: thoracentesis &/or
chest tube
Block 7.0
Module 4.1
Tracheobronchial Trauma
Tear of tracheobronchial tree d/t blunt force trauma
&/or rapid deceleration.
Develop massive air leaks into the mediastinum
w/extensive crepitus (SQ emphysema)
If mainstem bronchus tear, monitor for tension
pneumothorax when intubated & placed on
mechanical vent
Managed w/tracheotomy below level of injury if
tracheal trauma
Block 7.0
Module 4.1
Pleural Effusion
Collection of fluid in the pleural space
Usually d/t other disease: heart failure, TB,
pneumonia, pulmonary embolus,
bronchogenic cancer
Fluid may be clear, bloody, or purulent
S/sx:
– Those of underlying disease – fever, chills, pleuritic CP w/pneumonia;
dyspnea, coughing w/CA
– SOB w/large fluid collection d/t restriction of space
Diagnostics & assessment:
– Decreased breath sounds; flat, dull w/percussion
– Chest x-ray, chest CT, thoracentesis
– Pleural fluid C&S, TB, cytology for cancer, chemistry, others
Block 7.0
Module 4.1
Medical Management of Pleural
Effusion
Treat underlying cause (heart failure,
pneumonia, cancer)
Thoracentesis or chest tube to remove
fluid.
Pleurodesis for recurrent pleural
effusions (usually d/t cancer)
Nursing management:
– Pain control
– Care of chest tube
– Patient/family education
Block 7.0
Module 4.1
Block 7.0
Module 4.1
Pulmonary Empyema
A collection of pus in the pleural space.
May enclose the lung in a thick exudative membrane
Most common causes: bacterial pneumonia and lung
abscess. Infected pleural effusion, penetrating chest
trauma.
S/sx: fever, night sweats, pleural pain, cough,
dyspnea, anorexia, wt loss
Block 7.0
Module 4.1
Diagnostics & Interventions for
Pulmonary Empyema
Dx: CXR, chest CT, thoracentesis
Interventions include:
– Prolonged use of antibiotics for identified
organism (4-6 wks)
– Emptying the empyema cavity using
thoracentesis, chest tube, or open
thoracotomy
– Re-expansion of the lung
Block 7.0
Module 4.1
Pleurisy
Inflammation of both layers of the pleurae (parietal &
visceral)
May develop w/pneumonia or URI
Sharp pain on inspiration d/t inflamed pleural
membranes rubbing together
Usually unilateral
Diagnostics: chest x-ray, sputum C&S,
thoracentesis for pleural fluid specimen
Block 7.0
Module 4.1
Medical Management of Pleurisy
Treat underlying cause (pneumonia, URI)
Monitor s/sx pleural effusion
Analgesics: NSAIDs to allow deep
breaths & effective coughing
Splint affected chest wall
Block 7.0
Module 4.1
End of respiratory, part 1
Go on to respiratory, part 2
Block 7.0
Module 4.1