To Patch or Not To Patch Angela Skelton RN, BSN
advertisement
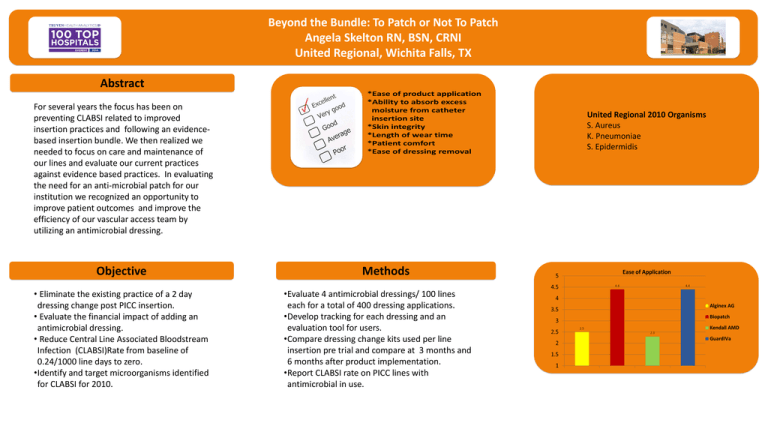
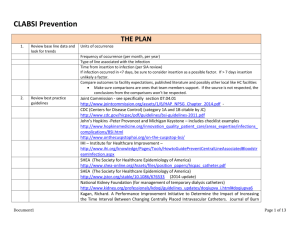
Beyond the Bundle: To Patch or Not To Patch Angela Skelton RN, BSN, CRNI United Regional, Wichita Falls, TX Abstract For several years the focus has been on preventing CLABSI related to improved insertion practices and following an evidencebased insertion bundle. We then realized we needed to focus on care and maintenance of our lines and evaluate our current practices against evidence based practices. In evaluating the need for an anti-microbial patch for our institution we recognized an opportunity to improve patient outcomes and improve the efficiency of our vascular access team by utilizing an antimicrobial dressing. Objective • Eliminate the existing practice of a 2 day dressing change post PICC insertion. • Evaluate the financial impact of adding an antimicrobial dressing. • Reduce Central Line Associated Bloodstream Infection (CLABSI)Rate from baseline of 0.24/1000 line days to zero. •Identify and target microorganisms identified for CLABSI for 2010. United Regional 2010 Organisms S. Aureus K. Pneumoniae S. Epidermidis Methods •Evaluate 4 antimicrobial dressings/ 100 lines each for a total of 400 dressing applications. •Develop tracking for each dressing and an evaluation tool for users. •Compare dressing change kits used per line insertion pre trial and compare at 3 months and 6 months after product implementation. •Report CLABSI rate on PICC lines with antimicrobial in use. Beyond the Bundle: To Patch or Not To Patch Angela Skelton RN, BSN, CRNI United Regional, Wichita Falls, TX CLA-BSI Rate (2011) House-wide – 0.22 Lines with GuardIVa - 0 Pre implementation cost prior to evaluation hemostatic patch for dressing changes: $63,012 (nursing time and supplies) annually Post implementation to adding hemostatic patch for dressing changes: $48,824 (nursing times and supplies) annually Overall savings for addition of hemostatic patch for dressing changes was estimated at: $14,188 annually Conclusions References 5 Million Live Campaign(2008). Getting started kit: Preventing central line infections how-to-guide, Cambridge Massachusetts: Institute for Healthcare Improvement; 2008. (available at. www.ihi.org) Tools for Reducing Central Line Associated Blood Stream Infections (March 2013), Agency for Healthcare Research and Quality www.ahrq.gov Infusion Nursing Society (2011) Infusion Nursing Standards of Practice Journal of Infusion Nursing 34 (1S) O’Grady NP et al (2011). CDC Guidelines for the Prevention of Intravascular Catheter-Related Infections •400 PICC line insertions and dressing changes were evaluated and the infusion staff chose GuardIVa based on their evaluation tool and overall performance. •Following GuardIVa implementation there were positive results for improved patient quality with Zero CLABSI on these vascular access devices. GuardIVa also had a positive financial impact by saving time and material utilization by saving $14,188 annually compared to the previous practice of a 2 day dressing change with sterile gauze placed at the time of insertion.