Ebert | Handout - Mount Carmel College of Nursing
advertisement

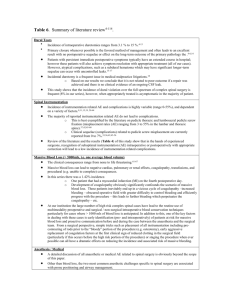
Benefits of the Use of a Cooling Blanket Postoperatively in Lumbar Spine Fusion Patients Dr. Daryl Sybert, DO, FAOAO and Kathleen Ebert RN, BSN FINDINGS/RESULTS INTRODUCTION • A two sample t-test (p=0.05) was applied to the data to determine significance • Statistical analysis shows a reduction in the time of immobility (p=0.03) and increased distance walked (p=0.001) in the experimental group • The raw sample data did reveal a decrease in the time until oxygen was discontinued, increased bowel function, and decreased length of stay for the experimental group • The data did not reveal a statistically significant reduction in narcotic usage for the experimental group • Annotated data revealed an increase in patient satisfaction in the experimental group 100% Control 90% A randomized inter-professional comparison study was conducted at Mount Carmel New Albany Surgical Hospital. The study was submitted to the IRB and approved. It was conducted from January 1, 2012 to December 31, 2012. There were a total of 502 participants (n= 502). All patients scheduled for elective lumbar spinal fusion surgery were given the opportunity to participate in the study, and informed consent was obtained. Inclusion criteria consisted of the following: 1) age 18-80, 2) delirium screen <5, 3) primary phone number for follow up, and 4) English-speaking. Participants were excluded if any of the following conditions were met: 1) an Acetaminophen drip was ordered or initiated, 2) oxygen-dependency at home, or 3) physically unable to walk due to disability not related to pain. Participants were randomly assigned to a control (n= 245) or experimental group (n=257). The control group received standard postoperative care with no cold therapy. The experimental group received standard postoperative care with cold therapy using a commercially-manufactured cooling blanket. The variables measured were as follows: 1) length of stay, 2) use of narcotics for breakthrough pain, 3) use of oxygen, 4) distance walked, 5) time of immobility, and 6) bowel function at 72 hours postoperative. The data were collected by an inter-professional staff team including nursing, case management, pharmacy, respiratory therapy and physical therapy. The collected data were then entered into a central database and subjected to statistical analysis to determine significant differences in treatment variables. 80% 70% 60% Distance (feet) METHODOLOGY Experimental 50% 40% 30% 20% 10% 0% Bowels functioning normally at 72 hours 100 95 90 85 80 75 70 65 60 55 50 45 40 35 30 25 20 15 10 5 0 70 Control 65 Control Experimental 60 Experimental 55 50 Elapsed Time (hours) The purpose of the study was to determine if any benefits can be derived from the use of a commercial cooling blanket immediately following lumbar spinal fusion surgery. Although the use of ice packs for local cooling after knee surgery has been studied in the past with mixed results there is limited research concerning their use in lumbar spinal surgery. Local cooling has also been used in exercise studies and has been shown to decrease inflammatory mediators which may cause pain and decrease physical performance. Drawing from the previous research a study was constructed to investigate the impact of cold therapy in spinal surgery. 45 40 35 30 25 20 15 10 5 0 Distance of first ambulation Time from PACU admission Time from PACU admission Time from PACU admission to first ambulation to supp. O2 to discharge from MCNA discontinuation DISCUSSION & RECOMMENDATIONS Initial findings reveal a reduction in the length of stay, decreased pain on admission, decreased length of time that oxygen was administered, and increased bowel functions from the experimental group data. There was only found to be statistical significance for the distance ambulated and time to ambulation. The results of this research have led to a change in the standard order sets for all patients undergoing lumbar spinal fusion to include the use of a commercial cooling blanket. Increased patient comfort, improved patient satisfaction, enhanced patient experience, and increased patient safety all contribute to improved patient outcomes. It is recommended that the study be repeated to further investigate the impact on use of oxygen, bowel function and length of stay. Mount Carmel IRB File # 111207-1 Expedited Approval