arterial diseases
advertisement
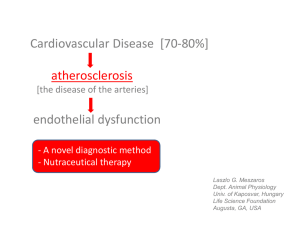
Objectives: • TO UNDERSTAND THE NATURE OF OCCLUSIVE ARTERIAL DISEASE AND ITS ASSOCIATED SYMPYOMS AND SIGNS •TO ABLE TO ASSESS ACUTE AND CHRONIC ARTERIAL INSUFFICIENCY AND KNOW TREATMENT OPTIONS. •TO KNOW ABOUT GANGRENE AND ITS MANAGEMENT •TO KNOW OTHER ARTERIAL DISEASES LIKE ANEURYSMS, ARTERITIS AND VASOSPASTIC DISEASES & AVFistula Arterial Occlusion Occlusive arterial disease Types Acute arterial occlusion Chronic arterial occlusion ACUTE ARTERIAL OCCLUSION CAUSES EMBOLIC THROMBOTIC Heart diseases-Atrial fibrillation,mural thrombus, Post MI Rheumatic valvular heart diseases Paradoxical embolism- venous thromboembolism due to patent foramen ovale Arterio- arterial embolism- dislodgement of atheromatous plaques Angiographic procedures Accidental- intraarterial injection- Ergot,thiopental Trauma. Embolism Brain-MCA Retina-Amaurosis fugax Mesenteric vessel- Spleen Kidneys Lungs-pulmonary embolism ACUTE ARTERIAL OCCLUSIONEmbolism C/F FIVE Ps PAIN PARALYSIS PALLOR PULSELESSNESS PARAESTHESIA Relation ship of symptoms to the site of obstruction Aorto-iliac obstruction Iliac obstruction Caludication in both buttocks,thighs & calves. Femoral & distal pulses absent in both limbs. Impotence.bruit over aortoiliac region. U/l claudication in thigh & calf buttocks. Bruits over iliac region Femoro-popliteal obstruction U/L absence of femoral or distal pulses. Distal obstruction U/L claudication in calf. Femoral pulse palpable with absent u/l distal pulses Femoral & Popliteal pulse palpable ankle pulses absent claudication in calf & foot Arterial Stenosis Investigations: GeneralCBC,ESR, PLASMA -fibrinogen, protein, electrophoresis, Glucose- blood n urine. Lipid profile Doppler -USG blood flow detection Duplex imaging. Echocardiography Arteriography DSA ECG Hand held Doppler COLOUR DUPLEX ARTERIOGRAM DSA Angioscope Treatment. Embolic arterial occlusion is an emergency!!! THROMBOLYSIS – Immediate -Intra Venous Heparin 5000U to prevent distal and proximal extension of thrombus. Contraindications Recent stroke Active peptic ulcer Bleeding disorders Pregnancy Hydration EMBOLECTOMY THROMBECTOMY. Fogarty catheterization- for removing proximal and distal extension of thrombus. Postoperatively- heparin and oral anticoagulation Intrarterial Thrombolysis Only if ischemia is not so severe that immediate operation is mandatory, it is possible to treat thrombus or embolus by intra arterial thrombolysis Agents-TPA-tissue plasminogen activator** Streptokinase Urokinase Identify and treat the basic cause. SFA thrombolectomy Removed thrombus Arterial Catheters Chronic Arterial Insufficiency Etiology Atherosclerosis Buerger’s disease Artritis Arterisclerosis Diabetes Risk Factors Hypertension Diabetes Strong family history Smoking Lipid abnormalities Chronic Limb Ischemia Ischemia of the lower limb may be minimal to critical Also called Chronic arterial insufficiency or Peripheral Vascular disease-PVD. Clinical presentationIntermittant Claudication-commonest complaint. Fatigue, aching or crampy pain occuring with exertion and relieved by rest, reproducible at the same distance. Claudication distance- distance at which the pain appears Rest pain Critical ischemia- severe ischemia with actual or potential tisssue loss. Signs of chronic ishemia Loss of muscle mass/bulk Loss of subcutaneous fat Skin shiny Loss of hair Brittle nails Gangrene and ulcers of foot. ??? GANGRENE Def: death, often with putrifaction of macroscopic portion of tissues. VARIETIES ACCORDING TO THE CAUSE- Secondary: Thrombus in atherosclerotic artery. ATRIAL FIBRILLATION-embolus. Arteritis from NEUROPATHY BUERGERS DISEASE RAYNAUDS DISEASE/ERGOTISM- causing arterial shutdown INTRARTERIAL INJECTIONS- thiopentone & cytotoxic materials. GANGRENE Primary: INFECTIVE- boils, carbuncles, gas gangrene, gangrene of scrotum (Fournier’s gangrene) TRAUMATIC- crush, pressure sores & constriction grooves PHYSICAL- burns, scalds,frostbite,chemical irradiation & electricity. VENOUS C/F Pulseless,painnless,funtionless, with colour change. Lacks capillary refill and venous return. Black,brown, greenish black. GANGRENE CLINICAL TYPES- DRY & MOIST DRY gangrene dessicated tissues,part becomes dry and wrinkled. Wrinkled ,discolourd from disintegration of Hb. & greasy to touch. MOISTgangrene: when venous & arterial obstruction is present, when artery is suddenly occluded by a ligature or embolus & in diabetes.. Infection & putrifaction is present. Part is swollen& discoloured. Crepitus may be present. GANGRENE SEPERATION OF GANGRENE SEPERATION BY DEMARCATION SEPERATION WITHOUT DEMARCATION. Vague DEMARCATION & skip lesions. TREATMENT OF GANGRENE GENERAL PRINCIPLES- limb saving attitude. Cardiac failure Atrial fibrillation anaemia. Nutritious diet. Control of diabetes. Analgesics. LOCAL TREATMENT dry.protection of pressure areas. Cleanniess. VARIETIES OF GANGRENE DIABETIC GANGRENE- three factors Trophic changes from peripheral neuritis. Atheroma of artries causing ischemia Excess sugar –decreases resistance to infections esp. fungal infection DIRACT TRAUMATIC GANGRENE BEDSORES-(Decubitus Ulcers) 5 factors 1. 2. 3. 4. 5. Pressure Injury Anemia Malnutrition Moisture Pressure Sore Gangrene INDIRECT TRAUMATIC GANGRENEInterference with blood vessels from pressure by a fractured bones / strangulation Thrombosis of an artery Ligation of an artery poor technique for digital anesthesia ERGOT- claviceps purpurea. Fingers,nose & ears . Seen in migrane suffers. PHYSICAL AND CHEMICAL CAUSE OF GANGRENE . FROST BITE- cold+wind. Damage to Vessel wall with transudation & edema. Pain initially later painless & gangrene TRENCH FOOT-cold+ moist+ muscular inactivity. Ill fitting boots. I/V INJECTION OF THIOPENTONE DRUG ABUSE CHEMICAL GANGRENE- carbolic acid(phenol). Frost bite ANEURYSMS ANEURYSMS- dilatation of a localised segment of the arterial system. True- all three layers involved. False- single layer of fibrinous tissue as the wall of the sac. According to the shape -fusiform -Saccular -Dissecting Eti0logy-traumatic/atherosclerotic/syphilitic/collagen disease(Marfan,syndrome), mycotic(bacterial) ANEURYSMS Symptoms- due to expansion, thrombosis, rupture or release of emboli. Symptom relate to the vessel affected, the site supplies or the tissue compressed. Clinical features Intrinsic-expansile pulsation along the course of an artery. proximal compression decreases pulsations Palpation- thrill Auscultation-bruits?? Extrinsic- neighboring or distal structures are affected. Nerve Veins Tubes-trachea ,esophagus D/D Swelling under an artery- cervical rib(subclavian) Swelling over an artery-pancreatic cyst Pulsatile tumors-sarcoma,osteoclastoma & metastsis from hypernephroma. abscess serpentine artery- innominate,carotid. ANEURYSMS Abdominal aortic aneurysm Commonest large vessel aneurysm 2% population 95% atherosclerotic 95% below the renal arteries Symptomatic/asymptomatic Symptoms-back pain, sudden – mild-sudden severe. ANEURYSMS Ruptured AAA Anterior Posterior Free bleeding into the peritoneal cavity(20%) Retroperitoneal hematoma(80%) Profound hypotension Severe pain ANEURYSMS Investigation: USG abdomen CT Chest & abdomen. AORTOGRAM ANEURYSMS Procedure Open surgical procedure Endoluminal stent graft procedure. Complications: Respiratory H’ge Colonic ischemia Renal failure Infection of the graft. Sexual dysfunction Fistula formation. Spinal cord ischemia. Peripheral aneurysms Popliteal aneurysms- most common Femoral Iliac Ascending aorta & arch AVF: Communication between an artery & vein. Congenital Acquired- trauma, penetrating wound or sharp blow, surgical for renal failure. Structural effect- arterialized veins. Dilated tortuous veins Physiological effect- Increased VR, Increased VP, Increased HRIncreased CO. PP-HIGH LVF Cardiac failure Cong Fistula- Overgrowth of limb. Persistent ulcer due to distal ischemia. ??? AVF Clinical signs: Pulsatile swelling Thrill on palpation Bruits on ausculatation Dilated veins Nicoladoni-Branham’s test- Decreased thrill, reduction in size and bradycardia on pressing the artery proximal to fistula Treatment Embolization Ligation of feeding artery??? Surgery- Separation of artery & vein ARTERITIS Thromboangitis obliterans/ Buerger’s disease Small & medium sized arteries.Occlusive disease 2. Thrombophebitis of superficial/ deep veins. 3. Raynauds syndrome, male, young patients 1. VASOSPASTIC CONDITIONS: Reynaud's syndrome: Primary/ idiopathic form. Secondary Pallor- blanching Blue- cyanosis Redness-red engorgement. Accompanied by pain. Treatment - conservative Tab. nicotinamide Secondary Reynaud's syndrome due to some other problem like-collagen disease, atherosclerosis, thoracic outlet syndrome, carpal tunnel syndrome