Intro to Shared Governance for UPC
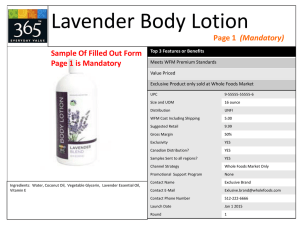
advertisement

SHARED GOVERNANCE Giving nurses a voice in their practice The System of Care: CareTouch Peer Feedback Standardized Documentation Core Values Care Teams Enhanced Communication Patient-Family Centered Care Capability Building 2 Skill Building Talent Management Leader Development Healthy Work Environments EvidenceBased Optimized Performance Shared Accountability Clinical Inquiry Centers WHAT IS SHARED GOVERNANCE? ▪ Shared Governance gives nursing team members a voice in their practice and the innovation of that practice through elected nursing practice councils at unit, facility, region, and ANC levels –Shared Governance: ▫ Creates a structure to implement practice guidelines ▫ Provides a framework for professional accountability ▫ Recognizes staff nurse's authority and responsibility for their practice ▫ Promotes nurses’ voices in their practice ▫ Improves functioning: Substantial literature and experience indicates that Shared Governance - Increases nurse engagement - Improves the working environment - Improves the quality of care provided What is Shared Governance? Shared governance means that as nursing staff, you are given ▪ A mechanism for implementing practice guidelines on your unit ▪ ▪ A voice in innovating your practice ▪ An easy pathway for sharing concerns and ideas with management Representation for bedside nurses at the executive level of the Department of Nursing ▪ Accountability for all issues elating to nursing practice ▪ Empowerment to translate ideas into actions How do we achieve it? Your unit will form a Unit Practice Council (UPC), which will include: ▪ Members representative of the unit (all positions, active duty and civilian) ▪ ▪ An election based on individuals who self-nominate for the UPC A UPC Chair, Co-Chair, Secretary, and Facility Nursing Practice Council rep GOALS OF SHARED GOVERNANCE Shared Governance provides a framework for encouraging professional accountability Goals ▪ Implement practice innovations, including clinical practice guidelines and “quick wins” supported by peer-reviewed literature and other evidence ▪ Increase nurse autonomy by giving nursing team members a voice in their daily practice and the innovation of that practice Drive and tailor ANSOC implementation, sustainment, and refinement on the unit Impact Evidence-based practice innovation, nurse autonomy, and successful ANSOC implementation that is relevant and appropriate for the unit BENEFITS OF SHARED GOVERNANCE Benefits to unit staff Benefits to facility ▪ Allows innovations to get visibility and support from facility-level ▪ ▪ leadership Shares ideas across units Helps leadership identify when unit struggles actually have a system-wide basis, and helps proactively address these ▪ Results in significant improvement in nurse engagement ▪ ▪ ▪ ▪ – Increases satisfaction with the work environment – Improves nurse perception of autonomy Results in lower nurse turnover (documented rates of <10%) Decreases nurse absenteeism (documented rates of 0-5%) A part of achieving Magnet status; part of Pathways to Excellence Widely adopted among top nursing practices and best-in-class healthcare facilities Benefits described by peer-reviewed literature listed in the Appendix HOW THE UPC AND CNOIC/NCOIC WILL WORK TOGETHER – CNOIC/NCOIC will turn to UPC as “decider” on key practicerelated issues within their primary scope – CNOIC.NCOIC will “concur” or in rare cases, veto (see slide 10) – UPC will need guidance from CNOIC/NCOIC for both practicerelated issues and ANSOC implementation: ▫ Practice-related issues: UPC will want input on quick wins and practice innovations, including ideas for both, feasibility, priority and required next steps ▫ ANSOC implementation: UPC will need consultation on tailoring of ANSOC components ACCOUNTABILITIES FOR SHARED DECISION-MAKING Clinical Practice Accountabilities • Standards of Practice • Specialty and related • Clinical competency • Care Delivery Model Shared • Professional Development Decision• Orientation Making • Continuing education • Certification • Advanced degrees • Quality • EBNP • Research • Outcomes • Peer Review • Interdisciplinary Relationships Management Accountabilities • Resources/Allocation • Human • Fiscal • Material • Structure • System/Organizational Links • Reward and Recognition (from continual performance evaluation) EXAMPLES OF HOW OTHER UNITS HAVE IMPLEMENTED SHARED GOVERNANCE (1 OF 3) Preventing infection Streamlining a procedure Setting a name tag trend ▪ An Inpatient Med/Surg UPC ▪ Combined surgical suite UPC ▪ Another inpatient Med/Surg identified several issues with wearing ACUs on the floor: – The long sleeves had significant potential to act as a vector for germs – The need to wash the ACUs daily was quickly wearing them out, and they were expensive to replace ▪ The UPC’s proposal to their CNOIC recommended the use of short-sleeve scrubs for military nurses and provided evidence that the proposed change would both reduce the chance of spreading infections and the cost of uniforms ▪ Due to the UPC’s evidencebased recommendation, the uniform was changed to optional scrubs for all nurses on the unit brought voices of nurses from separate but highly interlinked groups together for the first time ▪ Suggestion from OR nurses requested that the pre-op nurses put on a specific type of immobilization before anesthesia ▪ The UPC immediately worked to ensure that pre-op nurses could change a simple procedure to make OR nurses’ jobs easier UPC heard that patients were confused about the roles of the various nursing team members ▪ The UPC proposed an initiative to have name tags with nurse roles on them ▪ The tags were a hit and spread to the doctors in the unit, and from there were adopted around the facility because of their popularity EXAMPLES OF HOW OTHER UNITS HAVE IMPLEMENTED SHARED GOVERNANCE (2 OF 3) Hand hygiene ▪ The nursing team of an adult ▪ ▪ ▪ ▪ medicine clinic noticed that patients did not wash their hands frequently when at the hospital The UPC brainstormed ways to effectively increase hand hygiene The UPC proposed mounting Purell dispensers in the hallways to encourage everyone to have better hand hygiene The UPC’s recommendation is in line with evidence on infection control and frequency of use with different kinds of hand hygiene The CNOIC accepted the proposal and dispensers were mounted on the walls Streamlining a procedure ▪ A Hem/Onc clinic and an inpatient ▪ ▪ ▪ ▪ unit wanted to optimize their coordination of care They identified three areas to improve: communicating more often, communicating more effectively, and becoming more familiar with the other unit’s operations The clinic staff began providing a patients’ last lab, pharmacy flow sheets, and oncologist note to the inpatient nursing team The inpatient unit’s Lead RNs began calling down to the Hem/Onc clinic to speak with their patient’s team to ensure that the inpatient plan of care was congruent with the outpatient plan of care The UPCs invited each other to various events (e.g., BBQ, “after hours” event) to increase collegiality between the units Surgical tours ▪ An OR unit and a PACU ▪ ▪ ▪ realized that patients and their families got very anxious before a surgery To reduce their patients’ anxiety, the UPCs collaborated to hold a monthly surgery tour where the patients and their families could get familiar with the rooms and what would happen during care This allowed patients and their families to better plan for the surgery and recovery; it also laid the groundwork for a culture of trust and communication between the patients, families, and staff The concept was so successful and popular that the PAO did an article on the concept EXAMPLES OF HOW OTHER UNITS HAVE IMPLEMENTED SHARED GOVERNANCE (3 OF 3) Fall prevention ▪ Two inpatient med/surg units wanted to prevent falls ▪ Their UPCs decided to have a ▪ ▪ ▪ ▪ competition for who could go longer without any falls The units put up posters indicating the number of days since their last fall Each reviewed best practices on falls prevention and instituted the methods they felt would help their unit most Falls decreased dramatically over the months of the competition and stayed low The staff became actively and creatively engaged in preventing falls through friendly competition Streamlining a procedure ▪ A GI unit and PACU at a ▪ ▪ ▪ MEDCEN wanted to optimize their coordination of care The units had a good record of communication and wanted to ensure this trend continued The units modified an existing documentation form to accurately reflect changes in their practice, familiarized staff through inservices, and monitored compliance through chart audits In addition, the units set three goals: – GI staff would perform accurate and complete bed side hand-off communication to PACU staff – PACU discharge criteria would be met prior to initiation of report call to the GI unit – PACU staff would call report to a licensed GI staff member prior to release from PACU Minimizing need for ABGs ▪ The adult critical care and ▪ ▪ ▪ respiratory care units identified that new clinical guidelines called for use of PetCO2 (capnography) in several new patient populations The nursing staff developed a recommendation to routinely use PetCO2 monitoring on patients receiving moderate sedation and those at risk for respiratory compromise, in addition to intubated patients (who already were routinely monitored with PetCO2) The nursing staff engaged their leadership, CNS, providers, and respiratory therapists to properly implement the change and track its impact (e.g., reduction in ABGs) They instituted hands-on training with a goal of making PetCO2 monitoring part of their daily best practice ESTABLISHING REPRESENTATIVE UPCS ▪ Guidelines ▪ ▪ ▪ Representation – The ratio of nursing roles on the UPC should mimic that of the unit (i.e., % of RNs, LPNs, CNAs, civilian, and military staff on UPC is reflective of mix on the unit) – Each member has a constituency they talk to before each meeting and update after – Constituencies may be assigned, based on who elected them, or based on another model Nomination – Individuals can self-nominate or be nominated by others – In small units, everyone may be on the ballot automatically unless they opt out Size – Ideal size of UPC is 5-15 members; each member should have ~4-7 constituents – Some units may combine to form a council Terms – UPC members serve 1-2 years before re-election Lessons Learned – Members in good standing can be reelected ▪ Representatives must be able to update all – Members roll on and off at different times for their constituents personally – therefore continuity and institutional memory representatives should have no more than – Limiting number of consecutive terms to two seven constituents can help most of the staff to serve over the ▪ At Tripler, some UPCs decided all elections years, facilitating buy-in would be in January of every year; what – Election rhythm: they found was that the new UPC was all ▫ If a UPC decides on 1 year terms, half the new members and no one knew how to run positions are up for re-election every 6 months the meeting or what had been done before. ▫ If a UPC decides on 2 year terms, half the When they staggered elections, new positions are up for re-election every 12 members learned from their predecessors months QUICK WINS Quick wins should be… For each quick win, identify… ▪ ▪ ▪ The goal/proposal ▪ Data supporting that the goal is a good one ▪ Data suggesting that this is the appropriate method to address the goal ▪ Steps required to get to that goal ▪ ▪ ▪ ▪ Something everyone can get excited about Concrete, easy to put your hands on Rapidly accomplishable Non-controversial Able to make a daily difference Recommendation Focus on only 1-2 quick wins at a time The rationale and reasons for the goal – Who you need to win over – What information you need to collect ▪ Possible challenges and ways to address those challenges ▪ ▪ ▪ Backup option/goal Leader(s) who will own the proposal Resources the leader(s) can use UPC COLLABORATION WITH OTHER GROUPS ▪ The UPC works with other people and groups at both the unit and facility levels – CNOIC/NCOIC: The UPC identifies and prioritizes quick wins and long term goals and ANSOC tailoring in conjunction with the CNOIC/NCOIC – Unit nursing team: A “project board” and/or website are updated every meeting and track outcomes of UPC projects for all to see – Guests: The UPC invites guests to sit in on meetings as relevant for problem solving, e.g., pharmacy, hospital services – Facility NPC: ▫ UPCs each elect a representative to the Facility NPC ▫ UPCs present updates and innovations to Facility NPC monthly ▪ Autonomy of the UPC – Each UPC is self-governing, e.g., deciding for itself how it will conduct meetings and breaks, schedule rooms, develop norms under its charter etc – UPCs must still work within unit norms and with the CNOIC/NCOIC Guidelines Lessons Learned Some CNOIC/NCOICs were concerned that they might not know what changes were happening in the unit or be able to share key insights, so the Facility NPC developed a set of guidelines for all UPCs to ensure that CNOIC/NCOICs kept informed of progress and had clear channels for providing input and feedback : EXPECTATIONS FOR UPC ATTENDANCE AND ROLES Guidelines ▪ Attendance – Each UPC representative is required to attend each meeting. Staff are not scheduled on the floor during meetings. Missing meetings requires an official excuse (must have annual, military, or sick leave) – The charter should specify how to deal with members who miss meetings repeatedly ▪ Roles – There is a Chair, Co-chair and a Secretary ▫ The Chair, Co-chair and Coach solidify the agendas and meet with the CNOIC/NCOIC before each meeting ▫ The Secretary takes and publically posts minutes and keeps the UPC on track for due-outs – These roles are decided at the first meeting Lessons Learned One facility found that if all their UPCs met on a single day each month, it was easier to predict, schedule for, and reserve rooms. Attendance was boosted by holding all the meetings on one day; For other facilities, covering the ward with so many nurses out or finding rooms for all UPCs may be hard RESOURCING UPCS Guidelines ▪ Time: – Dedicated time for introducing nursing team to UPC and training those ▪ involved with the UPC – Dedicated time for members to attend meetings ▫ Early in the process: In order to get traction against the issues required for the first months UPCs will likely need to meet for 2 hours once or twice weekly ▫ Steady state: UPCs will meet for ~1 hour monthly1 ▫ Members should not be pulled away during meetings – Dedicated time for Coaches to prepare for meetings, attend and coach – Dedicated time for Unit Shared Governance Leader/UPC Chair for training and pushing forward initiatives Materials: Lessons Learned – UPCs need access to: One facility found that using a meeting space in a different part of the facility, away from the ▫ Bulletin board unit, increased the efficiency of meetings ▫ Room for meetings because it reduced distractions and the number ▫ Other materials, e.g.: of times the UPC members were interrupted - Email with issues on the floor - Poster supplies - Access to AKO 1 Some UPCs may meet 2 hours per month or arrange time in other fashions WILL THE UPC BE REQUIRED TO MAKE TOUGH DECISIONS? ▪ Unit members will bring issues and recommended solutions to their UPC ▪ The UPC will not make decisions in a vacuum – they will receive input and guidance from unit leaders, the Facility NPC, and others as appropriate ▪ The UPC will develop evidence-based recommendations/proposals to give to unit leadership and staff ▪ Everyone will be a part of the decision making process HOW WILL MY VOICE BE HEARD IF I’M NOT ON THE UPC? ▪ Every staff member on your unit will be assigned a member of the UPC as their rep (most UPC members will be the rep for 4-6 constituents) ▪ Each UPC member is responsible for keeping their constituents updated on the issues being discussed by the UPC and getting their feedback ▪ UPC members should have face-to-face contact with their constituents before and after each meeting WHAT’S THE DECISION-MAKING PROCESS FOR THE UPC? ▪ The UPC will decide how it makes decisions and recommendations – either through consensus or voting or both ▪ When making decisions, each UPC member will provide their recommendation based on the input of their constituents ▪ Additionally, the UPC will take into account any guidance unit leadership may have provided ▪ Do not take it personally if your recommendation is not the final outcome –everyone has the opportunity to let their voices be heard, and the UPC will make the decision they believe is best for the entire unit ▪ The UPC also has the ability to try a course of action, then go back to re-evaluate and change directions based on results and continued feedback WILL THE UPC WILL COME UP WITH IDEAS THAT WILL CHANGE LONG TIME ROUTINES? ▪ The short answer is “Yes” ▪ The UPC is designed to be an avenue for evidence-based practice innovation within the unit, so it is quite possible that it will come up with ideas that may change long time routines ▪ Decisions will be made based on current research and clinical evidence, clinical practice guidelines, best practices, etc. ▪ All changes should be driven by the goals of enhancing the quality of nursing care, improving patient outcomes, satisfaction, and/or experience, and creating a healthy work environment for our team WILL YOUNG NURSES CHANGE THINGS WITHOUT THE BENEFIT OF EXPERIENCE? ▪ It is critical that the UPC membership is representative of all staff members on the unit, including both experienced and less-experienced nursing staff ▪ Whether the experienced staff are UPC members or constituents, everyone has an equal voice through their UPC rep and the insight of experience from long time staff will be taken into consideration ▪ Young nurses are also helpful to have on the UPC because they are often closest to recent updates to nursing practice and can bring a fresh perspective and enthusiasm to the work area ▪ All UPC decisions are made after consulting all members of the unit and considering everyone’s ideas and perspectives WILL MILITARY CONCERNS WILL TRUMP CIVILIAN CONCERNS? ▪ Every staff member (military or civilian) has an equal voice on the UPC ▪ Both military and civilian nurses have particular constraints and interests that should be considered equally in any decision-making process ▪ However, UPCs have some limits on the recommendations/decisions they can make – there may be some issues more appropriately addressed by unit leadership ▪ The UPC Chair and Co-chair can work with their UPC Coach and unit leadership to identify those concerns best dealt with through the UPC and those that should fall under the purview of the unit’s chain of command WITH THE RANK STRUCTURE OF THE MILITARY, WILL SOME UPC MEMBERS BE INTIMIDATED IN LETTING THEIR VOICES BE HEARD? ▪ Within a UPC, EVERYONE has an equal voice regardless of rank, experience, or education level ▪ There should be a representative of almost all staff types within your work environment (RN, LPN, NA, medic, clerk, tech), as well as a mix of civilian and military WHAT IS THE ROLE OF THE CNOIC AND NCOIC IN THE UPC? ▪ Unit leadership has a significant role in unit Shared Governance, including to: – Provide vision, guidance, coaching and support for your UPC – Provide protected time for your UPC to meet – Maintain dialogue with the UPC while empowering them to – come up with recommendations enhancing the quality of nursing care, improving patient outcomes, satisfaction, and/or experience, and creating a healthy work environment for the team Give the UPC opportunities to update staff during staff meetings ▪ It may be helpful for unit leadership to join the UPC meeting (preferably toward the end of the meeting) so that the UPC can provide updates, ask questions, and get unit leadership guidance and feedback AS THE CNOIC / NCOIC, WHAT SAY WILL I HAVE IN THE DECISIONS BROUGHT FORTH BY THE UPC? ▪ Your roles as the leaders of the unit are unchanged ▪ You provide the vision, guidance, and parameters for the UPC ▪ ▪ ▪ to move forward on ideas and projects Your leadership challenge is to identify ways to collaborate with the UPC and give them as much responsibility as possible while still maintaining proper command and control – this will take some work by both the unit leadership and the UPC to figure out a process that works for the team The UPC has the authority to come up with ideas, do the research related to those ideas, and formulate recommendations Depending on the topic, the UPC must then go back to unit leadership and/their constituents for final authorization or to get the issue elevated to a higher level (for example, the Facility NPC) I FEEL THE UPC HAS TO DO WHAT I SAY BECAUSE I AM THE BOSS. IT THAT RIGHT UNDER THIS MODEL? ▪ The whole point of shared governance is to empower staff ▪ ▪ ▪ members to become part of the solution, so they feel like their voice is being heard and they are invested in the success of the unit (this is a change in philosophy from the previous way that the Army has practiced) The UPC should have the freedom to brainstorm evidencebased solutions to issues that enhance the quality of nursing care, improve patient outcomes, satisfaction, and/or experience, and create a health work environment for the team (see scope of focus) Unit leadership should work collaboratively to implement those solutions that make sense and coach the UPC on how to improve/refine recommendations that are not feasible as submitted When possible, unit leaders should include their UPC in solution development – it can actually significantly reduce leadership workload