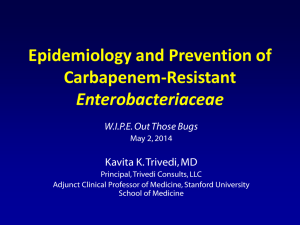
Update on Carbapenem Resistant Enterobacteriaceae
advertisement
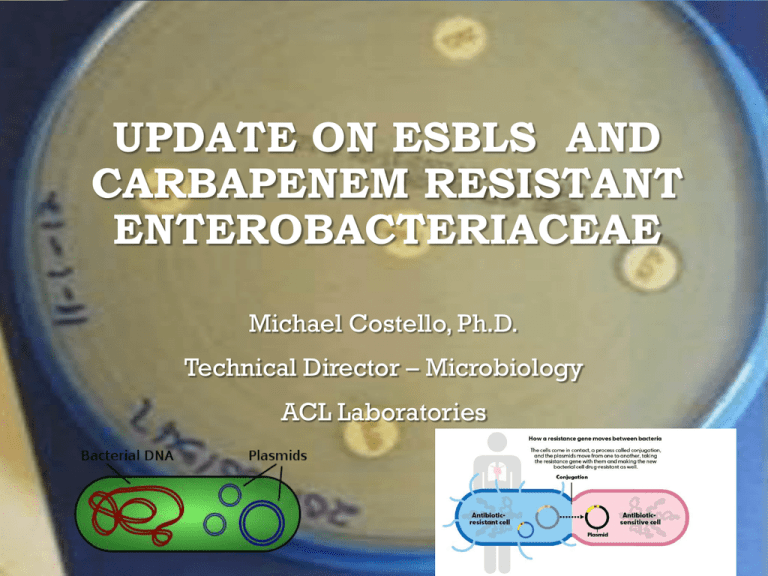
UPDATE ON ESBLS AND CARBAPENEM RESISTANT ENTEROBACTERIACEAE Michael Costello, Ph.D. Technical Director – Microbiology ACL Laboratories TOPICS TO COVER • Extended spectrum β lactamases (ESBLs) • Update on the recent changing patterns of different types of ESBLs in the Chicago/Milwaukee area • Implications • Healthcare associated infections (HAI) Vs. community acquired infections • Carbapenemases – more than “just” KPC • Summarize carbapenemases currently found in the Wisconsin/Illinois area • Expand on how and why CREs have spread so rapidly throughout the world. • Define testing algorithms for rapid detection of CRE, faster the better • Talk about new molecular based tests that are becoming available • Molecular assays for identification of bacteria and resistance genes directly from a positive blood culture bottle. • Culture not required ANTIBIOTIC RESISTANCE • Gram Negatives • Production of β-lactamases – Enzymatic destruction of antibiotic • Switch from Tem and SHV to CTX-M • Permeability alterations • Porin mutations – antibiotic entry is limited • Porins are barrel shaped proteins that cross cell membranes and act as a port though which nutrients, toxins and antibiotics can diffuse • Antibiotic extrusion by efflux pumps • Rapidly pump out antibiotics before they are effective • Rarely, PBP alterations • PBP 7-8 in A. baumanii • Combinations of the above CHANGING ESBL PATTERNS OUT WITH THE OLD (TEM, SHV) AND IN WITH THE NEW [ESBL (CTX-M), CARBAPENEMASES (KPC, NDM-1)] Target is still the same – β-lactam ring Only difference between peniclliniases, cephalosporinases and carbapenemases is the preferred substrate CLASSIFICATION OF ß-LACTAMASES BUSH-JACOBYMEDERIOS - FUNCTIONAL CLASSIFICATION Group Enzyme Type Inhibition by Clavulanate Molecular Class (Ambler) # of Enzymes Characteristics Example 1 Cephalosporinase No C 53 Mainly chromosomal located in gram negative bacteria, but may be plasmid mediated. Resistance to ß-lactams (except carbapenems) E. Coli 2a Penicillins Yes A 20 Narrow spectrum resistance to penicillins only S. Aureus 2b Broad spectrum Yes A 16 Broad spectrum penicillinases TEM-1, SHV-1 2be Extended spectrum Yes A 38 ESBL conferring resistance to oxyiminocephalsporins and monobactams TEM-3, SHV-2, CTX-M 2br Inhibitory resistant Partly A 9 Inhibitor resistant ß-lactamases (mostly TEMtypes and to a lesser extent SHV derived ESBL TEM-30, TRC-1 2c Carbenicillinase Yes A 15 Carbenicillinases BRO-1, CARB3, PSE-1 2d Cloxacillinase Variable D or A 18 Oxacillinases, partly inhibited by clavulanate OXA-1, PSE-2 2e Cephalosporinase Yes A 19 Oxacillinases, inhibited by clavulanate P. vulgaris, Bacteroides fragilis 2f Carbapenemase Yes A 3 Serine active carbepemases, inhibited by clavulanate. E. cloacae, 3 Metalloenzyme No B 15 Metallo-ß-lactamases conferring resistance to all ß-lactam drugs except monobactams aztreonam S. maltophilia 4 Penicillins No 7 Miscellaneous ß-lactamases that do not conform to other groups B. cepacia ESBL Pandemics Enterobacteriaceae pan-resistance endemic pAmpC detected KPC detected NDM detected. ESBL (EXTENDED SPECTRUM Β-LACTAMASE) OUT WITH THE OLD AND IN WITH THE NEW! • Old ESBLs - SHV (SulfHydryl Variable) and TEM (Temoneira) • >120 variants • TEM and SHV-1 (initially only hydrolyzed ampicillin) first described in 1960’s • First ESBLs • SHV-2 in 1983 • TEM-3 in 1984 • TEM and SHV are primarily healthcare associated • Competitive disadvantage outside of a healthcare setting • Require administration of antibiotics to compete • More reactive against ceftazidime than cefotaxime • Rarely carbapenem resistant • New ESBLs – CTX-M (CefoTaXime –Munich) • First described in Japan in 1986 and named in Germany in 1989. • Can show carbapenem resistance, especially in association with a porin mutation CTX-M • CTX-M -lactamases are extended-spectrum β-lactamases (ESBLs) that mainly inactivate cefotaxime and cefriaxone and have less activity against ceftazidime • Sequencing evidence that gene mobilized from Kluyvera spp. (environmental bacteria rarely associated with disease) • Associated with community-acquired UTIs • Highest incidence in E. coli • Plasmid is stable and confers minimal competitive disadvantage when β-lactams are not present • Dramatic world-wide spread in the last decade • Quickly replacing TEM- and SHV-type ESBLs • Detected in both humans and animals (in the food chain) • Present wherever β-lactam antibiotics are used • Associated with other multidrug-resistant genes • Found on plasmids that also include resistance genes to aminoglycosides and fluoroquinolones ANTIBIOGRAMS 2008 - NEW MORE AGGRESSIVE E. COLI STRAIN ESBL POSITIVE ANTIBIOGRAMS Ertapenem Imipenem (%S) Nitrofurantoin (%S) Piperacillin/tazobactam (%S) Tobramycin (%S) Trimethoprim/sulfamethox. (%S) 100 100 80 88 40 37 100 100 88 94 39 39 97 72 77 40 46 100 100 78 96 36 68 51 100 100 89 74 25 32 52 100 100 83 90 30 57 Escherichia coli, ESBL (6%) 205 92 0 11 0 0 0 0 0 2 67 Bethany Escherichia coli, ESBL (40%) 29 100 0 0 0 0 0 0 0 3 68 Good Sam Escherichia coli, ESBL (2%) 43 100 0 12 0 0 0 0 0 14 92 GSH Escherichia coli, ESBL (2%) 18 100 0 0 0 0 0 0 0 0 78 SSUB Escherichia coli, ESBL (4%) 35 100 0 20 0 0 0 0 0 3 54 Trinity Escherichia coli, ESBL (2%) 25 92 0 16 0 0 0 0 0 0 48 IMMC Escherichia coli, ESBL (6%) 74 93 0 7 0 0 0 0 0 12 LGH Escherichia coli, ESBL (8%) 190 96 0 1 0 0 0 0 0 6 Hospital Gentamicin (%S) 46 Ciprofloxacin (%S) 21 Cefepime (%S) 66 Ceftriaxone (%S) 93 Ceftazidime (%S) 100 Cefazolin (%S) 53 Aztreonam (%S) 37 Ampicillin/sulbactam (%S) 85 Ampicillin (%S) 84 Amikacin (%S) 100 # Isolates 100 CMC E. coli ESBL Isolates Total = 619 Gram Negative Unusual resistance pattern 1. ESBL 2. Aminoglycoside resistance 1. Tobramycin more resistant than Gentamicin 3. Flouroquinolone resistance Cipro = Levo UROPATHOGENIC E. COLI ST131 MULTIPLE RESISTANCE GENES AND VIRULENCE FACTORS - ALL COMMUNITY ACQUIRED Multiple genes International Journal of Antimicrobial Agents, accepted for publication 201 CTX-M SUMMARY Uropathogenic E. coli clone ST131 from phylogenetic group B2 that have plasmids that produce multiple resistance factors • CTX-M-15 or CTX-M-14 • CTX-M-15 is also resistant to Ceftazidime • Different epidemiology – multidrug resistant community onset UTIs • AAC (6’)-lb-cr aminoglycoside/fluoroquinolone acetyltransferase (ACC (6’)-Ib responsible for resistance to kanamycin, tobramycin and amikacin. ACC (6’)-Ib-cr also confers resistance to ciprofloxicin and norfloxicin) • Aminoglycoside modifying enzyme that can also cause quinolone resistance, esp. in norfloxicin and ciprofloxicin (also see resistance to levofloxicin) Common cause of UTIs in the Chicago area by ESBL-producing E. coli. Bacteria with multiple resistance genes becoming widespread AMPC DETECTION – DIFFERENTIATE FROM CARBPENEMASE PRODUCERS AMPC • Chromosomal = MY SPACE bugs • (Morgenella, Y. enterocolitica, Serratia, Providencia, Aeromonas, Citrobacter, Enterobacter) • Inducible = Any MYSPACE containing AmpC plasmid • Organism may develop resistance during prolonged therapy with 3rd generation cephalosporins. • Identified in organisms exhibiting the following: • Resistant to cephamycins • Cefoxitin and Cefotetan • Resistant to penicillin – β-lactam inhibitors • Sensitive to cefepime and carbapenems • Hyperproduction = Any Enterobacteriaceae • Caused by a mutation in the AmpC regulator gene leading to permanent (?) hyperproduction or derepression. • Increased AmpC production and proin mutation can result in carbapenem resistance PAMPC • AmpC enzymes in the midwest • C. freundii cluster • CMY-2 • Enterobacter cluster • MIR-1, ACT-1 • M. morganii cluster** • DHA-1 • plasmid-encoded inducible cephalosporinase , other plasmid-encoded AmpC enzymes are almost always expressed constitutively • H. alvei cluster • ACC-1 • Aeromonas cluster • CMY-1 and FOX-1 DETECTION OF AMPC HYPERPRODUCER Cephamycin – inducible AmpC Inducible AmpC Cefotetan + cloxacillin Cefotetan Hyperproduction of AmpC > 3 mm difference Hyperpoduction associated with a mutation Of the AmpC regulator gene. Cephalosporinase not regulated and AmpC produced at higher levels Meropenem + Cloxacillin Meropenem + Boronic acid Meropenem AMPC + PORIN LOSS = CARBAPENEM RESISTANCE Porins - Protein channels through bacterial membrane allow for exchange of water, ions, glucos and other nutrients as well as waste products AMPC SUMMARY • Gene can be found on plasmids • No longer restricted to MYSPACE bacteria • Morgenella, Y. enterocolitica, Serratia, Providencia, Aeromonas, Citrobacter, Enterobacter • Different AmpC genes with differing ranges • DHA-1 can hydrolyze carbapenems • Carbapenem resistance usually requires overexpression of AmpC (mutation in the regulator gene) and the presence of a porin mutation, restricting migration of antibiotic into the bacteria Carbapenem-Resistant Enterobacteriaceae (CRE) Meropenem Imipenem Doripenem Ertapenem CARBAPENEMASES THE RISE OF CARBAPENEMASES WHY ARE PLASMID CRE’S A PUBLIC HEALTH EMERGENCY • Limited treatment options for life threatening infections • Co-migrate with other resistance genes • Resistant mechanisms have transferred to plasmids • Plasmids easily spread to other bacterial species • No/few new drugs/drug classes • Rapid detection and effective infection control measures are essential to control spread IPDH NEW RULE - REPORTING CARBAPENEMASES • Major points: • This establishes the mechanism by which carbapenem-resistant Enterobacteriaceae (CRE) are reported to IDPH, starting Sept 1, 2013, for all Illinois healthcare facilities • Beginning September 1, 2013, reporting facilities shall report carbapenem-resistant enterobacteriaceae (e.g., E. coli, Klebsiella species, Enterobacter species, Proteus species, Citrobacter species, Serratia species, Morganella species, or Providentia species) based on laboratory test results • Laboratory tests • Molecular tests (PCR specific for carbapeneamse) • • KPC PCR currently offered at Rosemont Phenotypic test (Modified Hodge Test) specific for carbapeneamse production • Rosemont offers modified Hodge Test and ROSCO Disks – identification of KPC, MBL, hyper AmpC, and Oxa-48 carbapenemases • • E . coli and Klebsiella species only: nonsusceptible to one of the following carbapenems: doripenem, meropenem, or imipenem and resistant to the following 3rd generation cephalosporins: ceftriaxone, cefotaxime, and ceftazidime • • Phenotypic tests are too slow! We use this definition for all Enterobacteriaceae The rationale to use a registry mechanism for reporting, versus the traditional INEDSS, is to allow the database to serve as an inter-facility information exchange for patient-related CRE status. For example, a hospital IP can query the database to see if a newly admitted patient has a history of CRE. Querying is restricted to IDPH-registered personnel with login access to the XDRO registry . WHY ARE CRES SO IMPORTANT? • Invasive infections (e.g., bloodstream infections) with CRE are associated with mortality rates exceeding 40% • Carbapenem-resistant strains frequently possess additional resistance mechanisms that render them resistant to most available antimicrobials • CRE can spread rapidly in health-care settings • Enterobacteriaceae are a common cause of community infections, and CRE have the potential to move from their current niche among health-care–exposed patients into the community MMWR March 8, 2013 / 62(09);165-170 Number of Subjects 100 80 60 * * CRKP * * CSKP * p <0.001 40 20 0 From: CDC webcast 3/19/09 IDENTIFICATION OF CARBAPENEMASES FOUND IN THE CHICAGO/MILWAUKEE AREA Carbapenemase Hydrolysis Profilea Inhibition Profileb Molecular Class Functional Group Enzyme A 2f NMC-A Penicillins Early Cephalosporins Extended Spectrum Cephalosporins Aztreonam EDTA/ DPA Clavulanic Acid Boronic Acid Cloxacillin Temocilin + + -/+ + - + - - +/- + + -/+ + - + - - +/- + + + + - +/- + - +/- IMI# + + +/- + - + - - - GES^ + + + - - + - + + + - + - - - +/- + + -/+ - - -/+ - - + (chromosomal) SME (chromosomal) KPC (plasmid) (chromosomal) (plasmid, low carbapenemase - activity) B1 3 NDM, IMP, VIM, GIM, SPM (most plasmid) D # 2d OXA-48 (plasmid)? Selective increased resistance to imipenem Sensitive to AZT; clavulanic Acid +, Boronic Acid and EDTA – a Hydrolysis Symbols: - +, strong hydrolysis; +/-, weak hydrolysis; -, no measureable hydrolysis b Inhibition Symbols: +, inhibition; +/-, variable inhibition among β-lactam family members; -, no inhibition NMC-A = Not MetalloCarbapenease A; SME = Serratia marcescens Enzyme; KPC = Klebsiella pneumoniae carbapenemase; IMI = imipenem hydrolyzing β-lactamase; GES = Guiana Extended Spectrum β-lactamase; NDM = New Delhi Metallo carbapenemase; IMP = active on imipenem ; VIM = Verona Integron-encoded Metallo-β-lactamase; GIM = German Imipenemase; SPM = Sao Paulo Metallo-β-lactamase; DPA = dipicolinic acid (Metallo β-lactamase inhibitor); Boronic Acid (KPC and AmpC inhibitor); Cloxacillin (AmpC inhibitor) ^ CRES DETECTED IN CHICAGO/MILWAUKEE AREA CRE Type Year Detected Chromosomal or Plasmid Bacteria SME 2005 Chromosomal Serratia marcescens NMC-A 2004 Chromosomal Enterobacter spp. KPC 2009 Plasmid Enterobacteriaceae NDM-1 2010 Plasmid K. pneumoniae, E. coli OXA-48 2012? Plasmid Screening started 2013 VIM, IMP 2010? Chromosomal/plasmid Screening started 2009 Carbapenem Breakpoints Lowered 9/2012 EFFECTS OF LOWERING CARBAPENEM BREAKPOINTS • Detect chromosomal carbapenemases that are not considered an infection control emergency • More SME (Serratia Marcescens Enzyme) • Carbapenems resistant and 3rd and 4th generation cephalosporins sensitive • More NMC-A (Not Metallo Carbapenemase, in Enterobacter sp.) • Carbapenems resistant and 3rd and 4th generation cephalosporins sensitive Acute care hospital Long term Care facilities Need to break the cycle! ADVOCATE HOSPITALS – K. PNEUMONIAE IMIPENEM (% SENSITIVE) Hosp. 2007 2008 2009 2010 2011 2012 100 96 94 92 93 92 Condell - - - 99 99 99 G. Sam 100 100 99 98 95 96 G. Shep 100 100 100 96 98 97 IMMC 100 98 92 91 92 92 LGH 100 98 95 91 92 92 SSUB 100 97 94 94 90 90 Trinity 100 97 94 94 93 92 CMC VITAL SIGNS: CARBAPENEMRESISTANT ENTEROBACTERIACEAE • Enterobacteriaceae are gram-negative bacteria that can cause invasive disease but generally have been susceptible to a variety of antibiotics. • Carbapenem-Resistant Enterobacteriaceae (CRE) are Enterobacteriaceae that have become highly resistant to most or all antibiotics through several mechanisms. Carbapenem resistance, while relatively uncommon among Enterobacteriaceae (4% of Enterobacteriaceae in this study), has increased from about 1% during the past decade. CRE bloodstream infections are associated with mortality rates approaching 50%. MMWR March 8, 2013 / 62(09);165-170 VITAL SIGNS: CARBAPENEMRESISTANT ENTEROBACTERIACEAE • CRE has now spread throughout the United States but in most areas they remain relatively uncommon; about 4% of acute-care hospitals and 18% of long-term acute-care hospitals reported at least one CRE to the National Healthcare Safety Network in the first 6 months of 2012. Nearly all patients with CRE were currently or recently treated in a health-care setting. However, CRE could spread into the community among otherwise healthy persons MMWR March 8, 2013 / 62(09);165-17 VITAL SIGNS: CARBAPENEMRESISTANT ENTEROBACTERIACEAE • Preventing spread is important before CRE gains a foothold in more hospitals or in the community. This requires active (rapid) case detection and contact precautions for colonized or infected patients as well as cohorting of patients and staff; appropriate antibiotic use in all settings; and communication about infections when patients transfer. Regional and state-based approaches have been shown to be effective in reducing incidence. • Additional information is available atMarch 8, 2013 / 62(09);165-17 MMWR http://www.cdc.gov/vitalsigns MECHANISMS OF CARBAPENEM RESISTANCE • Non enzymatic • Modifications of outer membrane permeability • Porin loss • Allow passage molecules include water, ions, glucose, and other nutrients as well as waste products • Up regulation of efflux systems • Enzymatic • Production of carbapenem hydrolyzing β-lactamases • hyperproduction of AmpC β-lactamases • Certain ESBLs with increased capacity to hydrolyze carbapenems • CTX-M • Production of carbapenemases • KPC, NDM-1, others • Combinations of all of the above NEED TO DISTINGUISH MECHANISMS OF CARBAPENEM RESISTANCE – WHY? • KPC (increasing numbers) • Make all penicillins, cephalosporins, inhibitor combinations, aztreonam, and carbapenems resistant • Hyper AmpC (most common) • Make all penicillins, cephalosporins, inhibitor combinations, and aztreonam Resistant • Cefepime may still be effective • Do not change carbapenem interpretations • Metallo β-lactamases (rare, but increasing) • Same as KPC, except do not change aztreonam interpretation • Other carbapenemases • Antibiotic profiles not clear • 1st described in 1998, 2001 in NYC • Now endemic in the Northeastern/Mid-Atlantic region of the United States • surveillance cultures of hospitals in the New York City area reporting rates of carbapenem resistance in K. pneumoniae isolates ranging up to 40% • Reported in Europe, China, Central America, South America – Since 1998 • Also reported in Pseudomonas aeruginosa (Columbia) • KPC is a class A b-lactamase (serine residue at the active site) • Confers resistance to all b-lactams including extendedspectrum cephalosporins and carbapenems • Occurs in other Enterobacteriaceae • Most commonly seen in Kliebsiella pneumoniae • Also reported in: K. oxytoca, Citrobacter freundii, Enterobacter spp., Escherichia coli, Salmonella spp., Serratia spp., CARBAPENEM RESISTANT ENTEROBACTERIACEAE: INCIDENCE AND RISK FACTORS IN A COMMUNITY-TEACHING HOSPITAL A. Makarem, MD; P. Alvarez, MD; M. Kulkarni, MD; M. Costello, PhD; T. Chou, MPH; J. Kerridge, RN; K. Wickman, RN; J. Malow, MD BACKGROUND METHODS Carbapenems are the treatment of choice for multidrug resistant Enterobacteriaceae. However, there have been increasing reports of carbapenem resistant Enterobacteriaceae (CRE), and their prevalence has increased since they were first described in 2001. The study population included adults who were hospitalized in our institution (level 1 trauma community-teaching Hospital, with 551 licensed beds, 2 adult intensive care units and a neonatal intensive care unit) from July 2008 through March 2010 and had positive cultures for CRE. CRE are resistant to almost all available antimicrobial agents. Infections with CRE have been associated with high rates of morbidity and mortality, even when treated appropriately, particularly among individuals with prolonged hospitalization and those who are critically ill and exposed to invasive devices. CRE detection: all bacteria with MIC > 1mcg/ml for any carbapenem and resistance to any 3rd generation cephalosporin are considered screen positive. These are then confirmed as CRE by modified Hodge test and Etest. Outbreaks have been reported in many countries, predominately Asia and South America. In the U.S., CRE were first reported in North Carolina, with the first reported healthcare-related outbreak in New York. Since then, CRE have been reported in at least 32 states. Patient records were reviewed for the following: type and location of residence, presence of indwelling devices (ventilator, central line, urinary catheter, and gastrostomy tubes), recent antibiotic exposure, signs and symptoms of infection, sites of positive cultures, co-morbidities, and mortality. RESULTS • There were a total of 20 patients with 32 CRE positive cultures in our institution during the study period. • 19/20 (95%) were infected, only 1 (5%) was colonized. FIGURES DISCUSSION All CRE isolates obtained are multidrug resistant with very limited therapeutic options, and are widespread throughout the extended care facilities (ECF) in the Chicago metropolitan area. With a mortality rate of 40%, CRE may pose a real challenge unless appropriately addressed. RESIDENCE OF PATIENTS WITH CRE POSITIVE CULTURES 30% 55% Horizontal dissemination appears to have an important role in the emergence of CRE infections. This is supported by the fact that most patients resided in an ECF prior to admission. Furthermore, only one patient had previous exposure to a carbapenem, and all infections were acquired prior to admission except for one. 10% NURSING HOME 5% LONG TERM ACUTE CARE FACILITY PRIVATE RESIDENCE Chronic illnesses and indwelling supportive devices also appear to increase the risk of acquiring CRE infections. This might be related to a decreased functional status, or possibly some degree of immunosupression, both of which have been reported as risk factors for CRE infections. REHABILITATION INSTITUTION ANTIBIOTIC SUSCEPTIBILITIES OF CRE ISOLATES A larger sample size is needed for more accurate calculations. 100% 80% 60% 40% 20% 0% CONCLUSIONS • Patients in extended care facilities are at risk for acquiring CRE. • Use of contact precautions, hand hygiene, and other infection control measures may limit the spread of CRE. • Only one patient (5%) had previous carbapenem exposure. • 40% had two sites of infection with CRE. SUSCEPTIBLE INTERMEDIATE • Screening for CRE should be considered in areas of high CRE endemicity. RESISTANT • Development of new antimicrobial agents is needed. • Infection sites included urine (60%), blood (25%), wounds (15%), sputum (15%), and PEG tubes (5%). • 2/5 of bacteremic patients died (40%). • 95% had at least one type of chronic indwelling supportive device (PEG tube, urinary catheter, tracheostomy, PICC line). SITES OF THE 32 CRE POSITIVE ISOLATES REFERENCES 1. Rapid Spread of Carbapenem-Resistant K pneumoniae in New York City. S Bratu, MD et al. Arch Intern Med. 2005;165:1430-1435. 18% 2. Carbapenemase-producing Enterobacteriaceae, U.S. rivers. Aubron, C., L. Poirel, R. J. Ash, and P. Nordmann. 2005. Emerg. Infect. Dis. 11: 260-264. • 90% had at least one chronic co-morbidity. • 80% of patients with chronic indwelling urinary catheter presented with CRE in the urine. • 30/32 CRE cultures (93.7%) were identified as K. pneumoniae while the other two isolates were E. coli and P. mirabilis. Represents the location of our institution Represents the residence locations of CRE positive cases 3. Carbapenem resistance in Klebsiella pneumoniae not detected by automated susceptibility testing. Tenover FC. Kalsi RK. Williams PP. Carey RB. Stocker S. Lonsw ay D. Rasheed JK. Biddle JW. McGow an JE Jr. Hanna B. Emerging Infectious Diseases. 12(8):1209-13, 2006 Aug. 15% 52% 4. Carbapenem-resistant Enterobacteriaceae: a potential threat. JAMA 300:2911-3 2008 5. Tigecycline for the treatment of multidrug-resistant Enterobacteriaceae: a systematic review of the evidence from microbiological and clinical studies. Journal of Antimicrobial Chemotherapy 62:895-904 2008 11% 6. Guidance for control of infections w ith carbapenem-resistant or carbapenemase-producing Enterobacteriaceae in acute care facilities. Centers for Disease Control and Prevention (CDC). Morbidity & Mortality Weekly Report. 58(10):256-60, 2009 Mar 20. URINE BLOOD SPUTUM PEG TUBE 7. Ventilator-associated pneumonia caused by carbapenem-resistant Enterobacteriaceae carrying multiple metallobeta-lactamase genes. Dw ivedi M. Mishra A. Azim A. Singh RK. Baronia AK. Prasad KN. Dhole TN. Dw ivedi UN. Indian Journal of Pathology & Microbiology. 52(3):339-42, 2009 Jul-Sep. WOUND 8. Potential role of active surveillance in the control of a hospital-w ide outbreak of carbapenem-resistant Klebsiella pneumoniae infection. Infection Control & Hospital Epidemiology 31:620-6 2010 4% 9. Risk Factors and Outcomes Associated w ith Acquisition of Colistin-Resistant KPC-Producing K pneumoniae: a Matched Case-Control Study. Zarkotou et al. J. Clin. Microbiol. 2010;48:2271-2274 160 140 120 100 150/3206 = 4.7% KPC Positive Patients ACL 148/3534 = 4.3% - 6 NDM PATIENTS WITH LAST 6 MONTHS - OXA-48 PATIENTS, PROBABLY (CARBAPENEM R, 3RD/4TH GENERATION CEPHALOSPORIN S, PIP/TAZO R) Chicago area 80 60 Milwaukee Southeast Wisconsin 53/3040 = 1.7% 36/2365 = 1.6% 40 36/2448 = 1.5% 20 2/2408=0.08% 0 2008 2009 2011 2012 Advocate 0 53 150 148 Aurora 0 2 39 36 KPC positive defined by modified Hodge positive or boronic acid positive /cloxacillin negative. Based on K. pneumoniae isolates. Figure 1. A) Worldwide geographic distribution of Klebsiella pneumoniae carbapenemase (KPC) producers. Gray shading indicates regions shown separately: B) distribution in the United States; C) distribution in Europe; D) EID, Oct. 2011 CURRENT TESTS FOR CARBAPENEMASE PRODUCERS • AST patterns (ACL - all carbapenems in Gram negative panels) • Gram negative panels must include doripenem, ertapenem, imipenem, and meropenem for optimal sensitivity • Modified Hodge test ( ACL - Screen if carbapenems are NS) • Lacks sensitivity (does not detect all NDM, VIM, IMI producers) and specificity (hyper AmpC producers) • Takes too long, an additional 24-48 hours • E Tests • MBL for verification of a metallo-lactamase - carbapenem +EDTA/carbapenem • Cefotetan/Cefotetan+ cloxacillin for AmpC expression • Takes too long • Rosco Disks (ACL - Classify carbapenemases) • Differentiates MBLs, from KPCs, from hyper AmpC • Low sensitivity for Oxa-48 • Takes too long • Amplified molecular methods (ACL – KPC only, so far) • Rapid • Sensitivity dependent on variation of sequences of carbapenem resistance genes • Costly? POSITIVE FOR KPC Modified Hodge test ROSCO Disks CLASS B CARBAPENEMASE • VIM, IMP, and NDM most common • NDM more common in E. coli than KPC • Require zinc at active site for hydrolysis of the beta-lactam ring • Resistant to all beta-lactams except for aztreonam • May not be modified Hodge Test positive CLASS B CARBAPENEMASE RECENT CASE - PATIENT HISTORY • 70 year old male. Visiting relatives. • History – diabetes and chronic kidney failure, on dialysis • Admitted 9/23/2012 to CMC for shortness of breath. • Cardiac surgery - Triple bypass • Complicated recovery, discharged 10/22 to Long Term Acute Care Hospital (LTACH) LABORATORY DATA Treated with Pip/tazo and fluconazole LABORATORY DATA Repeat urine culture on 10/3 was negative Fosfomycin = S Colistin Sample is MHT + Tigecycline AmpC MBL IMI + EDTA IMI NDM 10/8/2012 K. Pneumoniae MHT positive 2/17/2013 K. Pneumoniae MHT negative Meropenem + cloxacillin Meropenem + Boronic acid Meropenem Temocillin Positive = > 5 mm difference Meropenem + Dipicolinic acid CASE REVIEW • Patient not isolated prior to MBL report on 10/8 • Did treatment (Pip-tazo) select for MBL? • Rectal swabs taken on all patients in Adult Surgical Heart Unit. All were negative for MBL • Rectal swabs preincubated in 2 μg/ml ertapenem in TSB for 18 hours and then plated on gram negative selective media with meropenem disks. • Gown and glove precautions on entire unit. • Patient discharged to Kindred (LTACH) CURRENT METALLO Β-LACTAMASE OUTBREAK Pt.SQ. 70M 9/2012 CMC Indian national Urine - K. Pneumoniae x 2 NDM-1 confirmed by CDC Pt. In LTACH Pt. CK 68F 1/2013 LGH Urine – E. coli NDM-1 (CDC Confirmed) x 2 Undermined acquisition LGH - Seen in ER and admitted Risk factors: close relative Recent Travel to Asia/Canada Pt. MM. 68F 4/2013. LGH Abd. Wound- E. coli, NDM (CDC Confirmed) Present on admission to LGH Risk factors: unknown, new pt. At LTACH at same time Pt. FR. 85M 4/2013 Nursing Home Rectal swab – E. coli NDM (CDC Confirmed) Risk factors: Ventilator dependent, roommate to Pt. KK at nursing home B, multiple MDRs Pt. KK. 73M 3/2013 LGH Sputum - E. coli NDM-1 (CDC Confirmed) Present on admission to LGH Risk factors: ventilator dependent , feeding tube, LTACH and Nursing home stays Pt. expired 3/28/13 Pt. MR. 88F 3/2013 LGH Urine – E. coli NDM (CDC Confirmed) Present on admission to LGH Risk factors: multiple AB for frequent UTIs, recent nursing home stay (G), Dementia PFGE Results = highly related = pending Follow-up Actions • Each case reported to CCPH and IDPH by LGH Infection Prevention • Communicated to LGH and Advocate Senior leadership • Education provided to physicians and associates • There are no relationships among these cases with locations and time at LGH • CCDP and IDPH conducting active surveillance of CRE in LTACH and 2 Nursing Homes • LTACH screen 25% KPC+ • Active surveillance for CRE on LGH Rehab Unit negative • Beginning 4/29 all admits to LGH Rehab Unit will be screened for CRE • ~20% KPC+ • 55% P. aeruginosa carbapenem resistant NATIONAL RESISTANCE ALERT 3 ADDENDUM CARBAPENEMASE-PRODUCING ENTEROBACTERIACEAE IN THE UK: NDM (NEW DELHI METALLO-) Β-LACTAMASE: REPEATED IMPORTATION FROM INDIAN SUBCONTINENT • Numbers of carbapenemase-producing Enterobacteriaceae continue to increase sharply • Many recently referred carbapenemase producers have NDM (New Delhi Metallo)-β-lactamase • • Most producers are resistant to ALL antibiotics except polymyxins and tigecycline and may pose a serious treatment challenge in severe infections · Vigilance and good infection control are essential to minimize transmission and accumulation in the UK NDM-1 + • E. coli • K. pneumoniae Medical Tourism Detection of Enterobacteriaceae Isolates Carrying Metallo-Beta-Lactamase — United States, 2010 – MMWR. June 25, 2010 • K. oxytoca • Enterobacter spp. • Proteus spp. • C. freundii • M. morganii • Providencia spp. Metallo β-Lactamases, Next Wave NDM, Current Wave IMP = imipenem hydrolyzing metallo β-lactamase NDM = New Delhi Metallo carbapenemase VIM = Verona Integron-encoded Metallo-β-lactamase Emerging Infectious Disease, Oct. 2011 THE CARBAPENEMASE THREAT CLASS D - OXACILLIN HYDROLYZING ΒLACTAMASE • First identified in Turkey in 2003, • Originated from Shewanella spp. • Confers resistance or reduced susceptibility to carbapenems and penicillin-inhibitor combinations, but producers only show slight resistance to oxyiminocephalosporins (Ceftriaxone, Ceftazidime) unless they have co-resident mechanisms such as ESBLs or AmpC. • High-level resistance to both piperacillin-tazobactam and temocillin may be useful indicators of OXA-48 production in enterobacteriae • Found in Acinetobacter baumanii, Pseudomonas aeruginosa, and Enterobacteriaceae. • Not confirmed in Midwest??? OXA-48 EID, Oct. 2011 WHY CARE ABOUT MECHANISMS OF RESISTANCE? • Carbapenemases • Chromosomal Vs. plasmid based • Chromosomal – Not an Infection Control Emergency • SME, NMC • See more with lower carbapenem breakpoints • Plasmid – Infection Control Emergency! • KPC, NDM, GES, VIM, Oxa-48 • Need to isolate all patients?? • A commercially available, standardized, and reproducible amplified molecular assay will make CRE detection/identification faster, more sensitive, and consistent NANOSPHERE - GRAM NEGATIVE BLOOD CULTURE ID • Pathogens detected • Escherichia coli/Shigella spp., Klebsiella pneumonaie, Klebsiella oxytoca, Serratia marcescens, Pseudomonas aeruginosa, Citrobacter spp., Enterobacter Spp., Proteus spp., Acinetobacter spp. • Resistance genes • KPC • NDM • CTX-M • VIM • IMP • Oxa-48 IN SUMMARY Clinical Cases • New resistance mechanisms, new challenges • Lines blurring between HAI and community acquired infections • MRSA, CREs, ESBLs, etc. • ESBLs are not just HAI’s anymore Asymptomatic Carriage • Team approach absolutely required • Lab, Pharmacy, and ICPs • Antibiotic stewardship • Lab needs to be more responsive and less conservative • Do you need to double check your results prior to reporting? • Patient to patient transmission can be limited by strict infection control measures • Laboratory identification of infection or carriage must be paired with rapid implementation of infection control measures • Group effort required • Screening – who pays? • Ongoing surveillance is essential • Surveillance must include extended care facilities and cooperation between healthcare systems • Moving target • Rapid detection and reporting essential