Slide Presentation - Maryland Hospital Association
advertisement
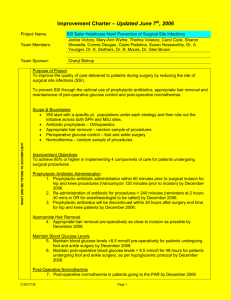
Surgical Site Infection SUSP Armstrong Institute for Patient Safety and Quality Presented by: Elizabeth C. Wick, M.D. and Deborah B. Hobson, R.N. Learning Objectives • Understand pathogenesis, monitoring and prevention of SSIs • To explore how to implement evidence-based behaviors to prevent SSIs 2 Proportion of Adverse Events Most Frequent Categories 25% Non-surgical 20% Surgical 15% 10% 5% 0% Drugrelated Wound infect. Tech. comp. Late comp. Diag. mishap Therap. mishap Nontech. comp. Proc. related Brennan. N Engl J Med. 1991;324:370-376 4 Background • SSI is the most common nosocomial infection in the surgical patient • SSI is the most common complication after colorectal abdominal surgery (3-30%) • SSI is associated with increased mortality, length of stay and readmission • An SSI costs between $6,200 - $15,000/per patient (superficialorgan space) Smith et al, Ann Surg, 2004 Wick et al, Arch Surg, 2011 5 Pathogenesis of SSI Host Bacteria Procedure 6 SSI Definitions • Superficial – – – – purulent drainage from wound positive wound culture pain, redness swelling diagnosis by surgeon • Deep – purulent drainage from deep aspect of wound – dehiscence – abscess on exam or CT scan • Organ Space – infection in surgical cavity (abdomen) 7 Monitoring: NHSN (CDC-National Healthcare Safety Network) NEW MANDATORY Monitoring: colon and hysterectomy • Rate will be risk adjusted based on age and ASA • Deep incisional and organ space rates for colon and hysterectomy will be reported to CMS (required for full payment) • Data to be transmitted to CMS late 2012, 2013 • Hospital specific standardized infection ratios will be generated for colon and hysterectomy http://www.cdc.gov/nhsn/PDFs/FINAL-ACH-SSI-Guidance.pdf 8 Monitoring: NSQIP (National Surgical Quality Improvement Program) • Data – Robust preoperative risk factors for risk adjustment – 30-day postoperative mortality and morbidity • Program – Costs approximately $30K/year; infection only one of many outcomes studied – Requires full time RN dedicated to data collection AND surgeon champion – Includes annual audit by NSQIP and risk adjusted reports – Option to collect all colon and rectal procedures vs. random sample of surgical procedures 9 SCIP PROCESSES TO PREVENT SSI 10 Does SCIP Give Us Enough information? Johns Hopkins Comparison Hospitals Surgery patients who were given an antibiotic at the right time (within one hour before surgery) to help prevent infection 98% 97% Surgery patients who were given the right kind of antibiotic to help prevent infection 98% 98% Surgery patients whose preventive antibiotics were stopped at the right time (within 24 hours after surgery) 97% 96% Surgery patients needing hair removed from the surgical area before surgery, who had hair removed using a safer method (electric clippers or hair removal cream – not a razor) 100% 100% Patients having surgery who were actively warmed in the operating room or whose body temperature was near normal by the end of surgery. 98% 99% SCIP Data Johns Hopkins Hospital. May 2010 SCIP, Hospital Compare, www.medicare.gov 12 Johns Hopkins CUSP Experience: Room for Improvement in SCIP Compliance Problem : Penicillin-allergic patients undergoing colorectal surgery were not receiving proper prophylactic antibiotics (Clindamycin and Gentamycin). 13 Antibiotic Compliance Project Johns Hopkins Correct Dose of Gentamicin Received 75 • Increased amount of gentamicin available in the room 50 • Added dose calculator in anesthesia record 100 % of Patients Compliant Interventions 92% 33% • Educated surgeons, anesthesia, and nursing in 25 0 Before After Wick et al, JACS 2012 (in press) 14 Perioperative Antibiotic Compliance: Michigan Surgical Quality Collaborative Antibiotics practices All cases (n = 3002) number (%) Was an SCIP-compliant antibiotic 2,431 (81.4%) chosen? Was antibiotic given within 1 h before 2,712 (90.8%) incision? Nonemergency Emergency cases (n = 2743) (n = 248) number (%) number (%) 2,293 (83.6%) 130 (52.4%) 2,544 (92.7%) 159 (64.1%) 245 (8.9%) 24 (9.7%) Antibiotics weight-adjusted (n = 972) 552 (56.8%) Antibiotics redosed (n = 398) 24 (6.0%) Total surgical site infection 269 (9.0%) Hendren et al. Am. J Surg 2011 15 Johns Hopkins CUSP Experience: Room for Improvement in SCIP Compliance Problem: Patients arrive in the recovery room with temperature < 36°C despite having a forced air warmer during surgery 16 Normothermia Project Johns Hopkins Temperature > 36 °C Post-Op 95% % of Patients Compliant 100 83% 75 Interventions • Confirmed that temperature probes were accurate (trial comparing foley and esophageal sensors) 50 • Initiated forced air warming in the pre-operative area 25 • Heightened awareness 0 Before After Wick et al, JACS 2012 (in press) 17 EMERGING EVIDENCE FOR SSI PREVENTION 18 Emerging Evidence for SSI Prevention 1. Antibiotic Usage – Redosing – Weight based dosing of cephalosporins 2. Maintenance of normogylcemia 3. Utilization of mechanical bowel preparation with oral antibiotics 4. Standardization of skin preparation 19 Additional Interventions to Improve Antibiotic Efficacy • Antibiotic Redosing – Maintain therapeutic antibiotic serum levels during entire procedure Medication Dosing Interval Cefazolin q3hrs Cefotetan q6hrs Cefoxitin q2h Clindamycin q6h Vancomycin q12h Consensus Guidelines, in press IDSA/SIS/SHEA/AHPS 20 Hyperglycemia and Infection BACKGROUND: • Hyperglycemia is common in hospitalized patients • 38% of medical and surgical patients had hyperglycemia (26% diabetic and 12% non-diabetic • In cardiac surgery, degree of postoperative hyperglycemia correlates with SSI; adopted as SCIP measures GOAL: Glucose <180mg/dl in all hospitalized patients Ramos. Ann Surg 2008 21 Preparation of the Surgical Site BACKGROUND • • 1012 Bacteria reside on the skin Staphlococcus and Streptococcus species among others GOAL OF SKIN PREPARATION • Reduce bacterial burden on skin prior to incision BEST PRACTICE • • • • Dual-agent skin preparation (chlorhexidine + alcohol, providone-iodine +alcohol) Skin prep should include alcohol to increase durability of sterilization Prep should be applied to specification (duration and amount) Prep must dry before incision Darouiche RO et al. N Engl J Med. 2010 Swenson BR et al. Infect Control Hosp Epidemiol. 2009 23 Bowel Preparation: A Brief History • Oral antibiotics for prevention of SSI was first described in the 1940’s • 1973 Nichols and Condon FAVORABLE • 1974 Washington et al randomized trial FAVORABLE • 1990’s-2000’s oral antibiotics fell out of favor in US – Patients not tolerant of preparation (nausea, dehydration) • 2002 Lewis et al – Randomized controlled trial – Oral neomycin and metronidazole plus systemic antibiotics vs systemic antibiotics alone (5% neomycin and metronidazole vs 17% placebo) Reviewed in Fry, 2011. 24 Bowel Preparation: A Brief History • Rigorous studies of IV antibiotics did not include oral antibiotics • 1990’s-2000’s oral antibiotics fell out of favor in US – Patients not tolerant of preparation (nausea, dehydration) – Patients no longer admitted to hospital pre-operatively • Lewis et al (2002) – Randomized controlled trial – Oral neomycin and metronidazole plus systemic antibiotics vs systemic antibiotics alone (5% neomycin and metronidazole vs 17% placebo) • 2012 – AHPSA guidelines on antimicrobial prophylaxis endorse use of oral antibiotics with mechanical bowel preparation plus IV antibiotics to prevent SSIs Reviewed in Fry, 2011. 25 Cochrane Review: Oral Antibiotics + Bowel Preparation is Associated with Lowest SSI Rate Guenaga Study2 SSI Rate SSI Rate Nelson Study1 MBP + oral + parenteral MBP no oral + parenteral MBP + + parenteral No MBP + + parenteral MBP = Mechanical Bowel Preparation Slide adapted from Patch Dellinger, MD University of Washington 1Guenega, 2Nelson, Cochrane Database Syst Rev,2009 Cochrane Database Syst Rev,2009 27 Summary of SCIP and Emerging Evidence to Prevent Colorectal SSIs • Appropriate prophylactic antibiotics – – – – – Selection* Weight-based dosing of cephalosporins Timing* Redosing Discontinuation* • Appropriate hair removal as close to time of surgery as possible* • Temperature management* • Appropriate glycemic control • Dual agent (with alcohol) surgical skin prep • Mechanical bowel prep and oral antibiotics *SCIP measures 28 Next Steps • Review current colorectal SSI bundles at your hospital (policy and practice) • Review hospital process measure data • With assembled CUSP team, plan for administration of staff safety assessment 29 Poll Who’s on the call? 30 Poll Does your hospital have a colorectal SSI bundle in place? 31 Poll If your hospital has a colorectal SSI bundle in place, what’s in it? 32 On-boarding Call Evaluation We want to ensure that the on-boarding calls provide useful and pertinent information for the SUSP teams. For this reason we request that you complete a brief evaluation following each call. The evaluation may be found at the following link: • https://www.research.net/s/susp_cohort_3 If you are not able to reach the link from the slide, please cut & past the URL into your browser. 33 Armstrong Institute for Patient Safety and Quality