EmpoweringPrimaryCare_PBreakout
advertisement
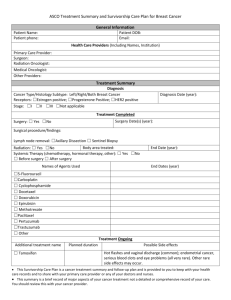
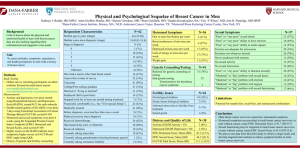
Empowering primary care physicians to handle survivorship needs DR. JULIA USATINSKY DR. NIJAL PATEL Who are the survivors? A cancer survivor is an individual from the time of cancer diagnosis, through the balance of his/her life National Cancer Institute definition Epidemiology Epidemiology of Breast Cancer An estimated 226,870 new cases of invasive breast cancer are expected to occur among women in the US during 2012; about 2,190 new cases are expected in men. Excluding cancers of the skin, breast cancer is the most frequently diagnosed cancer in women. The breast cancer incidence rate began to decline in 2000 after peaking at 142 per 100,000 women in 1999. The dramatic decrease of almost 7% from 2002 to 2003 has been attributed to reductions in the use of hormone therapy Epidemiology of Breast Cancer The 5-year relative survival rate for female breast cancer patients has improved from 63% in the early 1960s to 90% today. The 5-year relative survival for women diagnosed with localized breast cancer is 99%; if the cancer has spread to nearby lymph nodes (regional stage) or distant lymph nodes or organs (distant stage), the survival rate falls to 84% or 23%, respectively. For all stages combined, relative survival rates at 10 and 15 years after diagnosis are 82% and 77%, respectively Epidemiology of Colon Cancer An estimated 103,170 cases of colon and 40,290 cases of rectal cancer are expected to occur in 2012. The third most common cancer in both men and women. Incidence rates have been decreasing for most of the past two decades, which has largely been attributed to increases in the use of screening tests that allow the detection and removal of polyps before they progress to cancer. Epidemiology of Colon Cancer The 1- and 5-year relative survival rates for persons with colorectal cancer are 83% and 64%, respectively. When colorectal cancers are detected at an early, localized stage, the 5-year survival is 90% Cancer Survivors Distribution of cancer survivors in the U.S. by site, 2002. Survivors . The number of cancer survivors in the United States increased steadily during the past three decades: CDC/NCI. MMWR 2004;53:526-529. Increased from 3.0 million (1.5% of the U.S. population) in 1971 to 9.8 million (3.5%) in 2001, and expected to double by 2050 CDC. Cancer Survivorship–United States 1971-2001. MMWR. 2004: 53:526-529 Survivorship Care …increasing (survivors) population combined with predicted shortages of PCPs and oncologists will present unique challenges to making sure that cancer survivors receive high-quality cancer survivorship care.” ~Katherine Virgo, PhD, MBA, managing director of health services research at the American Cancer Society's Survivorship Care “People with histories of cancer have the right to continued medical follow-up with basic standards of care that include the specific needs of long-term survivors.” (Principle 6) ~National Coalition for Cancer Survivorship, 12 principles What are the needs of the survivors? Monitor for early complications after treatment Detect late effects of treatment Detect recurrences early Address general health issues (might have higher propensity for other health-related issues) Address psychological health Health maintenance Some other areas Care for the family members Ensure compliance with adjuvant therapies Direct exercise and nutrition Address quality-of-life issues Most importantly: return to normal life Who should follow? Journal of Clinical Oncology, 2009: PCPs are willing to assume exclusive responsibility for routine follow-up care after completion of active treatment. The following modalities were felt to be most useful to assist PCPs in assuming responsibilities: A patient-specific letter from the specialist Available guidelines Expedited routes of referral and access to investigations for suspected recurrence Who does better job? Lack of evidence supporting advantages of long-term follow-up care in Oncology clinics No significant difference in: Time to detection of disease recurrence Frequency of serious clinical events related to recurrence Health-related quality of life of cancer survivors Data from BMJ, J Clin Oncol, Br J Cancer, Eur J Cancer Prev What are the barriers? “Inadequate training” and “uncertainty” who is providing what care are concerns Journal of General Internal Medicine, 2011 (breast, colon) “CME initiatives” and “an enhanced cooperative effort between those delivering and coordinating…care” are needed Supportive Care in Cancer, 2010 “Inadequate preparation and lack of formal training” Cancer, 2009 (any cancer) What do our patients think? Survey of 300 breast cancer survivors: PCPs do great job at general care, psychosocial support, and health promotion However: Knowledgeable about cancer follow-up- 50% PCPs and oncologists communicate well- 28% Journal of Clinical Oncology, 2009 Common themes: Fragmentation of care Fragmentation of care One major barrier to successful transition is fragmentation of care Many cancer patients choose to receive treatment at hospitals where their primary care physicians aren't affiliated. Cancer center may not be coordinated electronically with the PCP’s office Fragmentation of care An average of 3 specialists/patient, with treatments across time and space…outpatient, inpatient, specialized treatment facilities…. Increasing with aging of the population Limited communication among treating physicians, multiple medical records Common themes: Lack of adequate knowledge/training Not enough training for PCPs in Medical School Cancer survivorship has yet to be well represented in undergraduate medical school curriculum and only a few schools currently offer courses or clerkships pertaining to cancer survivorship Not enough training! Pheochromocytoma: annual incidence is approximately 0.8 per 100,000 person years Hours of medical school and residency curriculum Oddly dominates lectures on hypertension Cancer survivor: one in every 25 Americans Review of curriculum guidelines of internal medicine and family medicine found a lack of mention of cancer survivorship Not enough guidelines for PCP Many guidelines address only the first five years post-treatment when patients are followed by their oncologist, but not for the period after that, when patients are being returned to their primary care physicians What do we do to fix it? Overcoming barriers Patients can be given a comprehensive care summary and follow-up plan that is clearly and effectively explained Frequent communication between the oncologist and PCP Cancer Treatment Plan and Summary Follow up care plan Overcoming barriers Improving medical schools/residency curricula Including cancer survivors as “standardized patients” by some medical schools Developing integrated curriculum on cancer survivorship Problem-based learning cases Multimedia web-based problems Introducing various CMEs for practicing physicians Overcoming Barriers Educating primary care physicians and oncology providers, as well as empowering patients, are key components Increasing the availability of evidence-based guidelines on cancer survivorship; existing guidelines should be refined Follow up guidelines Breast Cancer Follow Up Breast Cancer Follow Up Breast Cancer Follow Up Breast Cancer Surveillance Not Recommended Routine Blood Tests CBC and LFTS not recommended Imaging Studies CXR, Bone scans, liver U/S, CT scans, PET scans and Breast MRI not recommended Tumor Markers CA 15-3, CA 27.29 and CEA are not recommended Colon Cancer Lung Cancer CXR or CT is recommended every 6 months for 2 years and then annually Use of blood tests, PET scan, sputum cytology, tumor markers, and fluorescence bronchoscopy is not currently recommended for surveillance Patients who smoke should be strongly encouraged to stop smoking ACS Guidelines on Nutrition and Physical Activity for Cancer Survivors Achieve and maintain a healthy weight. •If overweight or obese, limit consumption of high-calorie foods and beverages and increase physical activity to promote weight loss. Engage in regular physical activity. •Avoid inactivity and return to normal daily activities as soon as possible following diagnosis. •Aim to exercise at least 150 minutes per week. •Include strength training exercises at least 2 days per week. Achieve a dietary pattern that is high in vegetables, fruits, and whole grains. • Follow the American Cancer Society Guidelines on Nutrition and Physical Activity for Cancer Prevention. Use of Supplements All attempts should be made to obtain needed nutrients through dietary sources. It may be counterproductive take folate supplements when receiving antifolate therapies such as methotrexate. When to supplement Only if a nutrient deficiency biochemically (eg, low plasma vitamin D levels, B12 deficiency) clinically (eg, low bone density) If nutrient intakes fall persistently below two-thirds of the recommended intake levels Consult a registered dietitian avoid ingesting supplements that exceed more than 100% of the Daily Value CASE Clinical Case AR is a 40 year old female with history of left sided breast cancer in which per patient she received chemotherapy and radiation and had a lumpectomy. Further information is unknown as patient just moved from out of state and her oncologist is retired, and she is unsure what hospital he was affiliated with. CC- progressively worsening SOB over the last 2 weeks PMH- breast cancer, HTN, and hyperlipidemia SH- not currently working, denies alcohol, smoking and drugs PE- Bibasilar crackles, 2+ lower extremity edema, lymphedema of the left arm Issues for the Patient Did my cancer spread to my lungs How do I make sure my 3 daughters and 2 sisters do not have breast cancer What further tests need to be done to make sure I do not have another cancer Colonoscopy Pap Smear Lung Cancer Skin Cancer Issues for the PCP Is this SOB secondary to CHF from Previous medical problems Radiation Chemotherapy Anthracycline, traztuzamab What chemotherapy regimen did the patient receive What follow up tests have been done for the patient and what needs to be done Possible Answers for Patients Issues Cancer spread to lungs- Unlikely because symptoms most consistent with CHF Genetics- Need to go over the recommendations for genetic referral Other cancers- Patient needs to be screened as any other patient; close monitoring of skin for malignancy Possible Answers for PCP issues Why SOB- will need further testing including ECHO, CXR to look for cause of SOB What regimen- not available at this point but this is where summary is helpful What tests need to be done- CHF workup, mammogram Conclusions With improvements in medical education and coordination of care, primary care will offer a safe, cost-effective method in providing routine (and often exclusive) follow-up care for cancer survivors Discharging cancer survivors from oncology programs will reduce the load of well patients on already busy cancer clinics Refining guidelines, risk-stratifying patients, as well as providing patients with follow-up care plans, will make this process better structured and coordinated. Available Resources Available resources Up to Date- now a small section on cancer survivorship, and more chapters are being written focusing on the topic ACP's online decision support tool, PIER (Physicians' Information and Education Resource) includes information on follow-up care organized by type of cancer The American Society of Clinical Oncology houses information on cancer survivorship on its website The American Cancer Society and the National Cancer Institute jointly co-sponsor a cancer survivorship conference every two years that allows the research community to come together to discuss the issue Questions? Thank You!