Working to improve Transition services both in the South West and
advertisement
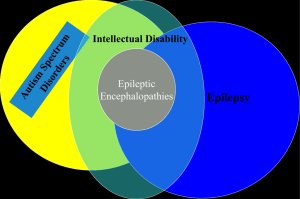
SW Strategic Clinical Network for Maternity & Children Reducing Avoidable SCN Conference Unplanned Hospital Reducing Avoidable Unplanned Hospital Admissions Admissions Long Term Conditions Long term Conditions th October November 14 2014 2014 Exeter Rugby Club Matthew Ellis Associate Clinical Director CYP Priorities Working Groups • Avoiding Unplanned Admissions • Long Term Conditions Themes Smarter network thinking • expertise earlier on pathways Integrated working • (1° / 2°/ 3°, Health/CYPS) Making the Unplanned Planned Parity of Esteem NHS Outcome Framework areas for improvement • 2.3 (2) Unplanned hospitalisation for asthma, diabetes and epilepsy in under 19s • 3 a Emergency admissions for acute conditions that should not usually require hospital admission • 3.2 Emergency admissions for children with LRTI Scale of CYP patient flow on the ’emergency/urgent care pathway’ around the South West? How big is the patient flow on the • >120,000 emergency department walkins carecare pathway’ • ’emergency/urgent > 18,000 GP referrals for urgent theassessed South inWest • around > 25,000 CYP specialist paediatric assessment units (SPAUs) >120,000 emergency department walkins involve CYP around south west annually > 18,000 GP referrals involve CYP around south west annually Big 6 (account for >50% admissions) + • abdominal pain • asthma/wheezy child • bronchiolitis • feverish illness • gastroenteritis • head injury • + self harm (up by 68% in the last 10 years) Variation across the Region eg Zero length of stay admissions Zero days admissions 6 Provider responses (n=10 of potential 14) Assessment Unit (SSPAU) • 7 units report this provision • variables where/when/who? Rapid Access Clinic • 6 units report this provision • Variables how often? Complexities of Systems Taxonomy of Potential Pathways and Referral Routes Primary Care Home 2h Incl MIU, Community Nurse, CAMHS, Social services, Midwives etc 2 GP Home 3h e 2p Home 2c 1g 5h 5e ED 1e Family 5a 7 5 3p 3 WARD Paeds 1 7h Home 5u 5c 1p 7c 4e 1s 3c SWAST 6a 8a 8e 4p Ambulance service 4 Home 4h HOT CLINIC 4c 8a e.g. Next Day Service Home 8h 8 6c IP PAU 6 OP 6i 6o 6h Home Advice and Guidance 8 (of 14) hospitals consulted ‘offer’ this service • 3 - Consultant, 3 – ST, 1 - SHO,1 - ED, Only 1 is formally commissioned and routinely records the activity for this service Commissioned @£100k PA 20% deflection • Vast majority to ‘home care’ • Minority to ‘hot clinic’ “It’s Good to Talk”: Looking at the effect of a GP Phone Advice Service within a Children’s Emergency Department Dr Zoe Roberts, Dr Rosie Fish, Dr Jacqueline Seckley, Dr Will Christian Introduction Methods/Design The Children’s Emergency Department has seen a significant increase in yearly attendances, many of which could have been dealt with in the primary care setting. With increasing pressures on acute paediatric services, the Bristol Children’s Emergency department introduced a telephone advice line for primary care providers in April 2012. The aim is for this to be delivered by the ED consultant group in order to try and reduce unnecessary visits and support primary care providers in their clinical practice. A one-month pilot study was undertaken in May 2011 to inform the development of the service. Following this a further, more detailed analysis was undertaken in June 2011, looking at all phone referrals to the department. Details documented included: • Grade of person taking the call • Brief history /examination • Time of call findings including vital signs • Patient demographics • Agreed Plan • Referrer • Outcome (including advice given • Reason for referral and disposal) Following this a survey was distributed to all GPs involved in the pilot study for feedback. Results: Total of 350 calls in June (average 12 per day) GP Feedback Survey YES NO DON’T KNOW Did you find speaking to the doctor helpful 87.5% - 12.5% Was it clear which grade of doctor you spoke to? 62.5% 37.5% - Did you think it enhanced the patient journey? 75% 12.5% 12.5% Did you feel happy with the advice given? 87.5% - 12.5% If no to above, was this because you spoke to a junior? - 66.7% 33.3% Was it easy to contact the dept and speak to the right person 85.7% 14.3% - Should we continue to offer this service? 100% - - Outcome of Call (by grade) Conclusion: In _ out of _ cases, the call resulted in the avoidance of a same day ED attendance. There was no obvious difference in outcome according to grade which may reflect on both the seniority of the trainees taking the call and the availability of consultant advice during the hours of 0800 – 22.30. Because there is a written record of the call, the consultant / senior trainee is often more aware of the acuity presenting to the ED and in some cases this has resulted in escalation of the pre-hospital management. Whilst we are succeeding in the overall aim of reducing emergency department attendances and there appears to be support for this service from GPs, it has also brought its own challenges namely consultants being drawn away from the shop floor during our busiest times and the potential financial loss caused by the reduction in ED attendance tariffs. Therefore in order to ensure its sustainability, we need to ensure adequate consultant availability and consider the potential for financial recompense for this service. Best Practice Network Standard Advice and guidance • An 8 to 8 service for GPs to access advice and guidance from local paediatrician SEE Revised Facing Future Standards: RCPCH in consultation 2014 ‘immediate telephone advice for acute problems for all paediatricians for all specialties’ Advice and Guidance • Use Network to leverage commissioned advice and guidance by paediatricians for primary care across the region in 2015 • Use Network to leverage specialist advice and guidance for paediatricians by specialist paediatricians across the region in 2015 Assess what worksstandardise unit metrics to allow more informed evaluation of initiatives at unit level • establish the simple core data needed for evaluation of initiatives at local level using unit trend data • Pilot data collection in individual units to ensure that data collection is feasible in 2014 • Procede to a region wide evaluation study in 2015 Long Term Conditions 0-16 years Prevalence South West • Diabetes: 2,000 • Epilepsy: 8,000 • Asthma: 40,000 boys 30,000 girls • ‘Core’ Disability: 0-16 yrs 56,000 0-25 yrs 90,000 15 NHS 2013 2013 commissioned review 1990-2013 NHS 2013 16 • 2/3rds of deaths in those with complex needs • Half of these ie 1/3 of all deaths in children with neurodevelopmental conditions Making the unplanned planned – Community Childrens Specialist Nursing • Diabetes Nurse – HbA1C control • Practice Nurse – asthma planning • Epilepsy Nurse – AED compliance emergency fit control Epilepsy 12 audit Category Professionals Assessment & Classification Investigation Management & Outcome Title Performance indicator 1 Paediatrician with expertise in epilepsies % of children with epilepsy, with input from a consultant paediatrician with expertise in epilepsies by 1 year 2 Epilepsy Specialist Nurse % of children with epilepsy, referred for input by an epilepsy specialist nurse by 1 year 3 Tertiary involvement % of children meeting defined criteria for paediatric neurology referral, with input of tertiary care by 1 year 4 Appropriate first clinical assessment % of all children, with evidence of appropriate first paediatric clinical assessment 5 Seizure classification % of children with epilepsy , with seizure classification by 1 year 6 Syndrome classification % of children with epilepsy, with epilepsy syndrome by 1 year 7 ECG % of children with convulsive seizures, with an ECG by 1 year 8 EEG % of children who had an EEG in whom there were no defined contraindications 9 MRI % of children with defined indications for an MRI, who had MRI by 1 year 10 Carbamazepine % of children given carbamazepine, in whom there were no defined contraindications 11 Accuracy of diagnosis % of children diagnosed with epilepsy whostill had that diagnosis at 1 year 12 Information & advice % of females over 12 years given anti-epileptic drugs, who had evidence of discussion of pregnancy or contraception Epilepsy12 Performance results across the South West Strategic Clinical Network Paediatrician with Epilepsy Appropriate expertise in specialist Paediatric first clinical Seizure Syndrome epilepsy nurse neurologist assessment classification classification Cornwall Plymouth Torbay Exeter North Devon Taunton Yeovil Bath Bristol Weston Swindon 66.7 100 36.4 100 66.7 16.7 45.5 0 100 0 44.4 75 50 50 100 100 83.3 72.2 0 50 0 0 38.9 0 83.3 11.1 50 20 Gloucester Key Significantly better than England No difference from England ignificantly worse than England No data available 100 50 100 100 33.3 50 ECG EEG Withdral Pregnancy or of contraception MRI Carbamazepine diagnosis discussion 75.9 73.9 40 61.4 77.8 83.3 72.7 85.7 44.4 40 82.8 75 16.7 71.4 100 40 27.3 92 37.5 14.3 45.5 95.5 57.1 100 62.5 65.6 57.1 55.6 79.7 70 98.2 73.1 88.9 83.3 50 83.3 66.7 100 100 94.4 11.1 8.3 0 100 44.4 25 50 11.1 100 55.6 18.2 100 22.2 60 66.7 43.6 40.9 81.3 93.8 90.5 100 93.2 90 93 92.5 75 45.5 0 66.7 50 100 69.2 69.2 100 100 100 100 100 66.7 100 100 100 91.7 100 100 85.7 66.7 100 100 100 73.2 81.8 0 100 100 100 100 100 How can younetwork help achieve these three ConcluSmarter thinking expertise earlier principles? on pathways Integrated working Smarter network thinking with expertise (1° / 2°/ Health/CYPS) earlier on3°, pathways Making the Unplanned Planned Integrated working sions Making the Unplanned Planned • Thankyou • Questions?