A Patient in Labor with Marfan Syndrome
advertisement

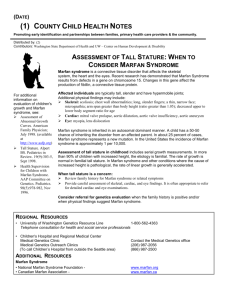
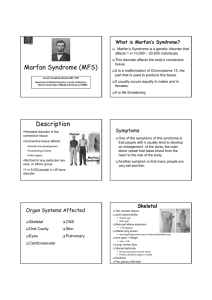
A Patient in Labor with Marfan Syndrome Aubrey Ballard, SRNA Missouri State University Objectives Presentation of Case Study Marfan Syndrome Marfan Syndrome and Pregnancy Marfan Syndrome and Anesthesia Answer Questions Patient Information 20-something year old, female Transported via EMS in labor, 175/115 Limited prenatal care; preeclampsia History of methamphetamine use (quite 4 months prior). Negative urine drug screen “Writhing in pain”, noncompliant with instructions, not allowing monitoring or additional lab work Anesthesia consulted for labor epidural Lab Values WBC 13.8 H RBC 4.22 L Hgb 12.0 Hct 36 Plt 281 PT 14.2 INR 1.1 PTT 26 Lab Values Sodium 138 Total Bilirubin 0.3 Potassium 3.3 AST 16 Chloride 103 ALT 24 CO2 22 Alk Phos 232 BUN 4 Lactate Dehydrogenase 231 Creatinine 0.6 Total Protein 6.4 Est. GFR >60 Albumin 2.9 Glucose 104 Uric Acid 7.3 Calcium 8.6 Magnesium 1.3 Urinalysis Color Yellow Clarity Slightly Cloudy pH 8 Specific Gravity 1.015 Protein 3+ RBC 2-5 WBC 2-5 Crystals Present Bacteria Few Casts None Mucus Small Patient Information Allergies: Codeine Current medications: multi-vitamin, magnesium gtt Anesthesia interview conducted Marfan Syndrome (MFS) Autosomal dominate genetic defect in fibrillin-1 or fibrillin-2 gene Fibrillin is a major component of microfibrils and also help store TGF-β Inherited or de novo germline mutations Diagnosis made from physical features & heredity Changes associated with MFS Cardiovascular Aortic dilation/dissection – especially at the root Aortic and mitral valve prolapse/regurgitation Pulmonary artery dilation Arrhythmias, cardiomyopathy, congestive heart failure Skeletal Arachnodactyly with hyperextensibility Chest wall deformities Scoliosis/kyphosis Osteoporosis High arched pallet, retrognathia, micrognathia Changes associated with MFS Ocular Lens subluxation Myopia Cataracts Retinal detachment Glaucoma Pneumothorax/pulmonary blebs, asthma, emphysema Inguinal and incisional hernias Dilation of dural sac Dissection of cranial arteries and aneurysmal subarachnoid hemorrhage Marfan & Pregnancy Pregnancy increases the likelihood of cardiovascular complications in patients with MFS Approximately 15% of MFS patients develop a major CV manifestation with pregnancy & 40% have obstetric complications Prophylactic treatment with beta-blockers or internal defibrillators has been suggested before conception Increased CO during labor and after delivery increases risk of aortic rupture Vaginal delivery vs. Cesarean section Prolonged maternal bleeding Marfan & Anesthesia In depth history and physical Hemodynamic management of cardiovascular conditions; Arterial line General vs regional (no epinephrine for blocks) Possible difficult intubation; minimize laryngoscopic response Careful positioning – joint laxity Dural ectasia Recognize and treat aortic dissection S/S of Aortic Dissection Important to distinguish dissection from ischemia Abrupt onset of severe chest or back pain Does not respond to nitrates or beta-blockers acutely but may decreased with decrease in blood pressure New aortic diasolic murmur, unequal peripheral pulses or BP, absence of rales with chest pain Ischemia may occur with aortic root involvement Treatment of dissection Lowering BP & decreasing myocardial contractility X-ray, echo, MRI, CT, TEE Anticoagulation/thrombolytic therapy contraindicated Need for surgery based on size and location MFS aneurysm >4.5 cm indicates need for operative repair Case Study Emergent Cesarean Section with RSI In room at 0936 with BP – 155/105 Incision at 0943 with deliver of baby at 0944 BP decreased to 92/68 Extubated without difficulty and transported to PACU CT CT findings A dissection that starts in the distal aortic arch between the takeoff of the left subclavian and the aberrant right subclavian artery that extends throughout the thoracic aorta, ending just above the level of the celiac trunk and upper abdominal aorta. The takeoff of the aberrant right subclavian artery is ectatic measuring 2 cm in diameter. The distal aortic arch is ectatic measuring 3.2 cm in diameter. Case Study Taken to ICU Cardiology consult Received 2 units PRBC for H&H of 8.1/24 Next day was transferred to larger facility References Elisha, S. (2011). Aortic Dissection. Case Studies in Nurse Anesthesia. 282285. Nagelhout, J.J., Plaus, K.L. & Rieker, M. (2014). Respiratory, Anatomy, Physiology, Pathophysiology & Anesthetic Management. Nurse Anesthesia. 653 Kasper, Dennis L. (2005). Harrison's Principles of Internal Medicine. Revised/Expanded ed. New York: McGraw-Hill, Medical Pub. Division. 23292330 Andropoulos, D., Stephen S., Isobel R., and Emad M. (2010). Anesthesia for Congenital Heart Disease. 2nd ed. Oxford: Blackwell. Coté and Lerman's a Practice of Anesthesia for Infants and Children. Revised/Expanded ed. Philadelphia, PA: Elsevier/Saunders, 2013. Bongard, F.S., and Darryl Y.S. (2008) Current Diagnosis & Treatment Critical Care. Revised/Expanded ed. New York: McGraw-Hill Medical. References Hall, J. (2005). Principles of critical care (Revised/Expanded ed.). New York: McGraw-Hill, Medical Pub. Division. Tintinalli, J. (2011). Tintinalli's emergency medicine: A comprehensive study guide (Revised/Expanded ed.). New York: McGraw-Hill. Marfan Foundation. (2013). What is Marfan Syndrome. Retrieved August 19, 2014, from http://www.marfan.org/about/marfan FBN1 gene. (2014, August 12).Genetics Home Refernce. Retrieved August 17, 2014, from http://ghr.nlm.nih.gov/gene/FBN1 Goland, S., & Elkayam, U. (2009). Cardiovascular Problems in Pregnant Women With Marfan Syndrome. Circulation, 619-623. References Hanumanthaiah, D. & Sudhir, V. (2013). Neuraxial block in a patient with dural ectasia. Indian Journal of Anaesthesia. 624-625 Bagirzadeh, L., Guglielminotti, J. & Loeys, B. (2013). Anesthesia recommendations for patients suffering from Marfan syndrome. Orphan Anesthesia. 2-8.