IRentrapment - University of Louisville Department of
advertisement

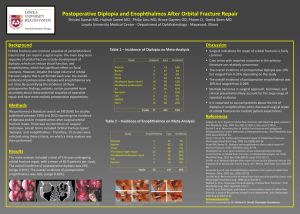
Grand Rounds Conference Lara Rosenwasser Newman, MD University of Louisville Department of Ophthalmology and Visual Sciences September 5, 2014 Subjective CC: Evaluate globe OS HPI: 6 yo African-American boy involved in a motor vehicle accident with waxing and waning consciousness. Pt complained of pain on eye movements, especially on upgaze. Denied diplopia. History PMHx: Asthma PSHx: Tympanostomy tube placement POHx: None Medications: Albuterol inhaler, Beclomethasone dipropionate (QVAR inhaler) Clinical Exam OD VA (n,sc/Allen): 20/30 OS 20/30 Pupils: 32 IOP: EOM: 32 (-)rAPD 19mmHg 20mmHg 0 -4 0 0 0 0 0 -3 Pain on attempted upgaze OS; no diplopia Clinical Exam PLE: External/Lids Conjunctiva/Sclera Cornea Anterior Chamber Iris Lens Vitreous Small superficial laceration on upper lid OS, mild ecchymosis/edema Clear/white; no subconj heme Clear OU Formed OU Normal OU Clear OU Normal OU DFE deferred per neurosurgery External Appearance Physical Exam Bradycardia with heart rate in 40s-50s Nausea, vomiting Waxing & waning consciousness since accident EOMs CT Face Minimally depressed fracture of L orbital floor Minor opacification of L ethmoid air cells, trace fluid or possibly hemorrhage in the L maxillary sinus Assessment 6 yo AAM status post motor vehicle accident with orbital floor fracture OS, with clinical exam suggestive of entrapment of inferior rectus muscle (WEBOF: white-eyed orbital blow-out fracture) Plan Admitted to ICU 2/2 bradycardia Ophthalmology: Patient taken to OR for fracture repair within ~6 hours of arrival to ED by oculoplastics L orbital floor fracture repair w/suprafoil implant Successful repositioning of orbital tissues Follow-up Post-operative day #1: 20/30 OD, 20/70 OS Improving periorbital edema, mild chemosis Diplopia Infraduction OS -1 DFE WNL Follow-up At 1 week: L face swollen No diplopia, intermittent pain “Trouble reading, covered 1 eye due to blurriness” Sinus arrhythmia – following with pediatrician Lower lid OS with decreased excursion 20/20 OU, motility full OU WEBOF: White-Eyed BlowOut Fracture Benign extraocular appearance w/minimal eyelid signs BUT w/significant EOM restriction Usually vertical gaze restriction Kids often do not complain of binocular diplopia (just close one eye) Cartilaginous/bendable bones in kids lead to: Increased risk for “trapdoor” fractures Increased risk for EOM incarceration WEBOF Presentation Kids may present w/severe oculocardiac reflex: Nausea or vomiting, dehydration from anorexia Bradycardia or syncope May be misdiagnosed as concussion Fracture/entrapment can be missed on CT head Always get dedicated CT face or orbits Imaging CT can show trapdoor fracture with rectus muscle incarceration or “missing” inferior rectus Inf rectus muscle belly “Missing” inf rectus Yano, H., Minagawa, T., Masuda, K., & Hirano, A. (2009). Urgent rescue of “missing rectus” in blowout fracture. Journal of Plastic, Reconstructive & Aesthetic Surgery : JPRAS, 62(9), e301–4. doi:10.1016/j.bjps.2007.12.041 Orbital Blow-out Fractures Symptoms: Pain on attempted eye movement Tenderness, lid edema, binocular diplopia, trauma hx Signs: Restricted EOMs, subcutaneous or conjunctival emphysema, point tenderness, enophthalmos Hypesthesia in distribution of the infraorbital nerve Byrne, Karen M. Infraorbital Nerve Block. Emedicine: http://emedicine.medscape.com/article/82660-overview Differential Diagnosis of Muscle Entrapment in Orbital Fractures Orbital edema and hemorrhage without blowout fracture Can still cause EOM limitation, swelling, ecchymosis Resolves over 7-10 days Cranial nerve palsy EOM limitation but no restriction on forced ductions Rule out intracranial & skull base processes w/CT WEBOF Treatment Consider broad-spectrum abx if hx of chronic sinusitis, diabetes, or immune compromise. Not mandatory Not evidence-based (limited, anecdotal evidence) Oxymetazoline BID for 3 days, no nose blowing Q1-2h ice packs for 20 mins for 24-28 hrs Consider oral steroids if swelling extensive and limiting exam of motility and globe position WEBOF Treatment Immediate repair (24-72 hrs) if evidence of muscle entrapment and non-resolving heart block, bradycardia, nausea, vomiting, or syncope Release incarcerated muscle to decrease chance of ischemia and fibrosis causing permanent restrictive strabismus Also to alleviate oculocardiac reflex Surgical Repair Technique Surgical approach: Subconjunctival incision +/- lateral cantholysis Elevate periorbita from orbital floor Release prolapsed tissue from fracture Usually place implant over fracture to prevent recurrent adhesions and tissue proplapse http://emedicine.medscape.com/article/882205-overview Balaji, S. M. (2013). Residual diplopia in treated orbital bone fractures. Annals of Maxillofacial Surgery, 3(1), 40–5. doi:10.4103/2231-0746.110078 Orbital Implants Alloplastic: Porous polyethylene Supramid (nylon foil) Gore-Tex Teflon Silicone sheet Titanium mesh Autogenous: Split cranial bone, iliac crest bone, or fascia http://emedicine.medscape.com/article/882205-overview#a3 Balaji, S. M. (2013). Residual diplopia in treated orbital bone fractures. Annals of Maxillofacial Surgery, 3(1), 40–5. doi:10.4103/2231-0746.110078 Timoney et al describe use of 0.4 mm Supramid Nylon foil – non-porous, relatively inert, alloplastic implant 59 orbits in 57 patients (all pediatric) 3 patients (5.3%) had entrapment with vasovagal responses and immediate intervention 6 had immediate post-op diplopia; all improved 2 post-op complications without permanent sequellae None had noticeable post-op enophthalmos Concluded Supramid implant safe and effective Timoney, P. J., Krakauer, M., Wilkes, B. N., Lee, H. B. H., & Nunery, W. R. (2014). Nylon foil (supramid) orbital implants in pediatric orbital fracture repair. Ophthalmic Plastic and Reconstructive Surgery, 30(3), 212–4. doi:10.1097/IOP.0000000000000051 http://www.ophthalmologyweb.com/Oculoplastic-and-Orbital-Procedures/5561-Supramid-Sheet-Implants/ References 1. 2. 3. 4. 5. 6. 7. 8. Balaji, S. M. (2013). Residual diplopia in treated orbital bone fractures. Annals of Maxillofacial Surgery, 3(1), 40–5. doi:10.4103/2231-0746.110078 Foulds, J. S., Laverick, S., & MacEwen, C. J. (2013). “White-eyed” blowout fracture in children. Emergency Medicine Journal : EMJ, 30(10), 836. doi:10.1136/emermed-2012-201741 Gerstenblith, A. T., & Rabinowitz, M. P. (2012). The Wills Eye Manual: Office and Emergency Room Diagnosis and Treatment of Eye Disease. Philadelphia, PA: Lippincott Williams & Wilkins. Hammond, D., Grew, N., & Khan, Z. (2013). The white-eyed blowout fracture in the child: beware of distractions. Journal of Surgical Case Reports, 2013(7), 2–3. doi:10.1093/jscr/rjt054 Orbital Trauma. In: Basic and Clinical Science Course (BCSC) Section 7: Orbit, Eyelids, and Lacrimal System. San Francisco, CA: American Academy of Ophthalmology; 2014: 100-104. Timoney, P. J., Krakauer, M., Wilkes, B. N., Lee, H. B. H., & Nunery, W. R. (2014). Nylon foil (supramid) orbital implants in pediatric orbital fracture repair. Ophthalmic Plastic and Reconstructive Surgery, 30(3), 212–4. doi:10.1097/IOP.0000000000000051 Verret, Daniel JDucic, Y. (2013). Implants, Soft Tissue, High-Density Porous Polyethylene (Medpor). Medscape Reference. Retrieved from http://emedicine.medscape.com/article/882205overview#a3 Yano, H., Minagawa, T., Masuda, K., & Hirano, A. (2009). Urgent rescue of “missing rectus” in blowout fracture. Journal of Plastic, Reconstructive & Aesthetic Surgery : JPRAS, 62(9), e301–4. doi:10.1016/j.bjps.2007.12.041